DKA

On this page
🔥 The Metabolic Crisis: When Sugar Becomes Acid
Diabetic ketoacidosis transforms the body into a paradox: cells starve while glucose floods the bloodstream, triggering a cascade that turns fat into toxic acids. You'll master why this metabolic emergency unfolds, how to recognize its distinctive clinical fingerprint, and the systematic approach to reverse life-threatening acidosis while avoiding dangerous pitfalls. This lesson builds your diagnostic precision to distinguish DKA from its mimics and your therapeutic confidence to orchestrate fluid resuscitation, insulin therapy, and electrolyte correction in the right sequence.
The classic DKA triad creates a perfect storm of metabolic dysfunction. Hyperglycemia >250 mg/dL floods the bloodstream while cells starve for glucose. Ketosis >3 mmol/L produces alternative fuel that acidifies the blood. Metabolic acidosis with pH <7.30 triggers compensatory hyperventilation and electrolyte chaos.
📌 Remember: DKA GAP - Dehydration, Ketosis, Acidosis create the Glucose Acid Paradox where sugar becomes poison
- Severe DKA: pH <7.00, bicarbonate <10 mEq/L, altered mental status
- Mortality risk: 5-10% with aggressive management
- ICU admission mandatory for continuous monitoring
- Hourly glucose, electrolytes, arterial blood gases
- Cardiac monitoring for arrhythmias from K+ shifts
- Moderate DKA: pH 7.00-7.24, bicarbonate 10-15 mEq/L
- Hospital admission required, ICU consideration
- Response to treatment within 6-12 hours expected
- Mild DKA: pH 7.25-7.30, bicarbonate 15-18 mEq/L
- Ward management acceptable with close monitoring
- Resolution typically within 12-18 hours
| Severity | pH Range | HCO3- (mEq/L) | Anion Gap | Mental Status | Mortality Risk |
|---|---|---|---|---|---|
| Mild | 7.25-7.30 | 15-18 | >10 | Alert | <1% |
| Moderate | 7.00-7.24 | 10-15 | >12 | Alert/Drowsy | 1-5% |
| Severe | <7.00 | <10 | >12 | Stupor/Coma | 5-10% |
| Cerebral Edema | Variable | Variable | Variable | Altered/Coma | 20-90% |
| Mixed DKA/HHS | >7.30 | >15 | >12 | Variable | 5-15% |

The anion gap elevation reveals the hidden acid load. Normal anion gap 8-12 mEq/L jumps to >20 mEq/L in severe DKA as ketoacids accumulate. Beta-hydroxybutyrate and acetoacetate create the gap while lactate may contribute in severe dehydration.
💡 Master This: Every 1 mEq/L bicarbonate drop corresponds to approximately 10 mg/dL glucose rise and 0.02 pH decrease. This relationship predicts severity and guides intervention timing.
Understanding DKA's metabolic cascade unlocks the logic behind every treatment decision, from fluid resuscitation priorities to insulin timing protocols.
🔥 The Metabolic Crisis: When Sugar Becomes Acid
⚡ The Biochemical Storm: Cellular Starvation Amidst Abundance
Counter-regulatory hormones create the perfect metabolic storm. Glucagon stimulates hepatic glucose production, increasing levels 300-500% above normal. Cortisol promotes protein breakdown and gluconeogenesis. Catecholamines enhance lipolysis and insulin resistance. Growth hormone amplifies all effects.
📌 Remember: CAGE Hormones - Cortisol, Adrenaline, Glucagon, Epinephrine create the metabolic CAGE that traps patients in DKA
- Ketogenesis Pathway: Accelerated lipolysis overwhelms normal fat oxidation
- Free fatty acid levels increase 5-10 fold above normal
- Hepatic ketone production reaches 300-500 mg/dL/hour
- Beta-hydroxybutyrate: 70% of total ketones
- Acetoacetate: 25% of total ketones
- Acetone: 5% (causes fruity breath odor)
- Osmotic Effects: Glucose acts as osmotic diuretic
- Every 100 mg/dL glucose elevation increases serum osmolality by 5.6 mOsm/kg
- Fluid losses reach 100-200 mL/kg body weight
- Electrolyte depletion: K+ 3-5 mEq/kg, PO4 1-1.5 mmol/kg
| Metabolic Parameter | Normal Range | Mild DKA | Moderate DKA | Severe DKA | Critical Threshold |
|---|---|---|---|---|---|
| Glucose (mg/dL) | 70-100 | 250-350 | 350-500 | 500-800 | >800 (HHS risk) |
| Ketones (mmol/L) | <0.6 | 3-5 | 5-8 | >8 | >10 (severe) |
| Anion Gap | 8-12 | 15-20 | 20-25 | >25 | >30 (extreme) |
| Osmolality (mOsm/kg) | 280-295 | 300-320 | 320-340 | >340 | >350 (coma risk) |
| Fluid Deficit (L) | 0 | 3-5 | 5-8 | 8-12 | >12 (shock) |
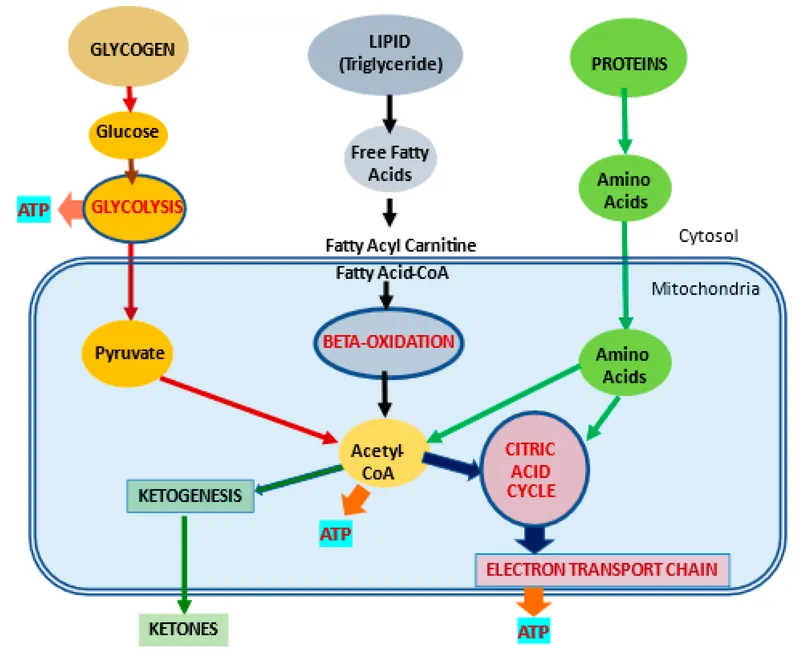
The acid-base disruption creates cascading physiological compensation. Metabolic acidosis triggers respiratory compensation with Kussmaul breathing - deep, rapid respirations attempting to blow off CO2. Renal compensation fails as dehydration impairs kidney function.
💡 Master This: The anion gap directly correlates with ketone concentration. Every 1 mmol/L increase in ketones raises the anion gap by approximately 1-2 mEq/L, providing rapid severity assessment.
Understanding these interconnected pathways reveals why DKA treatment requires simultaneous correction of multiple metabolic derangements rather than isolated glucose management.
⚡ The Biochemical Storm: Cellular Starvation Amidst Abundance
🎯 The Clinical Detective: Recognizing DKA's Signature Patterns
Recognition patterns follow the "4 P's plus" framework. Polyuria from osmotic diuresis, polydipsia from dehydration, polyphagia from cellular starvation, profound fatigue from metabolic dysfunction. Advanced cases add nausea/vomiting (75% of patients), abdominal pain (30% of patients), and altered mental status (25% of severe cases).
📌 Remember: DKA FAST - Dehydration signs, Kussmaul breathing, Abdomen pain, Fruity breath, Altered mental status, Sick appearance, Tachycardia
-
Physical Examination Priorities:
- Dehydration assessment: skin turgor, mucous membranes, orthostatic vitals
- Mild: 5% dehydration, normal skin turgor
- Moderate: 5-10% dehydration, delayed skin recoil
- Severe: >10% dehydration, tenting, dry mucosa
- Respiratory pattern: Kussmaul breathing in >80% of moderate-severe cases
- Neurological status: Glasgow Coma Scale correlation with pH
- pH >7.20: typically alert and oriented
- pH 7.00-7.20: drowsy but arousable
- pH <7.00: stuporous or comatose
- Dehydration assessment: skin turgor, mucous membranes, orthostatic vitals
-
Diagnostic Mimics Requiring Differentiation:
- Hyperosmolar hyperglycemic state (HHS): glucose >600 mg/dL, minimal ketosis
- Alcoholic ketoacidosis: history of alcohol use, normal glucose
- Starvation ketosis: mild ketosis, normal anion gap
- Salicylate poisoning: mixed acid-base disorder, altered mental status
- Methanol/ethylene glycol: severe anion gap, visual symptoms
| Clinical Feature | DKA Frequency | Severity Correlation | Diagnostic Value | Alternative Diagnosis |
|---|---|---|---|---|
| Polyuria/Polydipsia | 85-95% | Early symptom | High sensitivity | Diabetes insipidus |
| Nausea/Vomiting | 70-80% | Moderate-severe | Moderate | Gastroenteritis |
| Abdominal Pain | 25-35% | Variable | Low specificity | Acute abdomen |
| Kussmaul Breathing | 80-90% | pH <7.25 | High specificity | Respiratory alkalosis |
| Fruity Breath | 40-60% | Ketone level | Moderate | Alcoholic ketoacidosis |
The diagnostic triad requires laboratory confirmation, but clinical suspicion drives immediate management. Point-of-care glucose >250 mg/dL plus urine ketones >2+ or serum ketones >3 mmol/L with clinical presentation justifies empirical treatment while awaiting arterial blood gas results.
💡 Master This: Serum ketones >3 mmol/L provide more accurate assessment than urine ketones, which may remain positive for 24-48 hours after resolution. Beta-hydroxybutyrate measurement enables precise monitoring of treatment response.
Mastering these recognition patterns enables rapid DKA identification while avoiding diagnostic pitfalls that delay life-saving interventions.
🎯 The Clinical Detective: Recognizing DKA's Signature Patterns
⚖️ The Differential Maze: Distinguishing DKA from Metabolic Mimics
- Primary Differential Categories:
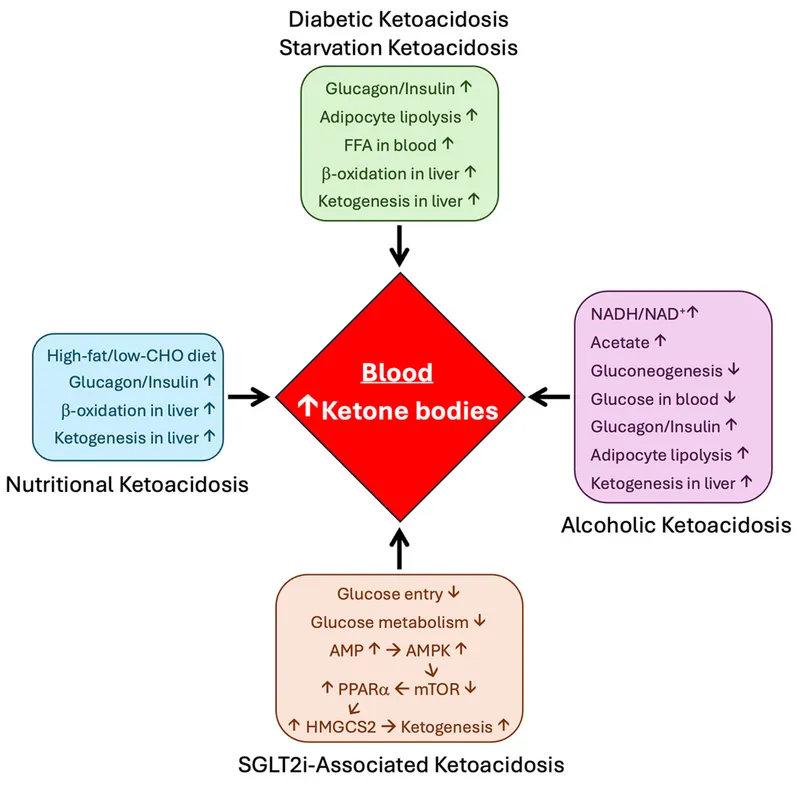
- Ketotic States: Alcoholic ketoacidosis, starvation ketosis, medication-induced
- Alcoholic ketoacidosis: normal glucose, elevated ketones, alcohol history
- Starvation ketosis: mild ketosis (<5 mmol/L), normal pH, prolonged fasting
- SGLT2 inhibitor ketosis: euglycemic DKA, recent medication use
- Non-Ketotic Acidosis: Lactic acidosis, uremic acidosis, toxic ingestions
- Lactic acidosis: elevated lactate >4 mmol/L, tissue hypoperfusion
- Uremic acidosis: chronic kidney disease, BUN >100 mg/dL
- Toxic ingestions: methanol, ethylene glycol, salicylates
- Mixed Disorders: DKA/HHS overlap, concurrent conditions
- Mixed DKA/HHS: glucose >600 mg/dL, osmolality >320, ketosis present
- Concurrent sepsis: fever, leukocytosis, hemodynamic instability
- Ketotic States: Alcoholic ketoacidosis, starvation ketosis, medication-induced
Laboratory patterns provide systematic discrimination. DKA shows glucose >250 mg/dL, ketones >3 mmol/L, pH <7.30. Alcoholic ketoacidosis presents normal glucose, elevated ketones, recent alcohol cessation. Lactic acidosis demonstrates lactate >4 mmol/L with tissue hypoperfusion markers.
📌 Remember: MUDPILES for anion gap acidosis - Methanol, Uremia, DKA, Propylene glycol, Isoniazid, Lactic acidosis, Ethylene glycol, Salicylates
| Condition | Glucose | Ketones | Lactate | Osmolality | Key Discriminator |
|---|---|---|---|---|---|
| DKA | >250 | >3.0 | <2.0 | 300-330 | Hyperglycemia + ketosis |
| Alcoholic Ketoacidosis | 50-150 | >3.0 | <2.0 | Normal | Normal glucose + alcohol |
| Lactic Acidosis | Variable | <1.0 | >4.0 | Normal | Elevated lactate |
| HHS | >600 | <1.0 | <2.0 | >320 | Severe hyperglycemia |
| Mixed DKA/HHS | >600 | >3.0 | <2.0 | >320 | Both hyperglycemia + ketosis |
| Starvation Ketosis | <100 | 1-3 | <2.0 | Normal | Mild ketosis only |
The clinical context provides crucial diagnostic clues. Type 1 diabetes history strongly suggests DKA, while Type 2 diabetes with obesity favors HHS. Recent alcohol use points toward alcoholic ketoacidosis. Medication history reveals SGLT2 inhibitor-induced ketosis.
💡 Master This: Serum osmolality calculation distinguishes DKA from HHS: 2(Na+) + glucose/18 + BUN/2.8. Values >320 mOsm/kg suggest HHS component requiring modified fluid management.
Time-sensitive differentiation prevents treatment delays. Point-of-care testing enables rapid glucose and ketone assessment within 5 minutes. Arterial blood gas provides immediate pH and bicarbonate levels. Comprehensive metabolic panel reveals anion gap and additional electrolyte abnormalities.
Systematic differential analysis transforms confusing presentations into clear diagnostic pathways, ensuring appropriate treatment selection while avoiding dangerous therapeutic errors.
⚖️ The Differential Maze: Distinguishing DKA from Metabolic Mimics
🚨 The Treatment Algorithm: Systematic Metabolic Rescue
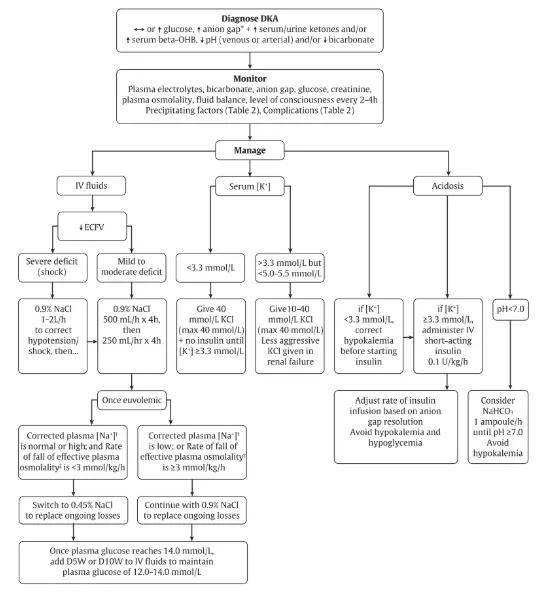
Fluid resuscitation takes priority in hemodynamically unstable patients. Normal saline 1-2 L over first 1-2 hours restores intravascular volume. Subsequent fluid choice depends on serum sodium: 0.45% saline if sodium >150 mEq/L, 0.9% saline if sodium 135-150 mEq/L.
-
Insulin Protocol Implementation:
- Loading dose: 0.1 units/kg IV bolus (optional in mild DKA)
- Continuous infusion: 0.1 units/kg/hour initially
- Target glucose decline: 50-75 mg/dL/hour
- Avoid faster decline to prevent cerebral edema
- Glucose management: Add D5W when glucose <250 mg/dL
- Continue insulin until anion gap closes
- Maintain glucose 150-200 mg/dL during treatment
- Transition criteria: Anion gap <12, bicarbonate >15, pH >7.30
-
Electrolyte Replacement Priorities:
- Potassium management: Most critical electrolyte
- K+ >5.2 mEq/L: Hold replacement, monitor closely
- K+ 3.3-5.2 mEq/L: Add 20-30 mEq/L to fluids
- K+ <3.3 mEq/L: Hold insulin, aggressive K+ replacement
- Phosphate monitoring: Replace if <1.0 mg/dL
- Magnesium assessment: Correct deficiency to enable K+ replacement
- Potassium management: Most critical electrolyte
| Treatment Phase | Timeframe | Fluid Rate | Insulin Rate | Monitoring Frequency | Key Targets |
|---|---|---|---|---|---|
| Initial (0-2h) | First 2 hours | 1-2 L/hour | 0.1 units/kg/h | Every hour | Volume restoration |
| Stabilization (2-6h) | Hours 2-6 | 250-500 mL/h | 0.05-0.1 units/kg/h | Every 2 hours | Glucose 50-75 mg/dL/h decline |
| Resolution (6-12h) | Hours 6-12 | 150-250 mL/h | 0.02-0.05 units/kg/h | Every 4 hours | Anion gap closure |
| Transition (12-24h) | Hours 12-24 | Maintenance | SubQ insulin | Every 6 hours | Stable glucose |
| Recovery (24-48h) | Days 1-2 | PO intake | Home regimen | Daily | Discharge planning |
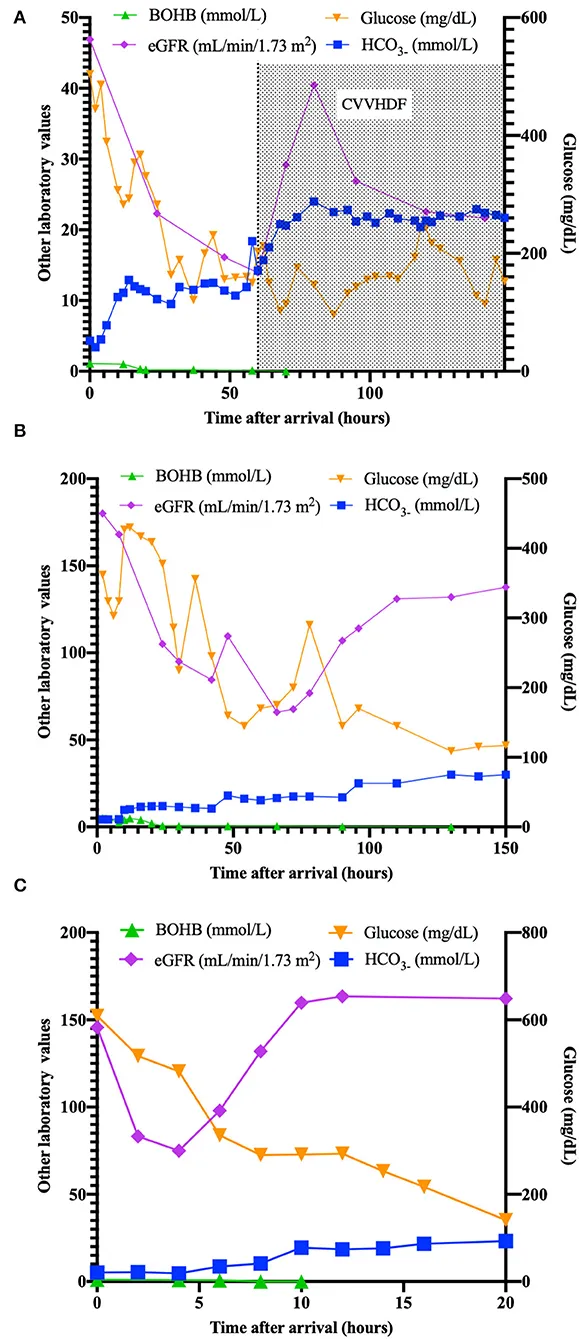
Monitoring protocols prevent treatment complications. Hourly glucose and electrolytes during initial 6 hours, then every 2-4 hours as patient stabilizes. Arterial blood gases every 2-4 hours until pH >7.30 and anion gap normalizes.
💡 Master This: Anion gap closure lags behind glucose normalization by 6-12 hours. Continue insulin until anion gap <12 mEq/L and bicarbonate >15 mEq/L, regardless of glucose levels.
Treatment success requires simultaneous correction of all metabolic abnormalities while vigilantly monitoring for complications like cerebral edema, hypokalemia, and hypoglycemia.
🚨 The Treatment Algorithm: Systematic Metabolic Rescue
🧠 The Integration Matrix: Multi-System DKA Mastery
- Cardiovascular Integration Patterns:
- Volume depletion: Total body water deficit 10-15% in severe DKA
- Cardiac output decreases 20-30% from preload reduction
- Compensatory tachycardia maintains perfusion pressure
- Orthostatic hypotension in >80% of moderate-severe cases
- Electrolyte cardiotoxicity: Potassium shifts create arrhythmia risk
- Hypokalemia: T-wave flattening, U-waves, prolonged QT
- Hyperkalemia: peaked T-waves, widened QRS, heart block
- Acid-base cardiac effects: pH <7.20 depresses myocardial contractility
- Reduced response to catecholamines and inotropes
- Increased risk of ventricular arrhythmias
- Volume depletion: Total body water deficit 10-15% in severe DKA
Neurological complications represent the most feared DKA sequelae. Cerebral edema occurs in 0.5-1% of adult cases but carries 20-90% mortality. Osmotic demyelination from rapid correction threatens permanent neurological damage.
📌 Remember: CEREBRAL edema warning signs - Confusion worsening, Eye movement abnormal, Reflexes abnormal, Extensor posturing, Bradycardia, Respiratory irregularity, Altered pupils, Loss of consciousness
- Renal System Integration:
- Acute kidney injury: Develops in 25-30% of severe DKA cases
- Pre-renal azotemia from volume depletion most common
- Contrast-induced nephropathy risk increased
- Recovery typically complete with adequate hydration
- Electrolyte handling: Impaired renal conservation mechanisms
- Potassium losses: 3-5 mEq/kg total body deficit
- Phosphate depletion: 1-1.5 mmol/kg deficit
- Magnesium losses: Often overlooked but critical for K+ replacement
- Acute kidney injury: Develops in 25-30% of severe DKA cases
| System | Primary Effects | Monitoring Parameters | Critical Thresholds | Intervention Triggers |
|---|---|---|---|---|
| Cardiovascular | Volume depletion, arrhythmias | HR, BP, ECG, CVP | MAP <65, HR >120 | Fluid bolus, pressors |
| Neurological | Cerebral edema, osmotic shifts | GCS, pupils, reflexes | GCS decline >2 | Mannitol, hyperventilation |
| Renal | AKI, electrolyte losses | Creatinine, UOP, lytes | Cr >2x baseline | Nephrology consult |
| Respiratory | Kussmaul, fatigue | RR, ABG, O2 sat | RR >30, pH <7.0 | Ventilatory support |
| Hematologic | Thrombosis, DIC | CBC, PT/PTT, D-dimer | Plt <50K, INR >2 | Anticoagulation |
Advanced monitoring strategies integrate multiple organ systems. Central venous pressure monitoring in severe cases guides fluid management. Arterial lines enable frequent blood gas sampling. Foley catheters track urine output and fluid balance.
💡 Master This: Effective osmolality calculation predicts cerebral edema risk: 2(Na+) + glucose/18. Rapid decline >3 mOsm/kg/hour increases edema risk, requiring slower correction protocols.
The integration matrix reveals how DKA treatment affects multiple organ systems simultaneously, requiring coordinated interventions that optimize metabolic correction while minimizing iatrogenic complications.
🧠 The Integration Matrix: Multi-System DKA Mastery
🎯 The Clinical Arsenal: Rapid DKA Mastery Tools
Essential DKA Arsenal - Critical numbers and thresholds for immediate clinical application:
📌 Remember: DKA 3-6-12 Rule - 3 hours to stabilize, 6 hours to improve, 12 hours to resolve anion gap
- Rapid Assessment Toolkit:
- Severity Stratification: pH <7.00 = severe, 7.00-7.24 = moderate, >7.25 = mild
- Fluid Deficit Calculation: 100 mL/kg for mild, 150 mL/kg moderate, 200 mL/kg severe
- Insulin Dosing: 0.1 units/kg/hour initial rate, adjust by 0.02-0.05 units/kg/hour
- Target glucose decline: 50-75 mg/dL/hour (never >100 mg/dL/hour)
- Add D5W when glucose <250 mg/dL, continue insulin until gap closes
- Potassium Protocol: Hold insulin if K+ <3.3, replace aggressively
- 20-40 mEq/hour if K+ <3.0 mEq/L with cardiac monitoring
- 10-20 mEq/hour if K+ 3.0-4.0 mEq/L in maintenance fluids
| Clinical Scenario | Immediate Action | Target Parameter | Time Frame | Red Flag Threshold |
|---|---|---|---|---|
| Severe DKA (pH <7.0) | 2L NS + insulin 0.1 u/kg/h | MAP >65, glucose ↓50-75/h | First 2 hours | No improvement in 4h |
| Moderate DKA | 1L NS + insulin 0.1 u/kg/h | pH >7.2, gap closure | 6-8 hours | Worsening acidosis |
| Euglycemic DKA | D10W + insulin 0.05 u/kg/h | Ketone clearance | 8-12 hours | Persistent ketosis >24h |
| Pediatric DKA | Careful fluid 10-20 mL/kg | Neuro checks q1h | 24-48 hours | GCS decline |
| Pregnancy DKA | Early insulin, fetal monitoring | Maternal pH >7.25 | 4-6 hours | Fetal distress |
Pattern Recognition Drills - Master these clinical correlations:
- Glucose >800 mg/dL: Think mixed DKA/HHS, modify fluid strategy
- Normal glucose + ketosis: SGLT2 inhibitor or starvation ketosis
- Persistent vomiting: Consider gastroparesis, may need antiemetics
- Abdominal pain: Usually resolves with ketosis correction
- Altered mental status: Correlates with effective osmolality, not glucose
💡 Master This: Transition to subcutaneous insulin requires 2-hour overlap with IV insulin to prevent rebound ketosis. Give first subcutaneous dose 2 hours before stopping IV infusion.
Emergency Protocols for life-threatening complications:
-
Cerebral Edema Management:
- Mannitol 1-2 g/kg IV over 15 minutes
- Hypertonic saline 3% 5-10 mL/kg over 30 minutes
- Hyperventilation to PCO2 25-30 mmHg temporarily
- Neurosurgery consultation for ICP monitoring consideration
-
Severe Hypokalemia Protocol:
- Cardiac monitoring mandatory
- 40 mEq/hour maximum replacement rate
- Central line preferred for concentrated solutions
- Magnesium replacement essential for effective K+ correction
This clinical arsenal transforms DKA management from reactive crisis response into proactive, systematic care that consistently achieves optimal outcomes while preventing complications.
🎯 The Clinical Arsenal: Rapid DKA Mastery Tools
Practice Questions: DKA
Test your understanding with these related questions
A 27-year-old man with a past medical history of type I diabetes mellitus presents to the emergency department with altered mental status. The patient was noted as becoming more lethargic and confused over the past day, prompting his roommates to bring him in. His temperature is 99.0°F (37.2°C), blood pressure is 107/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Laboratory values are ordered as seen below. Serum: Na+: 144 mEq/L Cl-: 100 mEq/L K+: 6.3 mEq/L HCO3-: 16 mEq/L BUN: 20 mg/dL Glucose: 599 mg/dL Creatinine: 1.4 mg/dL Ca2+: 10.2 mg/dL Which of the following is the appropriate endpoint of treatment for this patient?











