Arrhythmias

On this page
⚡ The Cardiac Electrical Storm: Mastering Arrhythmia Fundamentals
Arrhythmias transform the heart's elegant electrical symphony into chaos, threatening hemodynamic collapse within seconds or silently increasing stroke risk over years. You'll master the mechanisms that generate abnormal rhythms, develop systematic pattern recognition to distinguish benign from life-threatening dysrhythmias, and command evidence-based treatment algorithms that save lives in critical moments. This lesson integrates electrophysiology, ECG interpretation, clinical decision-making, and therapeutic intervention into a unified framework that turns rhythm disturbances from diagnostic mysteries into manageable clinical challenges.
The Electrical Foundation: Cardiac Conduction Architecture
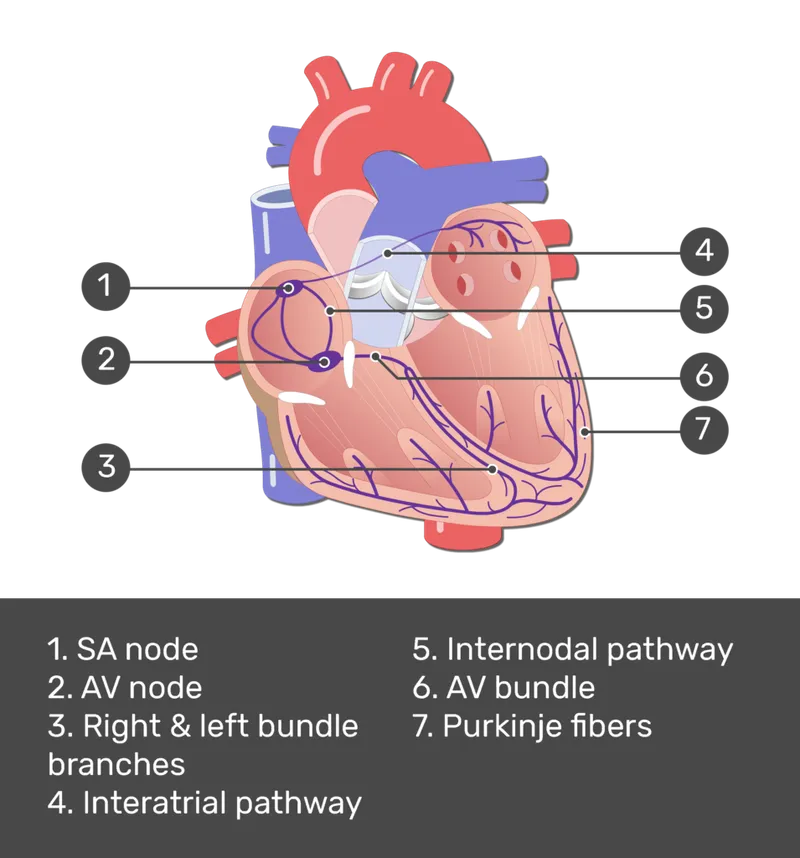
The heart's electrical system operates as a sophisticated biological pacemaker network, generating 60-100 beats per minute with remarkable consistency. The sinoatrial (SA) node fires at 0.5-2.0 Hz, creating the primary rhythm that coordinates 4-6 liters of blood flow per minute.
-
SA Node Dominance
- Intrinsic rate: 60-100 bpm (sinus rhythm)
- Automaticity threshold: -40 to -50 mV
- Recovery time: 1200-1500 ms (normal SNRT)
- Abnormal if >1800 ms (sinus node dysfunction)
- Corrected SNRT >550 ms indicates pathology
-
AV Node Conduction
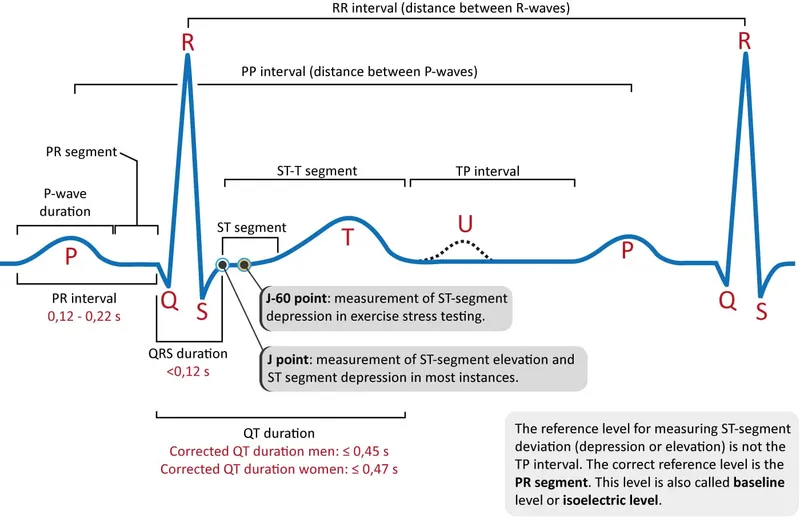
- Normal PR interval: 120-200 ms
- AV node delay: 100-120 ms (allows ventricular filling)
- Refractory period: 400-500 ms
- Protects ventricles from atrial rates >300 bpm
- Decremental conduction slows with faster rates
📌 Remember: PQRST - Pacemaker (SA), QRS (ventricular), Recovery (T wave), Systole (QRS-T), Timing (intervals)
Arrhythmia Classification Matrix
| Origin | Rate Range | QRS Width | Regularity | Clinical Significance | Mortality Risk |
|---|---|---|---|---|---|
| Sinus | 60-100 bpm | <120 ms | Regular | Physiologic | Minimal |
| Atrial | 150-250 bpm | <120 ms | Variable | Stroke risk | Low-Moderate |
| Junctional | 40-60 bpm | <120 ms | Regular | Backup rhythm | Low |
| Ventricular | >150 bpm | >120 ms | Variable | Hemodynamic collapse | High |
| Heart Block | <60 bpm | Variable | Variable | Syncope/death | Moderate-High |
The electrical conduction system's precision enables the heart to maintain cardiac output across varying physiologic demands. Connect this electrical foundation through arrhythmia mechanisms to understand how disruptions create clinical emergencies.
⚡ The Cardiac Electrical Storm: Mastering Arrhythmia Fundamentals
🌪️ The Rhythm Disruption Engine: Arrhythmogenesis Mechanisms
Fundamental Arrhythmia Mechanisms
-
Enhanced Automaticity
- Increased slope of phase 4 depolarization
- Threshold potential: -40 mV (normal) vs -50 mV (enhanced)
- Common triggers: catecholamines, hypoxia, electrolyte imbalance
- Digitalis toxicity increases automaticity at >2.0 ng/mL
- Hypokalemia <3.5 mEq/L enhances ectopic foci
-
Triggered Activity Mechanisms
- Early afterdepolarizations (EADs): occur during phases 2-3
- Delayed afterdepolarizations (DADs): occur after phase 4
- Critical coupling interval: 300-600 ms for torsades initiation
- QT prolongation >500 ms increases EAD risk 5-fold
- Calcium overload triggers DADs at >200% normal
📌 Remember: RATE - Reentry (most common), Automaticity (enhanced), Triggered activity (afterdepolarizations), Escape rhythms
Reentry Circuit Dynamics
Reentry accounts for >80% of clinically significant tachyarrhythmias, requiring three essential components for sustained circus movement:
-
Anatomical Requirements
- Unidirectional block in one pathway
- Slow conduction in alternate route
- Recovery of blocked pathway before circuit completion
- Critical path length: >22 cm for atrial flutter
- Conduction velocity: <0.3 m/s sustains reentry
-
Functional Reentry Patterns
- Leading circle diameter: 2-4 cm (minimum sustainable)
- Wavelength = refractory period × conduction velocity
- Spiral wave dynamics in atrial fibrillation
- Multiple wavelets: 4-6 simultaneous in persistent AF
- Dominant frequency: 6-8 Hz in left atrium
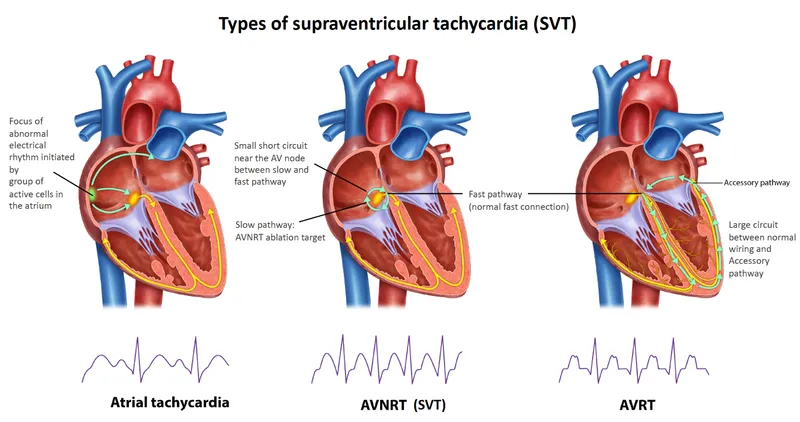
| Reentry Type | Cycle Length | Pathway | Termination | Recurrence Rate |
|---|---|---|---|---|
| AVNRT | 300-400 ms | AV node dual | Adenosine 95% | 30% annually |
| AVRT | 250-350 ms | Accessory | Adenosine 90% | 50% annually |
| Atrial Flutter | 200-250 ms | Tricuspid isthmus | Cardioversion 98% | 80% at 1 year |
| VT (scar) | 400-600 ms | Myocardial scar | Antiarrhythmics 60% | 90% without ICD |
💡 Master This: Reentry requires the wavelength (refractory period × conduction velocity) to be shorter than the circuit path length - this principle explains why class I antiarrhythmics can both terminate and prevent reentrant arrhythmias
Understanding these mechanisms enables prediction of which arrhythmias will respond to specific interventions. Connect reentry dynamics through pattern recognition frameworks to master rapid arrhythmia identification.
🌪️ The Rhythm Disruption Engine: Arrhythmogenesis Mechanisms
🎯 The Rhythm Recognition Arsenal: Clinical Pattern Mastery
The "See This, Think That" Framework
-
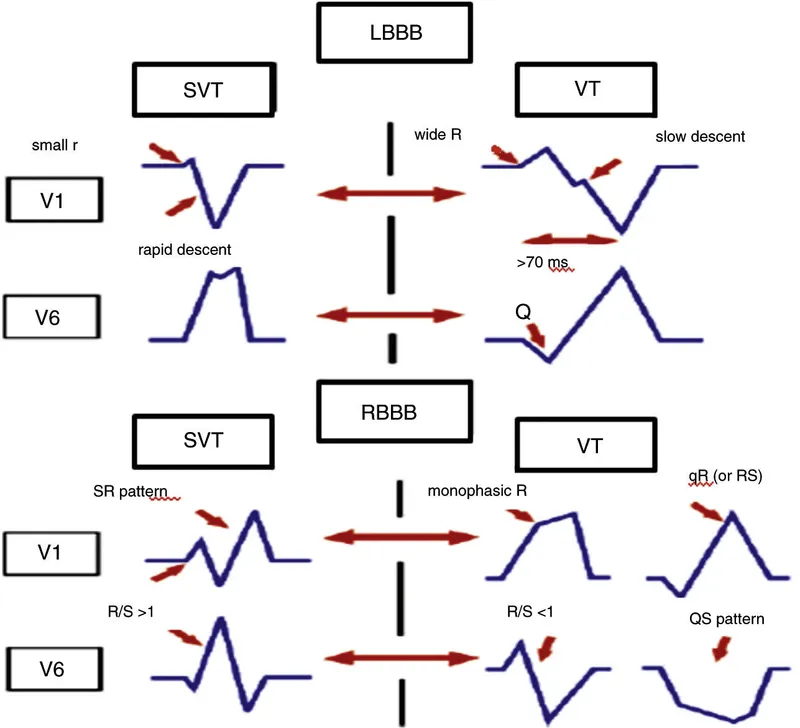
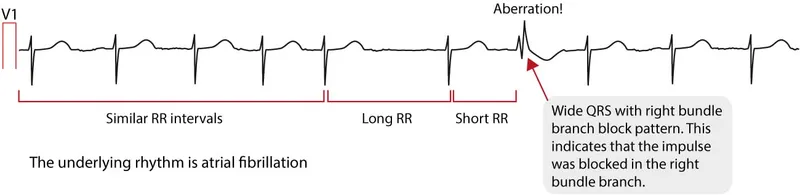
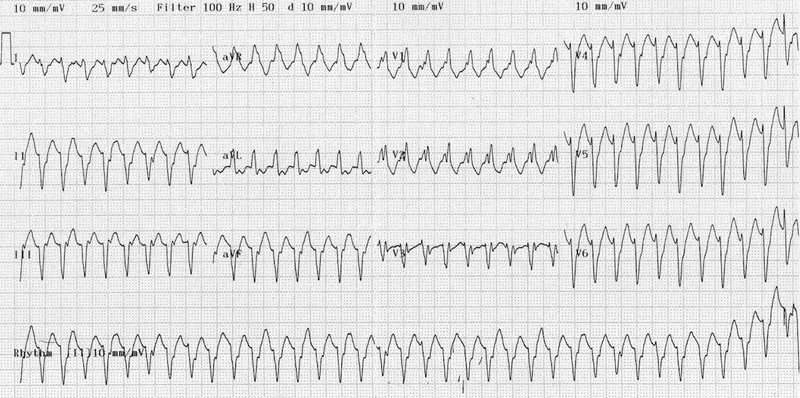
Wide Complex Tachycardia (QRS >120 ms)
- VT probability: 85% if age >35 years
- SVT with aberrancy: 15% overall incidence
- Hemodynamic stability: unreliable for differentiation
- 40% of VT patients remain stable initially
- Blood pressure >90 mmHg in 60% of VT cases
-
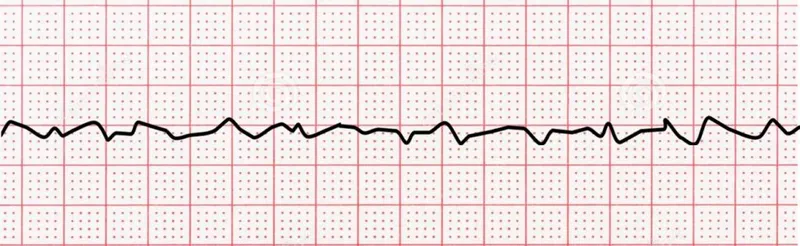
Narrow Complex Tachycardia (QRS <120 ms)
- Regular rhythm: AVNRT (60%), AVRT (30%), atrial flutter (10%)
- Irregular rhythm: Atrial fibrillation (95% probability)
- Rate >220 bpm: suggests accessory pathway conduction
- Maximum AV node conduction: 180-200 bpm in adults
- Rates >250 bpm: pre-excited AF (medical emergency)
📌 Remember: WIDE - Wide = VT until proven otherwise, Irregular narrow = AF, Delta waves = WPW, Extremely fast = accessory pathway
Morphology-Based Discrimination
-
VT Morphology Criteria (Brugada Algorithm)
- Step 1: AV dissociation present = VT (100% specific)
- Step 2: Concordance V1-V6 = VT (96% specific)
- Step 3: Morphology analysis in V1/V6
- RBBB pattern: R >30 ms in V1 = VT
- LBBB pattern: R >60 ms in V1 = VT
-
Accessory Pathway Recognition
- Delta wave: slurred QRS upstroke <120 ms
- Short PR interval: <120 ms (bypass AV node delay)
- Pre-excited AF: irregular wide complex >250 bpm
- Shortest RR interval <250 ms = high-risk pathway
- Risk of VF: 0.15% annually in asymptomatic WPW
| Arrhythmia | Rate (bpm) | Regularity | QRS Width | Key Feature | Emergency Priority |
|---|---|---|---|---|---|
| Sinus Tach | 100-150 | Regular | <120 ms | Gradual onset | Low |
| AVNRT | 150-220 | Regular | <120 ms | Abrupt onset/offset | Moderate |
| Atrial Flutter | 150 (2:1 block) | Regular | <120 ms | Sawtooth waves | Moderate |
| Pre-excited AF | >250 | Irregular | >120 ms | Variable QRS | CRITICAL |
| VT | 150-250 | Regular | >120 ms | AV dissociation | CRITICAL |
| VF | >300 | Chaotic | Variable | No organized QRS | CRITICAL |
💡 Master This: The "3 R's" of emergency arrhythmia assessment - Rate (>150 = urgent), Regularity (irregular wide = dangerous), Recognition (VT vs SVT determines treatment)
Pattern recognition mastery enables split-second therapeutic decisions. Connect these recognition frameworks through systematic discrimination tools to build comprehensive diagnostic expertise.
🎯 The Rhythm Recognition Arsenal: Clinical Pattern Mastery
⚖️ The Diagnostic Discrimination Matrix: Systematic Analysis Tools
The Comprehensive Discrimination Framework
-
Hemodynamic Assessment Limitations
- Myth: VT always causes instability
- Reality: 60% of VT patients maintain adequate blood pressure
- Hemodynamic tolerance depends on:
- LV function: EF <35% increases instability risk 3-fold
- Rate: >200 bpm reduces tolerance regardless of rhythm
- Duration: >30 minutes increases decompensation risk
-
Age-Based Probability Matrix
- Age <35 years: SVT probability 70%, VT 30%
- Age 35-50 years: SVT probability 40%, VT 60%
- Age >50 years: SVT probability 15%, VT 85%
- Prior MI history: VT probability increases to >95%
- Structural heart disease: VT likelihood >90%
📌 Remember: AVOID - Age >50 = VT likely, VT if wide + irregular, Old MI = VT, Instability unreliable, Drugs can cause both
Advanced Morphology Analysis
| ECG Feature | VT Probability | SVT Probability | Sensitivity | Specificity | Clinical Action |
|---|---|---|---|---|---|
| AV Dissociation | 98% | 2% | 25% | 98% | Treat as VT |
| Capture Beats | 100% | 0% | 8% | 100% | Diagnostic of VT |
| Fusion Beats | 100% | 0% | 5% | 100% | Diagnostic of VT |
| Concordance V1-V6 | 96% | 4% | 20% | 96% | Highly suggestive VT |
| Axis Deviation | 85% | 15% | 60% | 85% | Supportive of VT |
-
RBBB Pattern in V1:
- Monophasic R: VT (95% specific)
- Triphasic rSR': SVT (90% specific)
- R wave >30 ms: VT (85% sensitive)
-
LBBB Pattern in V1:
- R wave >60 ms: VT (95% specific)
- Notched downstroke: VT (85% specific)
- QS or rS <70 ms: SVT (90% specific)
Response to Therapeutic Interventions
-
Adenosine Response Patterns
- SVT termination: 95% of AVNRT/AVRT cases
- No response: 98% probability of VT
- Transient AV block: reveals underlying atrial arrhythmia
- Atrial flutter: sawtooth waves become visible
- Atrial tachycardia: discrete P waves at 150-250 bpm
-
Verapamil Response (AVOID in wide complex)
- SVT: terminates 80% of cases
- VT: can cause hemodynamic collapse in 40%
- Pre-excited AF: may precipitate ventricular fibrillation
⭐ Clinical Pearl: Capture beats (narrow QRS during wide complex tachycardia) are 100% diagnostic of VT but occur in only 8% of cases - when present, they're pathognomonic
💡 Master This: The "Rule of 4's" for wide complex tachycardia - if 4+ VT criteria are present (age >50, prior MI, AV dissociation, concordance), treat as VT with >95% confidence
Systematic discrimination prevents therapeutic disasters and guides evidence-based management. Connect these analytical frameworks through treatment algorithms to master therapeutic decision-making.
⚖️ The Diagnostic Discrimination Matrix: Systematic Analysis Tools
🚀 The Therapeutic Command Center: Evidence-Based Treatment Algorithms
Acute Arrhythmia Management Protocols
-
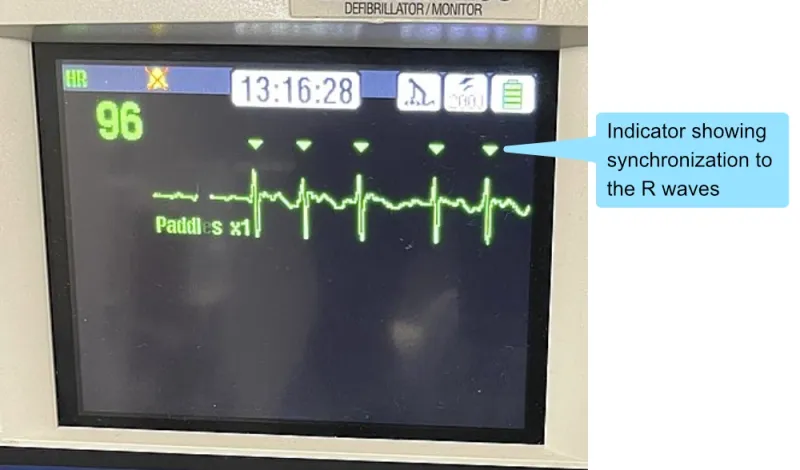
Immediate Cardioversion Indications
- Hemodynamic instability: SBP <90 mmHg
- Acute heart failure: pulmonary edema, cardiogenic shock
- Chest pain: ongoing ischemia with arrhythmia
- Altered mental status: cerebral hypoperfusion
- Success rate: >95% for organized rhythms
- Energy requirements: 100-200J for SVT, 200J for VT
-
Pharmacological Intervention Hierarchy
-
First-line narrow complex: Adenosine 6mg IV push
- Success rate: 85% first dose, 95% with second 12mg dose
- Half-life: <10 seconds (must give rapidly through large IV)
- Contraindications: asthma, 2nd/3rd degree AV block
-
First-line wide complex: Amiodarone 150mg IV over 10 minutes
- VT termination: 60-70% within 24 hours
- Maintenance: 1mg/min × 6 hours, then 0.5mg/min
- Alternative: Procainamide 20-50mg/min (avoid if CHF)
-
Rate Control vs Rhythm Control Strategies
| Arrhythmia | Rate Control | Rhythm Control | Success Rate | Recurrence | Long-term Strategy |
|---|---|---|---|---|---|
| Atrial Fibrillation | Metoprolol 25-100mg BID | Amiodarone 400mg daily | 80% vs 60% | 50% vs 70% | Rate preferred >65 years |
| Atrial Flutter | Diltiazem 120-240mg daily | Cardioversion | 70% vs 95% | 80% vs 60% | Rhythm preferred |
| AVNRT | Verapamil 240mg daily | Ablation | 85% vs 98% | 30% vs 5% | Ablation preferred |
| VT (stable) | Not applicable | Amiodarone/Ablation | N/A vs 80% | N/A vs 20% | ICD + ablation |
- Atrial fibrillation: resting HR <110 bpm (lenient control)
- Strict control: <80 bpm rest, <110 bpm exercise
- Heart failure patients: target 60-100 bpm
- Beta-blockers: mortality benefit in AF with HFrEF
- Digoxin: neutral mortality, avoid in women
- Anticoagulation Decision Framework
- CHA₂DS₂-VASc Score: guides anticoagulation in AF
- Score ≥2: anticoagulation recommended (Class I)
- Score 1: consider anticoagulation (Class IIa)
- Score 0: no anticoagulation needed
- Bleeding risk: HAS-BLED score ≥3 = high risk
- 3.7% annual major bleeding with warfarin
- 2.1% annual major bleeding with DOACs
- CHA₂DS₂-VASc Score: guides anticoagulation in AF
Advanced Therapeutic Interventions
-
Catheter Ablation Success Rates
- AVNRT: 98% success, <1% recurrence
- AVRT: 95% success, 5% recurrence
- Atrial flutter: 95% success, 10% recurrence
- VT (ischemic): 70% success, 30% recurrence
- Complications: 2-5% major, <0.5% mortality
- Procedure time: 2-6 hours depending on complexity
-
Device Therapy Indications
- ICD primary prevention: EF ≤35% on optimal medical therapy
- ICD secondary prevention: survived VT/VF arrest
- CRT-D: EF ≤35%, QRS ≥150ms, LBBB morphology
- 30% mortality reduction with appropriate ICD therapy
- 25% reduction in heart failure hospitalizations with CRT
⭐ Clinical Pearl: Synchronized cardioversion uses 50-75% less energy than unsynchronized shocks and reduces risk of inducing ventricular fibrillation from 15% to <1%
💡 Master This: The "ABCD" of arrhythmia management - Assess stability, Broad vs narrow complex, Cardioversion if unstable, Drugs if stable - this sequence prevents therapeutic errors in >95% of cases
Evidence-based algorithms ensure optimal outcomes across diverse clinical scenarios. Connect these treatment frameworks through multi-system integration to understand complex arrhythmia interactions.
🚀 The Therapeutic Command Center: Evidence-Based Treatment Algorithms
🔗 The Arrhythmia Ecosystem: Multi-System Integration Mastery
Cardiovascular-Neurohormonal Integration
-
Autonomic Nervous System Modulation
- Sympathetic stimulation: increases automaticity, shortens refractory periods
- Parasympathetic activation: prolongs AV conduction, increases refractoriness
- Circadian patterns: 6 AM-12 PM peak for sudden cardiac death
- 40% of VT/VF episodes occur during morning hours
- Cortisol surge increases catecholamine sensitivity by 300%
-
Heart Failure-Arrhythmia Interactions
- Structural remodeling: creates slow conduction zones for reentry
- Electrical remodeling: alters ion channel expression
- AF in heart failure: increases mortality by 15-20%
- Tachycardia-induced cardiomyopathy: EF improves >15% with rate control
- CRT response: reduced by 50% in persistent AF
📌 Remember: HEART - Hormones affect rhythm, Electrolytes alter conduction, Autonomics modulate rate, Remodeling creates substrate, Timing determines outcomes
Electrolyte-Arrhythmia Relationships
| Electrolyte | Normal Range | Arrhythmia Risk | ECG Changes | Treatment Target | Monitoring Frequency |
|---|---|---|---|---|---|
| Potassium | 3.5-5.0 mEq/L | <3.0 or >6.0 | U waves, peaked T | 4.0-4.5 mEq/L | q6h if abnormal |
| Magnesium | 1.7-2.2 mg/dL | <1.5 mg/dL | Prolongs QT | >2.0 mg/dL | Daily |
| Calcium | 8.5-10.5 mg/dL | <7.0 or >12.0 | QT changes | 8.5-10.0 mg/dL | Daily |
| Phosphorus | 2.5-4.5 mg/dL | <2.0 mg/dL | Indirect effects | >2.5 mg/dL | Daily |
- Mechanism: enhanced phase 4 depolarization, prolonged repolarization
- Risk threshold: <3.0 mEq/L increases VT risk 5-fold
- Digitalis interaction: hypokalemia increases digitalis toxicity by 10-fold
- Target K⁺ 4.0-4.5 mEq/L in digitalis patients
- Replacement rate: 10-20 mEq/hour maximum IV
- Magnesium Deficiency Syndromes
- Torsades de pointes: Mg²⁺ <1.5 mg/dL in >80% of cases
- Treatment: 2-4 grams IV magnesium sulfate over 15 minutes
- Refractory hypokalemia: often requires magnesium repletion first
- 60% of hypokalemic patients have concurrent hypomagnesemia
- Magnesium normalizes Na⁺-K⁺-ATPase pump function
Drug-Arrhythmia Interactions
-
QT-Prolonging Medications
- High risk: haloperidol, droperidol, sotalol, dofetilide
- Moderate risk: amiodarone, quinidine, procainamide
- Monitoring: baseline QTc, then q24h during initiation
- QTc >500 ms: discontinue offending agent
- ΔQTc >60 ms: significant prolongation requiring action
-
Proarrhythmic Effects
- Class IC agents: 2.5-fold increase in mortality post-MI (CAST trial)
- Antiarrhythmic paradox: 5-10% incidence of new arrhythmias
- Digitalis toxicity: bidirectional VT, accelerated junctional rhythm
- Therapeutic range: 0.8-2.0 ng/mL
- Toxicity risk: >2.5 ng/mL in >90% of cases
⭐ Clinical Pearl: Magnesium sulfate terminates torsades de pointes in >90% of cases, even when serum magnesium levels are normal - it's the first-line therapy regardless of measured levels
💡 Master This: The "4 M's" of arrhythmia complexity - Metabolism (electrolytes), Medications (drug interactions), Mechanics (heart failure), Modulation (autonomics) - addressing all four domains optimizes treatment success
Multi-system integration reveals the complexity underlying arrhythmia management. Connect these interaction patterns through rapid mastery frameworks to build comprehensive clinical expertise.
🔗 The Arrhythmia Ecosystem: Multi-System Integration Mastery
🎯 The Arrhythmia Mastery Toolkit: Rapid Clinical Reference
The Essential Numbers Arsenal
📌 Remember: CRITICAL 6 - 6mg adenosine, 6 seconds for VF, 60 bpm bradycardia threshold, 600 ms QT danger, 6 hours amiodarone loading, 6 months anticoagulation minimum
-
Emergency Thresholds
- Heart rate: <60 bpm (bradycardia), >100 bpm (tachycardia)
- Blood pressure: <90 mmHg systolic = unstable
- QTc intervals: >500 ms = high torsades risk
- Energy levels: 200J synchronized cardioversion, 360J defibrillation
- Biphasic: 120-200J equivalent efficacy to 360J monophasic
- Pediatric: 2 J/kg initial, 4 J/kg subsequent
-
Drug Dosing Quick Reference
- Adenosine: 6mg → 12mg → 18mg IV push
- Amiodarone: 150mg IV over 10 min, then 1mg/min × 6h
- Metoprolol: 25-50mg BID, titrate to 200mg BID maximum
- Diltiazem: 0.25 mg/kg IV, then 5-15 mg/hour infusion
Rapid Pattern Recognition Drills
| ECG Pattern | Rate | Regularity | QRS | Immediate Action | Success Rate |
|---|---|---|---|---|---|
| Narrow regular >150 | 150-220 | Regular | <120ms | Adenosine 6mg | 95% |
| Wide regular >150 | 150-250 | Regular | >120ms | Assume VT, cardiovert | 98% |
| Irregular narrow | Variable | Irregular | <120ms | Rate control AF | 85% |
| Irregular wide >250 | >250 | Irregular | >120ms | EMERGENCY cardiovert | 100% |
| No organized rhythm | >300 | Chaotic | None | Defibrillate immediately | 90% |
The Clinical Decision Matrix
-
The "STABLE" Assessment
- Systolic BP >90 mmHg
- Tolerating rhythm without distress
- Alert and oriented mental status
- Breathing without pulmonary edema
- Lack of chest pain/ischemia
- Effective cardiac output maintained
-
Post-Cardioversion Priorities
- Anticoagulation: if AF >48 hours or unknown duration
- Electrolyte optimization: K⁺ 4.0-4.5, Mg²⁺ >2.0
- Rate control: prevent rapid recurrence
- Rhythm monitoring: 24-48 hours minimum observation
💡 Master This: The "Rule of 200's" - QRS >120ms + rate >200 bpm + age >50 = treat as VT with >95% accuracy, avoiding the fatal error of giving AV nodal blockers to ventricular tachycardia
Long-Term Management Frameworks
-
Ablation Referral Criteria
- Symptomatic SVT: after 2+ episodes despite medication
- Atrial flutter: first-line therapy (>95% success rate)
- AF with heart failure: if rate control inadequate
- VT with ICD: >3 appropriate shocks in 24 hours
-
Anticoagulation Duration Guidelines
- Cardioversion: 3 weeks before + 4 weeks after minimum
- Persistent AF: lifelong if CHA₂DS₂-VASc ≥2
- Post-ablation: 3 months minimum, then reassess stroke risk
- Bleeding vs thrombosis: 2-3:1 ratio favors anticoagulation in most patients
The arrhythmia mastery toolkit transforms complex rhythm disturbances into systematic, evidence-based management approaches, ensuring optimal patient outcomes through rapid recognition and appropriate intervention strategies.
🎯 The Arrhythmia Mastery Toolkit: Rapid Clinical Reference
Practice Questions: Arrhythmias
Test your understanding with these related questions
A 44-year-old man comes to the emergency department because of persistent palpitations for the past 2 hours. The day before, he was at a wedding, where he drank several glasses of wine and 9–10 vodka cocktails. He has never had similar symptoms before. He is a manager at a software company and has recently had a lot of work-related stress. He is otherwise healthy and takes no medications. His temperature is 36.5°C (97.7°F), pulse is 90/min and irregularly irregular, respirations are 13/min, and his blood pressure is 128/60 mm Hg. Physical examination shows no other abnormalities. An ECG is performed; no P-waves can be identified. Echocardiography shows no valvular abnormalities and normal ventricular function. One hour later, a repeat ECG shows normal P waves followed by narrow QRS complexes. He is still experiencing occasional palpitations. Which of the following is the most appropriate next step in management?













