GI physiology (digestion, absorption, motility)

On this page
🏗️ The Digestive Engine: Architectural Mastery
Every meal you eat triggers a precisely choreographed cascade spanning 30 feet of tissue, dozens of enzymes, and multiple organ systems working in concert to transform food into fuel. This lesson will guide you through the architectural brilliance of the GI tract, the enzymatic precision that breaks down nutrients, the selective absorption mechanisms that capture what your body needs, and the clinical reasoning to diagnose when this system fails. You'll master the pathophysiology behind malabsorption syndromes, learn treatment algorithms that restore function, and understand how the gut communicates with distant organs to regulate metabolism, immunity, and even cognition.
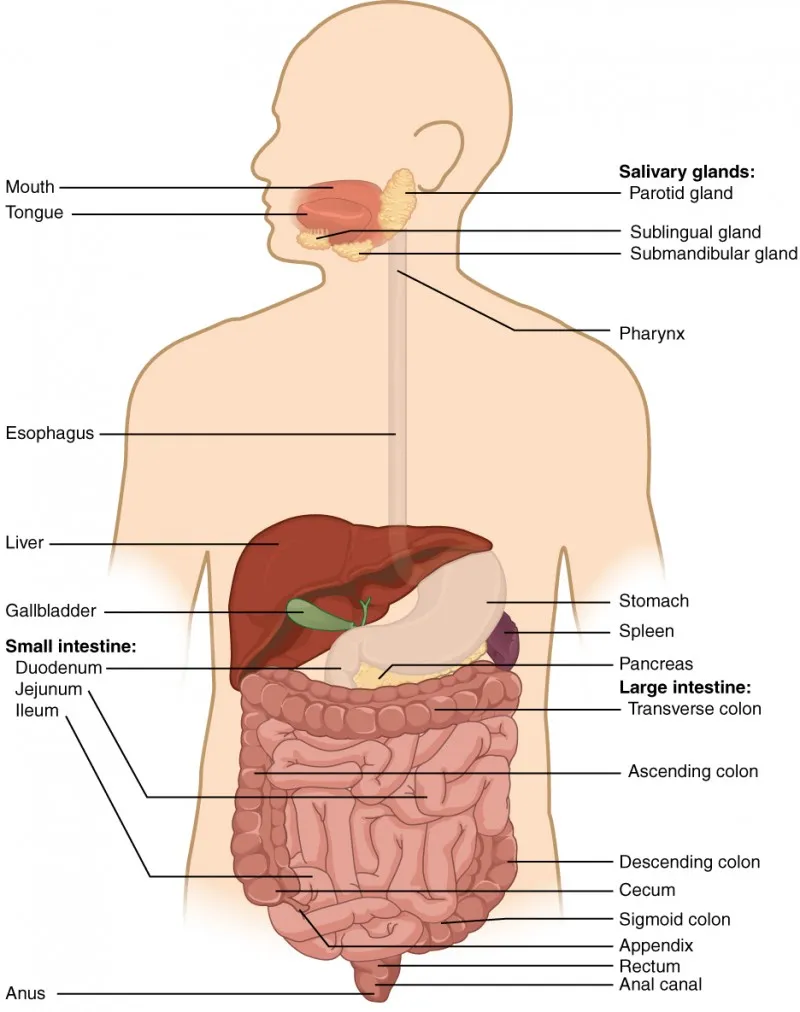
The digestive system operates as three integrated subsystems: mechanical processing (motility patterns), chemical breakdown (enzymatic cascades), and selective absorption (membrane transport). Each subsystem maintains strict temporal coordination-gastric emptying occurs every 90-120 minutes during fasting, pancreatic enzyme release peaks within 30 minutes of meal ingestion, and colonic transit requires 12-48 hours for complete processing.
📌 Remember: MASH for GI system organization - Motility (movement patterns), Absorption (nutrient uptake), Secretion (enzyme/acid release), Hormonal regulation (chemical messengers). Each component operates with 95%+ efficiency in healthy individuals.
-
Motility Coordination
- Gastric contractions: 3 waves/minute (basic electrical rhythm)
- Small bowel: 11-12 contractions/minute in duodenum, 8-9/minute in ileum
- Colonic mass movements: 3-4 episodes/day with 200-300 mmHg pressure
- Migrating motor complexes (MMC): 90-120 minute cycles during fasting
- Fed state: 4-6 hour digestive periods with coordinated segmentation
-
Secretory Precision
- Daily fluid production: 8-10 liters total (2L saliva, 2.5L gastric, 1.5L bile, 2.5L pancreatic, 1L small bowel)
- Gastric acid: 1-3 liters/day at pH 1.5-2.0 (0.16M HCl)
- Pancreatic bicarbonate: 120-300 mEq/day neutralizing 40-60 mEq gastric acid hourly
⭐ Clinical Pearl: 95% of GI fluid is reabsorbed-small bowel absorbs 8-9 liters/day, colon handles 1-2 liters/day. When this fails, 500mL excess fluid causes diarrhea, 1000mL+ causes severe dehydration requiring immediate intervention.
| GI Segment | Length | Surface Area | Primary Function | Transit Time | Absorption Capacity |
|---|---|---|---|---|---|
| Stomach | 25cm | 0.1 m² | Acid/pepsin secretion | 1-4 hours | Minimal (alcohol, some drugs) |
| Duodenum | 25cm | 2 m² | Neutralization/mixing | 30 minutes | Iron, calcium, folate |
| Jejunum | 2.5m | 100 m² | Major nutrient absorption | 2-3 hours | 80% nutrients, water |
| Ileum | 3.5m | 60 m² | B12, bile salts | 3-4 hours | Vitamin B12, bile acids |
| Colon | 1.5m | 2 m² | Water/electrolyte recovery | 12-48 hours | 1-2L water, sodium |
This architectural foundation enables the sophisticated chemical processing and transport mechanisms that follow, where enzymatic precision meets membrane selectivity to achieve 99%+ absorption efficiency for essential nutrients.
🏗️ The Digestive Engine: Architectural Mastery
⚙️ The Chemical Orchestra: Enzymatic Command Center
- Gastric Enzymatic Environment
- Pepsinogen activation: pH < 2.0 required for pepsin formation
- Gastric lipase: 10-15% of total fat digestion (optimal pH 4.0-6.0)
- Intrinsic factor: 2-3 mg/day for vitamin B12 binding (1000:1 binding ratio)
- Pepsin cleaves 15-20% of peptide bonds (preferentially aromatic amino acids)
- Gastric emptying: 50% liquid phase in 30 minutes, 50% solid phase in 90 minutes
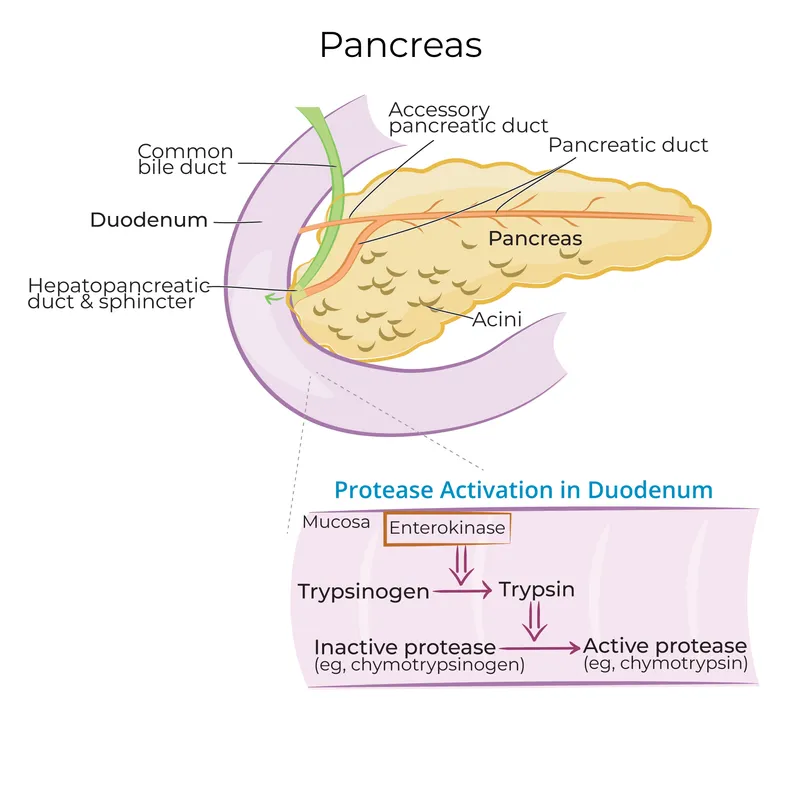
📌 Remember: PACE for pancreatic enzyme activation - Pancreatic duct delivery, Alkaline environment (pH 8+), CCK stimulation, Enterokinase triggers trypsinogen→trypsin conversion. Trypsin then activates all other pancreatic zymogens in cascade fashion.
- Pancreatic Enzyme Arsenal
- Proteases: Trypsin, chymotrypsin, elastase (25-30g/day protein capacity)
- Lipases: Pancreatic lipase (150g/day fat capacity), phospholipase A2, cholesterol esterase
- Carbohydrases: α-amylase (300-400g/day starch capacity)
- Trypsin specificity: cleaves after basic amino acids (lysine, arginine)
- Chymotrypsin specificity: cleaves after aromatic amino acids (phenylalanine, tyrosine, tryptophan)
- Pancreatic lipase: requires colipase and bile salts for optimal activity
| Enzyme Class | Location | Substrate | Products | Clinical Significance | Deficiency Prevalence |
|---|---|---|---|---|---|
| Disaccharidases | Brush border | Lactose, sucrose, maltose | Monosaccharides | Lactose intolerance | 65% global population |
| Peptidases | Brush border | Di/tripeptides | Amino acids | Protein malabsorption | <1% population |
| Nucleases | Pancreatic | DNA/RNA | Nucleotides | Rare deficiencies | <0.1% population |
| Lipases | Pancreatic | Triglycerides | Fatty acids + glycerol | Steatorrhea | 1-2% population |
| Proteases | Pancreatic | Proteins | Peptides | Protein maldigestion | 1-3% population |
💡 Master This: The brush border contains >20 different enzymes with 3-5 day turnover, making it vulnerable to any condition affecting enterocyte renewal. Viral gastroenteritis, celiac disease, and chemotherapy all impair brush border function, causing secondary disaccharidase deficiencies.
This enzymatic precision creates the molecular fragments ready for the sophisticated transport systems that achieve near-perfect absorption efficiency across the intestinal barrier.
⚙️ The Chemical Orchestra: Enzymatic Command Center
🎯 Pattern Recognition: The Absorption Matrix
- Duodenal Absorption Specialists
- Iron: 1-2 mg/day absorbed from 10-15 mg dietary intake (10-15% efficiency)
- Calcium: 200-400 mg/day absorbed (vitamin D-dependent, 30-40% efficiency)
- Folate: 400-800 μg/day absorbed (jejunal backup available)
- Iron absorption increases 3-5 fold in deficiency states
- Calcium absorption decreases to 10-15% in vitamin D deficiency
- Heme iron: 15-35% absorbed vs non-heme iron: 2-20% absorbed
📌 Remember: DIME for duodenal absorption - Divalent cations (Ca²⁺, Fe²⁺, Mg²⁺), Iron (heme and non-heme), Minerals (zinc, copper), Early vitamins (thiamine, riboflavin). Duodenal pH 6.0-7.0 optimizes divalent cation solubility.
-
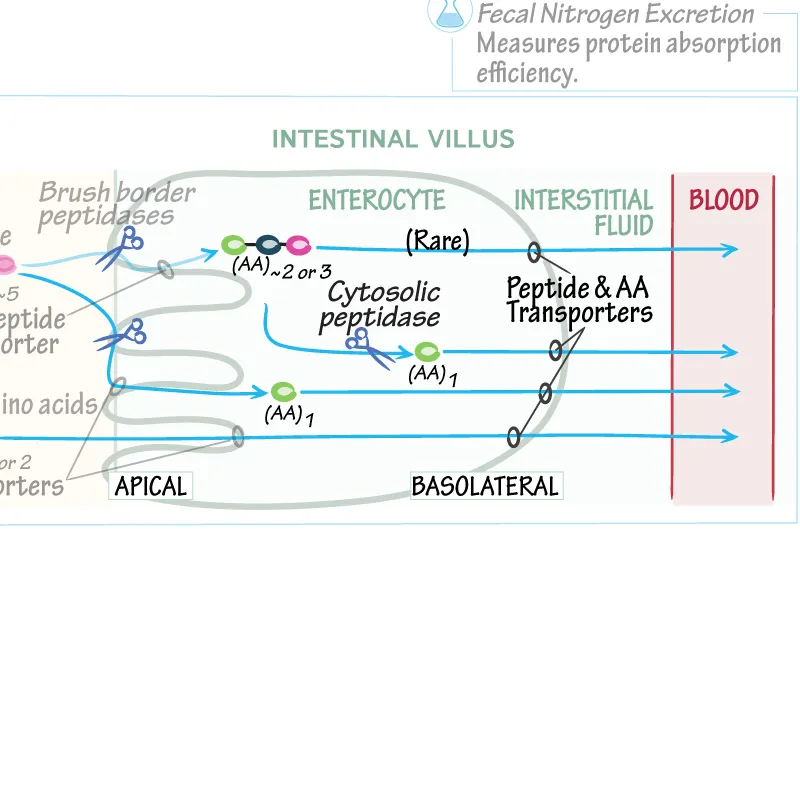
Jejunal Absorption Powerhouse
- Glucose: 300-400g/day capacity via SGLT1 (sodium-coupled)
- Amino acids: 100-150g/day via multiple transporters (sodium-dependent)
- Fat-soluble vitamins: A, D, E, K via chylomicron incorporation
- SGLT1 transporter: 2 Na⁺ : 1 glucose stoichiometry
- Amino acid transporters: >15 different systems with overlapping specificity
- Chylomicron formation: >48 hours for complete clearance
-
Ileal Absorption Specialists
- Vitamin B12: 1-3 μg/day via intrinsic factor complex (highly specific)
- Bile salts: 95% reabsorption (20-30g/day enterohepatic circulation)
- Fat-soluble vitamins: backup absorption site
- B12-intrinsic factor complex: cubilin receptor-mediated endocytosis
- Bile salt transporter (IBAT): sodium-dependent, 95%+ efficiency
- Enterohepatic circulation: 6-12 cycles/day for bile salts
⭐ Clinical Pearl: Terminal ileal resection >100 cm causes vitamin B12 deficiency (appears in 2-5 years) and bile acid malabsorption (immediate diarrhea). Cholestyramine treats bile acid diarrhea but worsens fat-soluble vitamin deficiency.
| Transport Type | Energy Source | Selectivity | Capacity | Clinical Examples | Saturation Point |
|---|---|---|---|---|---|
| Active (SGLT1) | ATP/Na⁺ gradient | High | 400g glucose/day | Glucose-galactose malabsorption | 60-80g/hour |
| Facilitated (GLUT2) | Concentration gradient | Moderate | Unlimited | Fructose absorption | Non-saturable |
| Coupled (PepT1) | H⁺ gradient | Low | 150g protein/day | Hartnup disease | 20-30g/hour |
| Passive diffusion | Concentration gradient | Very low | Variable | Fat-soluble vitamins | Non-saturable |
| Receptor-mediated | ATP | Very high | Limited | B12-IF complex | 1-3 μg/day |
These absorption patterns create the foundation for understanding malabsorption syndromes and designing targeted nutritional interventions based on anatomical precision.
🎯 Pattern Recognition: The Absorption Matrix
🔬 Diagnostic Precision: The Malabsorption Detective
- Fat Malabsorption Patterns
- Pancreatic insufficiency: >15g stool fat/day, normal D-xylose
- Small bowel disease: 7-15g stool fat/day, abnormal D-xylose
- Bile acid deficiency: moderate steatorrhea, normal pancreatic enzymes
- Coefficient of fat absorption: >95% normal, <90% abnormal
- Pancreatic elastase: <200 μg/g stool indicates severe insufficiency
- Fecal chymotrypsin: <3 U/g stool suggests pancreatic disease
📌 Remember: SPADE for steatorrhea causes - Small bowel disease (celiac, Crohn's), Pancreatic insufficiency (chronic pancreatitis, CF), Absent bile (cholestasis, ileal resection), Drugs (orlistat, cholestyramine), Endocrine (hyperthyroidism, diabetes). Each has distinct laboratory patterns.
-
Carbohydrate Malabsorption Testing
- Lactose tolerance test: <20 mg/dL glucose rise indicates lactase deficiency
- Hydrogen breath test: >20 ppm rise indicates bacterial fermentation
- Stool pH: <5.5 suggests carbohydrate malabsorption
- Breath hydrogen: peaks 90-180 minutes after lactose load
- Stool reducing substances: >0.5% indicates sugar malabsorption
- Osmotic gap: >125 mOsm/kg suggests osmotic diarrhea
-
Protein Malabsorption Assessment
- Fecal α1-antitrypsin: >54 mg/dL indicates protein-losing enteropathy
- Serum albumin: <3.5 g/dL with normal liver function
- Fecal nitrogen: >2.5g/day indicates protein malabsorption
- α1-antitrypsin clearance: >27 mL/day abnormal
- Fecal elastase: distinguishes pancreatic from intestinal causes
- Serum trypsinogen: <20 ng/mL indicates severe pancreatic insufficiency
⭐ Clinical Pearl: Bacterial overgrowth causes early breath hydrogen peak (<90 minutes) vs distal malabsorption causes late peak (>120 minutes). Antibiotic treatment normalizes early but not late peaks.
| Condition | Stool Fat | D-xylose | B12 Absorption | Folate Level | Diagnostic Clue |
|---|---|---|---|---|---|
| Celiac disease | 7-15g/day | Abnormal | Normal | Low | Anti-tTG positive |
| Pancreatic insufficiency | >15g/day | Normal | Normal | Normal | Low fecal elastase |
| Bacterial overgrowth | 5-10g/day | Abnormal | Low | High | Early H2 peak |
| Crohn's disease | Variable | Abnormal | Low (if ileal) | Low | Inflammatory markers |
| Tropical sprue | 10-20g/day | Abnormal | Low | Low | Geographic history |
This diagnostic framework enables precise localization of GI dysfunction and guides targeted therapeutic interventions based on pathophysiological mechanisms.
🔬 Diagnostic Precision: The Malabsorption Detective
⚕️ Therapeutic Mastery: The Treatment Algorithm
- Pancreatic Enzyme Replacement Therapy
- Dosing: 25,000-50,000 units lipase per meal, 10,000-25,000 per snack
- Timing: with first bite of food for optimal mixing
- Monitoring: coefficient of fat absorption >85%, weight stabilization
- Enteric-coated preparations: pH >5.5 for capsule dissolution
- Dose titration: increase by 25,000 units if steatorrhea persists
- Maximum dose: 2,500 units lipase/kg/meal (fibrosing colonopathy risk)
📌 Remember: PERT principles - PH-resistant coating, Early administration (with food), Regular monitoring (fat absorption), Titration based on symptoms. Acid suppression with PPI improves enzyme stability and efficacy.
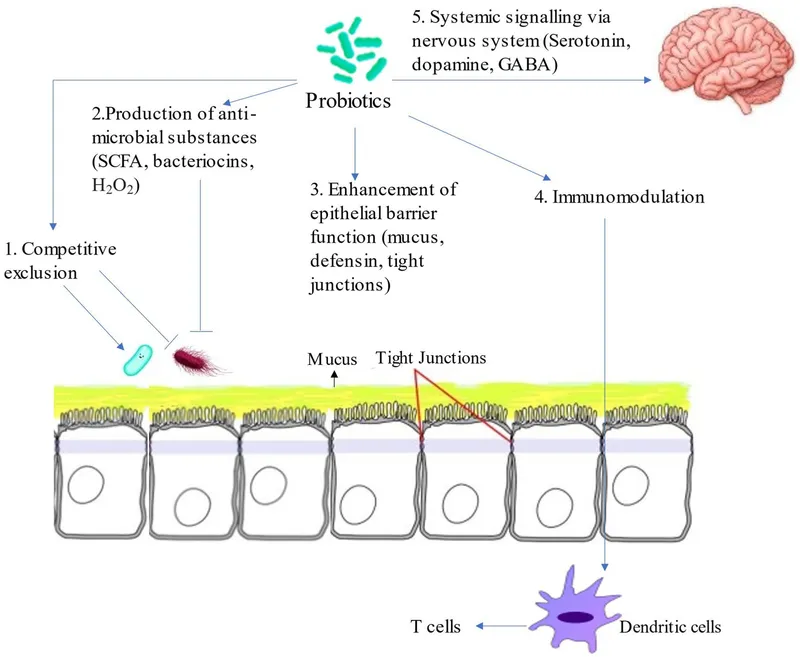
- Probiotic Therapeutic Protocols
- Lactobacillus rhamnosus GG: 10¹⁰ CFU/day for antibiotic-associated diarrhea
- Saccharomyces boulardii: 250-500mg twice daily for C. difficile prevention
- Multi-strain formulations: >4 species, >10⁹ CFU for IBS management
- Treatment duration: minimum 4 weeks for microbiome modulation
- Refrigeration: maintains viability for freeze-dried preparations
- Antibiotic spacing: 2-3 hours separation to prevent probiotic killing
- Nutritional Intervention Strategies
- Fat-soluble vitamins: A (25,000 IU), D (50,000 IU), E (400 IU), K (10mg) weekly
- Medium-chain triglycerides: 15-30g/day for fat malabsorption
- Elemental formulas: amino acids + simple sugars for severe malabsorption
- Water-miscible vitamin preparations: better absorption in steatorrhea
- MCT oil: absorbed directly into portal circulation (bypasses lymphatic system)
- Elemental diets: 90%+ absorption even with severe small bowel disease
⭐ Clinical Pearl: Zinc deficiency occurs in 80% of patients with chronic diarrhea. Zinc supplementation (20-40mg/day) reduces diarrhea duration by 25% and stool volume by 30% in acute gastroenteritis.
| Therapeutic Class | Mechanism | Dosing | Monitoring | Success Rate | Time to Effect |
|---|---|---|---|---|---|
| Pancreatic enzymes | Replace lipase/protease | 25,000-50,000 U/meal | Stool fat, weight | 85-95% | 1-2 weeks |
| Bile acid sequestrants | Bind excess bile acids | 4-8g before meals | Stool frequency | 70-80% | 3-7 days |
| Probiotics | Microbiome restoration | 10⁹-10¹¹ CFU/day | Symptom scores | 60-75% | 2-4 weeks |
| Prokinetics | Enhance motility | Varies by agent | Gastric emptying | 65-85% | 1-3 days |
| Anti-spasmodics | Reduce cramping | PRN dosing | Pain scores | 70-80% | 30-60 minutes |
This therapeutic precision enables restoration of normal GI function and prevention of long-term nutritional complications through evidence-based interventions.
⚕️ Therapeutic Mastery: The Treatment Algorithm
🌐 Systems Integration: The Gut-Body Network
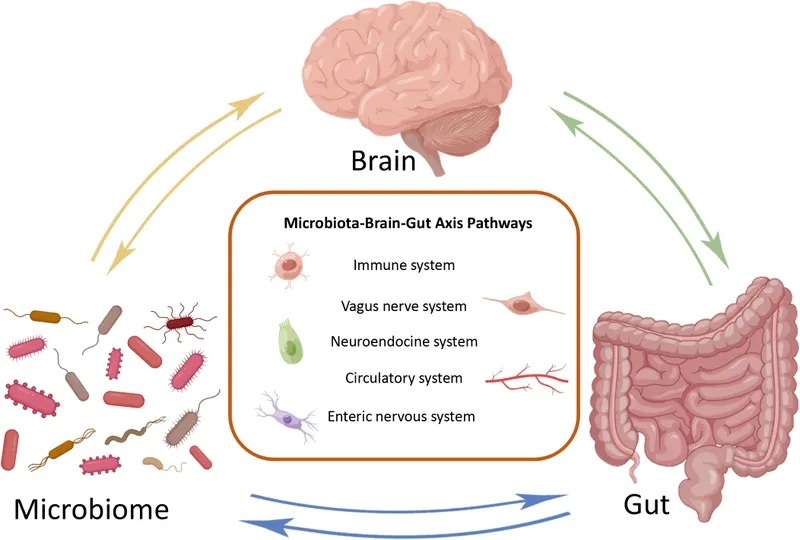
- Enteric Nervous System Architecture
- Myenteric plexus: motility control between muscle layers
- Submucosal plexus: secretion and blood flow regulation
- Neurotransmitters: >30 different types (acetylcholine, serotonin, VIP, substance P)
- Intrinsic neurons: 500 million total (5x more than spinal cord)
- Reflex circuits: complete function without CNS input
- Plasticity: neurogenesis continues throughout adult life
📌 Remember: GUTS for enteric nervous system - Gut has own brain (500M neurons), Unique neurotransmitters (>30 types), Two-way communication (gut↔brain), Serotonin central (95% body total). ENS dysfunction causes functional GI disorders in 15-20% population.
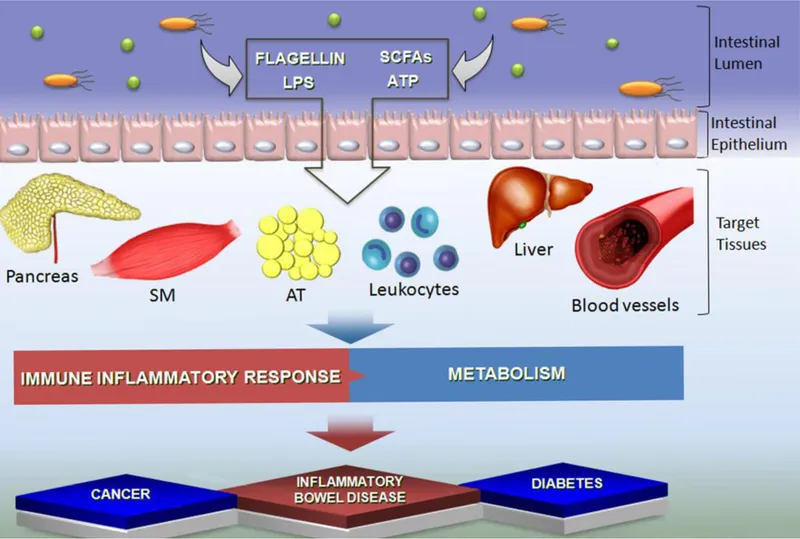
- Microbiome-Host Integration
- Bacterial density: 10¹¹-10¹² CFU/g in colon (highest in body)
- Metabolite production: short-chain fatty acids (60-70% colonic energy)
- Immune modulation: 70% of immune cells in gut-associated lymphoid tissue
- Firmicutes:Bacteroidetes ratio: healthy 3:1, obesity >10:1
- SCFA production: butyrate (colonocyte fuel), propionate (gluconeogenesis), acetate (lipogenesis)
- Barrier function: tight junction regulation via microbial metabolites
- Hormonal Integration Networks
- GLP-1: incretin effect (50-70% postprandial insulin response)
- Ghrelin: hunger signaling (peaks before meals, suppressed postprandially)
- Leptin: satiety signaling (adipose-derived, hypothalamic target)
- GLP-1 half-life: 1-2 minutes (rapid DPP-4 degradation)
- Ghrelin levels: increase 200-300% before meals
- Leptin resistance: obesity-associated, inflammatory-mediated
⭐ Clinical Pearl: Antibiotic exposure reduces microbiome diversity for 6-12 months, increasing C. difficile risk 10-fold and metabolic dysfunction risk 2-3 fold. Probiotic co-administration reduces antibiotic-associated diarrhea by 60-70%.
| Integration System | Key Components | Signaling Range | Response Time | Clinical Relevance | Dysfunction Prevalence |
|---|---|---|---|---|---|
| Gut-Brain Axis | Vagus, ENS, hormones | Bidirectional | Seconds-hours | IBS, depression | 15-20% population |
| Microbiome-Host | SCFA, metabolites | Local-systemic | Hours-days | Immunity, metabolism | Variable |
| Incretin System | GLP-1, GIP | Endocrine | Minutes | Diabetes, obesity | 5-10% population |
| Barrier Function | Tight junctions | Local | Minutes-hours | Inflammation, allergy | 10-15% population |
| Circadian Rhythm | Clock genes, feeding | 24-hour cycles | Hours | Metabolic syndrome | 20-30% population |
This systems integration reveals how GI physiology extends far beyond digestion to influence metabolism, immunity, mood, and overall health through sophisticated communication networks.
🌐 Systems Integration: The Gut-Body Network
🎯 Clinical Mastery: The Rapid Assessment Arsenal
📌 Remember: RED FLAGS for GI emergencies - Rectal bleeding (>50mL), Emergent weight loss (>10% in 6 months), Dysphagia (progressive), Family history (cancer <50 years), Lymphadenopath, Anemia (unexplained), Guarding/rigidity, Severe pain (>8/10). Any red flag requires urgent evaluation within 24-48 hours.
- Rapid Diagnostic Framework
- Acute abdomen: <6 hours pain, peritoneal signs, hemodynamic instability
- GI bleeding: hemoglobin drop >2g/dL, orthostatic changes, melena/hematochezia
- Functional disorders: >6 months symptoms, normal investigations, Rome IV criteria
- Acute abdomen mortality: 5-15% if delayed diagnosis >12 hours
- Upper GI bleeding: 80% stop spontaneously, 20% require intervention
- Functional disorders: affect 25% population, account for 50% GI consultations
⭐ Clinical Pearl: Fecal calprotectin revolutionizes IBD monitoring-<50 μg/g indicates remission, 50-250 μg/g suggests mild inflammation, >250 μg/g indicates active disease requiring treatment escalation. Serial monitoring predicts relapse 2-3 months before clinical symptoms.
| Clinical Tool | Sensitivity | Specificity | Clinical Application | Time to Result | Cost-Effectiveness |
|---|---|---|---|---|---|
| Fecal calprotectin | 95% | 90% | IBD vs IBS differentiation | Same day | High |
| Rome IV criteria | 85% | 85% | Functional disorder diagnosis | Immediate | Very high |
| Alarm symptoms | 90% | 70% | Organic disease screening | Immediate | Very high |
| H. pylori stool antigen | 95% | 95% | Active infection detection | 1-2 days | High |
| Fecal elastase | 90% | 85% | Pancreatic insufficiency | 1-2 days | Moderate |
This clinical mastery framework enables rapid, accurate assessment of GI disorders while optimizing resource utilization and patient outcomes through evidence-based decision-making tools.
🎯 Clinical Mastery: The Rapid Assessment Arsenal
Practice Questions: GI physiology (digestion, absorption, motility)
Test your understanding with these related questions
A 25-year-old male presents to his primary care physician for fatigue, abdominal pain, diarrhea, and weight loss. He states that this issue has occurred throughout his life but seems to “flare up” on occasion. He states that his GI pain is relieved with defecation, and his stools are frequent, large, and particularly foul-smelling. The patient has a past medical history of an ACL tear, as well as a car accident that resulted in the patient needing a transfusion and epinephrine to treat transfusion anaphylaxis. His current medications include vitamin D and ibuprofen. He recently returned from a camping trip in the eastern United States. He states that on the trip they cooked packed meats over an open fire and obtained water from local streams. His temperature is 99.5°F (37.5°C), blood pressure is 120/77 mmHg, pulse is 70/min, respirations are 11/min, and oxygen saturation is 98% on room air. Physical exam reveals poor motor control and an ataxic gait on neurologic exam. Cardiac and pulmonary exams are within normal limits. Laboratory studies are ordered and return as below: Hemoglobin: 9.0 g/dL Hematocrit: 25% Haptoglobin: 12 mg/dL Leukocyte count: 7,500 cells/mm^3 with normal differential Platelet count: 255,000/mm^3 Serum: Na+: 140 mEq/L Cl-: 102 mEq/L K+: 5.0 mEq/L HCO3-: 24 mEq/L BUN: 24 mg/dL Glucose: 82 mg/dL Creatinine: 1.0 mg/dL Ca2+: 9.0 mg/dL LDH: 457 U/L AST: 11 U/L ALT: 11 U/L Radiography is ordered which reveals a stress fracture in the patient’s left tibia. Which of the following is the best confirmatory test for this patient’s condition?













