ACS

On this page
🎯 ACS Mastery: The Cardiac Emergency Command Center
Acute coronary syndrome transforms stable coronary disease into a life-threatening emergency within minutes, demanding rapid recognition and decisive action. You'll master ECG interpretation to distinguish STEMI from NSTEMI, harness troponin kinetics to confirm myocardial injury, stratify risk to guide intensity of care, and deploy time-sensitive therapies from antiplatelet agents to reperfusion strategies. Beyond the acute phase, you'll learn to anticipate mechanical and electrical complications, then build a secondary prevention framework that transforms survival into long-term cardiovascular health.

ACS represents the clinical manifestation of acute myocardial ischemia, encompassing a spectrum from unstable angina to massive STEMI. Understanding ACS transforms emergency medicine from reactive care to predictive intervention, where pattern recognition saves lives and systematic approaches prevent catastrophic outcomes.
📌 Remember: ACS-STEMI - Acute Coronary Syndrome includes STEMI (complete occlusion, >20 minutes), Troponin-positive NSTEMI (partial occlusion, <20 minutes), Elevated biomarkers, Myocardial necrosis, Ischemic symptoms
The pathophysiological foundation centers on atherosclerotic plaque rupture triggering thrombotic occlusion of coronary arteries. Type 1 MI accounts for 85% of ACS presentations, while Type 2 MI (supply-demand mismatch) represents 10-15% of cases. Troponin elevation occurs within 3-6 hours, peaks at 12-24 hours, and remains elevated for 7-14 days.
-
STEMI Classification
- Complete coronary occlusion with >1mm ST-elevation in ≥2 contiguous leads
- Door-to-balloon time target: <90 minutes for primary PCI
- Door-to-needle time target: <30 minutes for fibrinolysis
- Anterior STEMI: LAD occlusion affecting 40-50% of left ventricle
- Inferior STEMI: RCA occlusion with 20-30% mortality if complicated
- Posterior STEMI: LCX occlusion requiring V7-V9 leads for detection
-
NSTEMI/Unstable Angina Classification
- Partial coronary occlusion with preserved antegrade flow
- TIMI Risk Score >3 indicates high-risk requiring invasive strategy <24 hours
- GRACE Score >140 predicts >3% in-hospital mortality
- Troponin-positive NSTEMI: myocardial necrosis with biomarker elevation
- Troponin-negative unstable angina: ischemia without cellular death
| ACS Type | Troponin | ECG Changes | Mortality | Reperfusion Target |
|---|---|---|---|---|
| STEMI | Elevated | ST-elevation ≥1mm | 6-14% | <90 min PCI |
| NSTEMI | Elevated | ST-depression/T-wave | 3-8% | <24 hr invasive |
| Unstable Angina | Normal | Dynamic changes | 1-3% | Medical therapy |
| Posterior MI | Elevated | R-waves V1-V3 | 8-12% | <90 min PCI |
| RV Infarct | Elevated | ST-elevation V4R | 15-25% | Volume + PCI |
💡 Master This: Time-dependent myocardial salvage follows the "golden hour" principle - myocardial viability decreases 1% per minute during complete occlusion. Collateral circulation can extend this window to 6-12 hours in 20-30% of patients.
The clinical presentation varies dramatically based on patient demographics, comorbidities, and infarct location. Classic chest pain occurs in only 60-70% of ACS patients, while atypical presentations dominate in women >65 years, diabetics, and elderly patients >75 years.
Connect this foundational understanding through systematic ECG interpretation to master the electrical signatures that guide immediate therapeutic decisions.
🎯 ACS Mastery: The Cardiac Emergency Command Center
⚡ The Electrical Battlefield: ECG Mastery in ACS
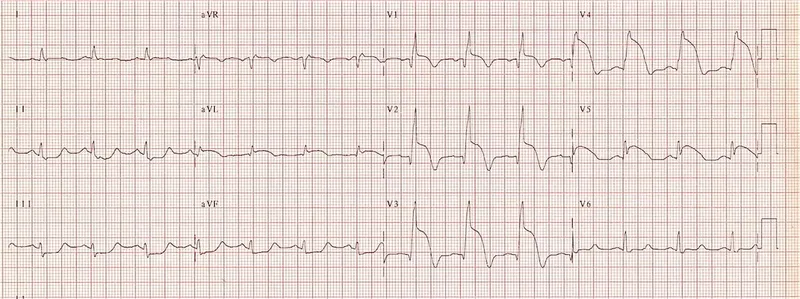
The ECG serves as the primary triage tool separating STEMI (immediate reperfusion) from NSTEMI/unstable angina (risk stratification pathway). Serial ECGs obtained every 15-30 minutes during active symptoms capture dynamic changes indicating evolving occlusion or successful reperfusion.
📌 Remember: STEMI-LEADS - ST-elevation Two Electrical Millimeters In Leads Examine Adjacent Distribution Segments (≥1mm in limb leads, ≥2mm in precordial leads, in ≥2 contiguous leads)
STEMI Criteria requires ≥1mm ST-elevation in ≥2 contiguous limb leads OR ≥2mm ST-elevation in ≥2 contiguous precordial leads. New LBBB or LBBB of unknown duration constitutes STEMI-equivalent requiring immediate reperfusion. Posterior STEMI presents as ≥2mm ST-depression in V1-V3 with tall R-waves and upright T-waves.
-
Anatomical Localization Patterns
- Anterior STEMI: V1-V6 indicating LAD occlusion affecting 40-50% LV mass
- Inferior STEMI: II, III, aVF indicating RCA occlusion in 85% of cases
- Lateral STEMI: I, aVL, V5-V6 indicating LCX occlusion with 15-20% LV mass
- Reciprocal changes: ST-depression in opposite leads confirms transmural ischemia
- RV involvement: ST-elevation V4R >1mm in 30-50% of inferior STEMIs
- Posterior extension: R/S ratio >1 in V1-V2 with ST-depression
-
STEMI-Equivalent Patterns
- New LBBB: QRS >120ms with appropriate discordance indicating proximal LAD occlusion
- Wellens Pattern: Biphasic T-waves V2-V3 indicating critical LAD stenosis >90%
- De Winter Pattern: Upsloping ST-depression with tall T-waves indicating LAD occlusion
- Sgarbossa Criteria: Concordant ST-elevation ≥1mm OR concordant ST-depression ≥1mm V1-V3
- Modified Sgarbossa: ST/S ratio ≥-0.25 in leads with QS or rS
| ECG Pattern | Location | Artery | LV Involvement | Mortality Risk |
|---|---|---|---|---|
| V1-V6 elevation | Anterior | LAD | 40-50% | 8-12% |
| II,III,aVF elevation | Inferior | RCA (85%) | 20-30% | 6-10% |
| I,aVL,V5-V6 elevation | Lateral | LCX | 15-20% | 4-8% |
| V7-V9 elevation | Posterior | LCX/RCA | 15-25% | 8-15% |
| New LBBB | Anterior | Proximal LAD | 45-55% | 12-18% |
💡 Master This: Dynamic ECG changes during active symptoms indicate unstable plaque with high thrombotic burden. Transient ST-elevation resolving with symptom relief suggests vasospasm or intermittent occlusion requiring urgent invasive evaluation.
NSTEMI/Unstable Angina ECG patterns include ST-depression ≥0.5mm, T-wave inversions ≥1mm, or transient ST-elevation <20 minutes. Horizontal or downsloping ST-depression carries higher risk than upsloping depression. Deep T-wave inversions >5mm in anterior leads suggest critical LAD disease.
Connect these electrical patterns through biomarker interpretation to understand the molecular signatures that confirm myocardial necrosis and guide therapeutic intensity.
⚡ The Electrical Battlefield: ECG Mastery in ACS
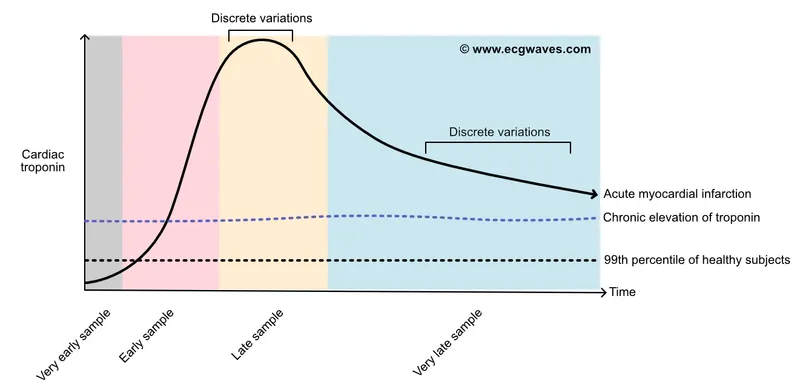
🧬 Molecular Messengers: The Troponin Revolution
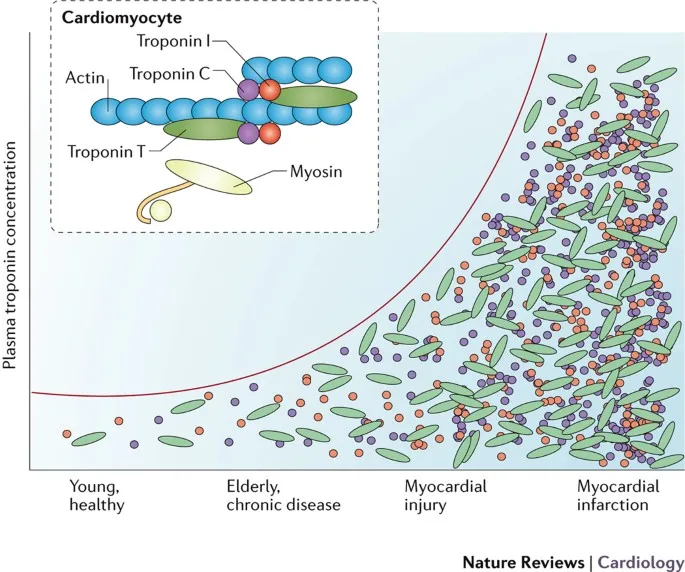
High-sensitivity troponin (hs-cTn) revolutionized ACS diagnosis by detecting myocardial injury at 10-fold lower concentrations than conventional assays. The 99th percentile upper reference limit serves as the diagnostic threshold, while delta changes ≥20% between serial measurements indicate acute injury versus chronic elevation.
📌 Remember: TROPONIN-RISE - Time-dependent Release Occurs Post-Occlusion Necrosis In Nanogram Ranges Identifying Small Elevations (rises 3-6 hours, peaks 12-24 hours, elevated 7-14 days)
Troponin kinetics follow predictable patterns enabling diagnostic timing optimization. Initial elevation occurs 3-6 hours post-symptom onset, peaks at 12-24 hours, and remains elevated for 7-14 days. High-sensitivity assays detect elevation within 1-3 hours, enabling accelerated diagnostic protocols.
-
Troponin Diagnostic Thresholds
- hs-cTnI: 99th percentile typically 15-40 ng/L (assay-dependent)
- hs-cTnT: 99th percentile typically 14-19 ng/L (Roche assay)
- Delta criteria: ≥20% change between serial measurements 3-6 hours apart
- Rule-out threshold: <5 ng/L at presentation with <2-hour symptoms
- Rule-in threshold: >5x 99th percentile indicates large MI
- Intermediate zone: 1-5x 99th percentile requires serial testing
-
Accelerated Diagnostic Protocols
- 0/1-hour algorithm: Baseline and 1-hour troponin for rapid rule-out/rule-in
- 0/3-hour algorithm: Traditional approach with 3-hour repeat if initial negative
- Single measurement: hs-cTn <5 ng/L at >6 hours post-symptom onset
- Rule-out criteria: hs-cTnT <12 ng/L AND hs-cTnI <6 ng/L at presentation
- Rule-in criteria: hs-cTnT >52 ng/L OR hs-cTnI >120 ng/L at presentation
| Biomarker | Rise Time | Peak Time | Duration | Sensitivity | Specificity |
|---|---|---|---|---|---|
| hs-cTnI | 1-3 hours | 12-24 hours | 7-14 days | 95-99% | 95-99% |
| hs-cTnT | 1-3 hours | 12-24 hours | 7-14 days | 95-99% | 95-99% |
| CK-MB | 3-6 hours | 12-18 hours | 2-3 days | 85-95% | 85-95% |
| Myoglobin | 1-2 hours | 6-8 hours | 24 hours | 95-99% | 70-80% |
| CK-Total | 4-8 hours | 18-24 hours | 3-4 days | 80-90% | 75-85% |
Non-ACS troponin elevation occurs in pulmonary embolism (15-50% of cases), sepsis (40-85% of ICU patients), renal failure (chronic elevation in >90% with GFR <30), and heart failure exacerbation (50-70% of acute episodes). Clinical context and troponin kinetics differentiate acute coronary occlusion from alternative etiologies.
💡 Master This: High-sensitivity troponin enables rule-out of MI in >50% of chest pain patients within 1 hour using validated algorithms. Negative predictive value >99.5% when hs-cTn <5 ng/L at presentation with >3-hour symptom duration.
Copeptin and heart-type fatty acid binding protein (H-FABP) serve as early markers complementing troponin for accelerated diagnosis. Copeptin rises immediately with stress response, while H-FABP appears within 1-3 hours of myocardial injury.
Connect these molecular insights through risk stratification frameworks to transform biomarker data into actionable clinical decisions that guide therapeutic intensity.
🧬 Molecular Messengers: The Troponin Revolution
⚖️ Risk Stratification: The Clinical Crystal Ball
Risk stratification separates high-risk patients requiring urgent invasive management from low-risk patients suitable for conservative approaches. TIMI Risk Score provides simple bedside calculation, while GRACE Score offers sophisticated mortality prediction incorporating physiological variables.
📌 Remember: TIMI-SCORE - Three Ischemic Markers Identify Severe Coronary Occlusion Requiring Emergent (Age ≥65, ≥3 CAD risk factors, Known CAD >50%, ASA use 7 days, Severe angina <24hr, ST-deviation ≥0.5mm, Elevated troponin)
TIMI Risk Score for UA/NSTEMI incorporates seven variables each worth 1 point: age ≥65 years, ≥3 CAD risk factors, known CAD stenosis ≥50%, ASA use within 7 days, severe angina <24 hours, ST-deviation ≥0.5mm, and elevated cardiac biomarkers. Scores 0-2 indicate low risk (4.7% events), scores 3-4 indicate intermediate risk (19.9% events), and scores 5-7 indicate high risk (40.9% events).
-
TIMI Risk Score Stratification
- Low Risk (0-2 points): 4.7% composite endpoint at 14 days
- Intermediate Risk (3-4 points): 19.9% composite endpoint at 14 days
- High Risk (5-7 points): 40.9% composite endpoint at 14 days
- Score ≥3: Consider invasive strategy within 24 hours
- Score ≥5: Urgent invasive strategy within 12 hours
- Score 6-7: Immediate invasive strategy with high-intensity antithrombotic therapy
-
GRACE Risk Score Variables
- Age: Strongest predictor (up to 58 points for age >90)
- Heart rate: 2 points per 10 bpm above 50 bpm
- Systolic BP: Inverse relationship with higher scores for hypotension
- Creatinine: 4 points per mg/dL above normal
- Killip class: 0 points (Class I) to 59 points (Class IV)
- Cardiac arrest: 39 points if present at admission
| Risk Score | Low Risk | Intermediate Risk | High Risk | Invasive Timing |
|---|---|---|---|---|
| TIMI (0-7) | 0-2 (4.7%) | 3-4 (19.9%) | 5-7 (40.9%) | Score ≥3: <24hr |
| GRACE (0-372) | <109 (1%) | 109-140 (3%) | >140 (8%) | Score >140: Urgent |
| CRUSADE (0-100) | <31 (3.1%) | 31-50 (5.5%) | >50 (11.9%) | Bleeding risk |
| PURSUIT (0-18) | 0-8 (4.9%) | 9-11 (8.8%) | 12-18 (19.9%) | 30-day mortality |
| HEART (0-10) | 0-3 (0.9%) | 4-6 (12%) | 7-10 (65%) | 6-week MACE |
High-risk features mandating urgent invasive strategy include recurrent ischemia, hemodynamic instability, sustained VT/VF, mechanical complications, and heart failure. Very high-risk patients require invasive strategy within 2 hours including refractory angina, dynamic ECG changes, and cardiogenic shock.
💡 Master This: Risk score integration guides evidence-based decision making - TIMI ≥3 OR GRACE >140 indicates invasive strategy benefit with NNT 48 for preventing death/MI. Low-risk patients (both scores low) have <2% event rates suitable for early discharge.
Bleeding risk assessment using CRUSADE or HAS-BLED scores balances ischemic benefit against hemorrhagic risk. Elderly patients >75 years, renal dysfunction, prior bleeding, and anemia increase bleeding risk requiring dose adjustments and access site optimization.
Connect these risk stratification insights through therapeutic decision algorithms to master the treatment pathways that transform risk predictions into optimal patient outcomes.
⚖️ Risk Stratification: The Clinical Crystal Ball
🎯 Therapeutic Command Center: ACS Treatment Algorithms
Reperfusion strategy represents the cornerstone of STEMI management, with primary PCI preferred when available within 90 minutes of first medical contact. Fibrinolytic therapy serves as alternative reperfusion when PCI unavailable or delays >90 minutes anticipated, provided no contraindications exist.
📌 Remember: REPERFUSION-TIME - Rapid Evaluation Primary Emergent Revascularization Fibrinolysis Urgent Salvage Intervention Optimal Needs Timing Immediate Management Execution (Door-to-balloon <90 min, Door-to-needle <30 min)
Primary PCI achieves superior outcomes compared to fibrinolysis with 2-3% absolute mortality reduction, 50% reduction in reinfarction, and 60% reduction in intracranial hemorrhage. Mechanical reperfusion restores TIMI 3 flow in >90% of cases versus 50-60% with fibrinolytic therapy.
-
Primary PCI Advantages
- TIMI 3 flow achievement: >90% versus 50-60% with fibrinolysis
- 30-day mortality: 7% versus 9% with fibrinolytic therapy
- Reinfarction rate: 3% versus 7% with fibrinolytic therapy
- Intracranial hemorrhage: <0.5% versus 0.5-1% with fibrinolysis
- Major bleeding: 4-6% versus 5-10% with fibrinolytic therapy
- Stroke prevention: 1% versus 2% with fibrinolytic therapy
-
Fibrinolytic Therapy Indications
- STEMI presentation with symptom onset <12 hours
- PCI unavailable or anticipated delay >90 minutes
- No absolute contraindications to thrombolytic therapy
- Tenecteplase (TNK): Single bolus dosing 0.5 mg/kg (maximum 50 mg)
- Alteplase (tPA): 15 mg bolus + 0.75 mg/kg over 30 minutes + 0.5 mg/kg over 60 minutes
- Reteplase (rPA): Two 10-unit boluses separated by 30 minutes
| Reperfusion Strategy | TIMI 3 Flow | 30-Day Mortality | Reinfarction | ICH Risk | Time Window |
|---|---|---|---|---|---|
| Primary PCI | >90% | 7% | 3% | <0.5% | <12 hours |
| Fibrinolysis | 50-60% | 9% | 7% | 0.5-1% | <12 hours |
| Rescue PCI | 85-90% | 8% | 4% | <0.5% | After failed lysis |
| Facilitated PCI | 80-85% | 10% | 5% | 1-2% | Not recommended |
| No reperfusion | 15-20% | 15-20% | 12% | <0.1% | >12 hours |
NSTEMI/Unstable Angina management follows risk-stratified approach with invasive timing determined by clinical presentation and risk scores. Very high-risk patients require immediate invasive strategy, high-risk patients need early invasive approach <24 hours, and low-risk patients may receive conservative management.
💡 Master This: Optimal medical therapy includes dual antiplatelet therapy, anticoagulation, beta-blockers, ACE inhibitors, and high-intensity statins. Guideline-directed medical therapy reduces cardiovascular mortality by 25-30% independent of reperfusion strategy.
Antiplatelet therapy combines aspirin 325 mg loading with P2Y12 inhibitor for dual antiplatelet therapy (DAPT). Clopidogrel 600 mg, prasugrel 60 mg, or ticagrelor 180 mg provide loading doses followed by maintenance therapy for 12 months minimum.
Connect these therapeutic algorithms through complication recognition frameworks to master the management of mechanical, electrical, and hemodynamic complications that threaten post-ACS recovery.
🎯 Therapeutic Command Center: ACS Treatment Algorithms
⚠️ Complication Surveillance: The Post-ACS Minefield
MI complications follow predictable timelines enabling anticipatory monitoring and early intervention. Electrical complications dominate first 24 hours, mechanical complications peak 3-7 days post-MI, and remodeling complications develop over weeks to months.
📌 Remember: COMPLICATIONS-TIME - Cardiogenic shock Occurs Mechanical Problems Late Ischemic Changes Arrhythmias Thromboembolism Infarct Occur Now Sudden Timing Important Monitoring Essential (Hours: arrhythmias, Days: mechanical, Weeks: remodeling)
Cardiogenic shock complicates 5-10% of STEMIs with 40-50% mortality despite optimal therapy. Mechanical complications including papillary muscle rupture, ventricular septal defect, and free wall rupture occur in <5% of modern MIs but carry >50% mortality without emergency surgery.
-
Electrical Complications (0-24 hours)
- Ventricular fibrillation: 4-18% of STEMIs, highest risk first 4 hours
- Complete heart block: 15-20% of inferior STEMIs, 5% of anterior STEMIs
- Atrial fibrillation: 10-15% of all MIs, associated with larger infarcts
- Accelerated idioventricular rhythm: Benign reperfusion arrhythmia in 20-40%
- Sustained VT: 3-5% of STEMIs, requires immediate cardioversion
- Bradyarrhythmias: Sinus bradycardia in 30-40% of inferior MIs
-
Mechanical Complications (3-7 days)
- Papillary muscle rupture: 1-3% incidence, >50% mortality without surgery
- Ventricular septal defect: 1-2% incidence, 87% mortality without repair
- Free wall rupture: <1% incidence, >90% mortality, surgical emergency
- Acute mitral regurgitation: Papillary muscle dysfunction in 10-15%
- Pseudoaneurysm formation: Contained rupture requiring surgical repair
- Pericarditis: 10-15% of transmural MIs, usually benign
| Complication | Incidence | Timeline | Mortality | Treatment |
|---|---|---|---|---|
| Cardiogenic Shock | 5-10% | 0-48 hours | 40-50% | IABP + Revascularization |
| VF/VT | 4-18% | 0-24 hours | 15-30% | Defibrillation + Antiarrhythmics |
| Complete AV Block | 5-20% | 0-72 hours | 10-20% | Temporary Pacing |
| Papillary Rupture | 1-3% | 3-7 days | >50% | Emergency Surgery |
| VSD | 1-2% | 3-7 days | 87% | Emergency Repair |
| Free Wall Rupture | <1% | 3-7 days | >90% | Emergency Surgery |
Cardiogenic shock management requires immediate revascularization combined with mechanical circulatory support. Intra-aortic balloon pump (IABP) provides modest hemodynamic support, while Impella or ECMO offer more robust assistance for severe shock. Vasopressor support with norepinephrine or dopamine maintains perfusion pressure.
💡 Master This: Right heart catheterization differentiates mechanical complications - VSD shows oxygen step-up >7% from RA to RV, while acute MR demonstrates prominent V-waves in pulmonary capillary wedge pressure. Thermodilution cardiac output quantifies hemodynamic severity.
Late complications include ventricular aneurysm formation (10-15% of anterior STEMIs), mural thrombus (5-15% of large anterior MIs), and post-infarction pericarditis (Dressler syndrome in <5%). LV remodeling with progressive dilatation leads to heart failure in 20-30% of large MIs.
Connect this complication awareness through secondary prevention strategies to master the long-term management approaches that prevent recurrent events and optimize cardiovascular outcomes.
⚠️ Complication Surveillance: The Post-ACS Minefield
🛡️ Secondary Prevention Arsenal: The Long-Term Victory Strategy
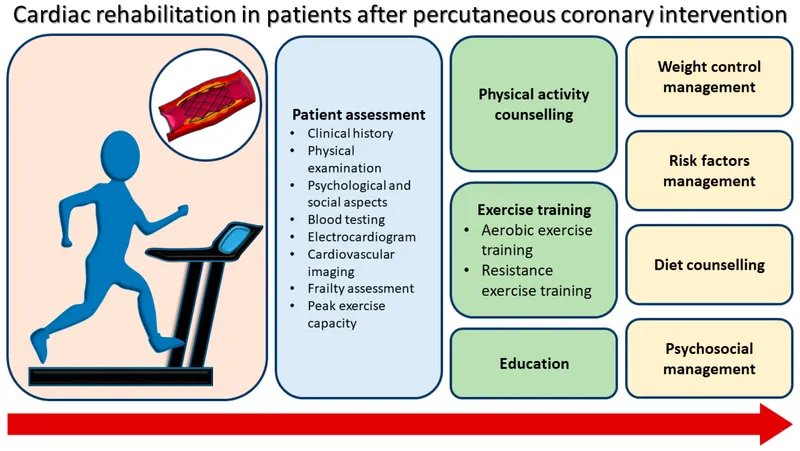
Guideline-directed medical therapy (GDMT) forms the foundation of secondary prevention, with evidence-based medications providing additive cardiovascular protection. Dual antiplatelet therapy, high-intensity statins, ACE inhibitors, and beta-blockers constitute the core regimen with proven mortality benefit.
📌 Remember: SECONDARY-MEDS - Statins Essential Clopidogrel One-year Needed Dual Antiplatelet Required Yearly Monitoring Enalapril Daily Sustained (Aspirin + P2Y12 inhibitor + Statin + ACE inhibitor + Beta-blocker)
Antiplatelet therapy continues aspirin 75-100 mg daily indefinitely plus P2Y12 inhibitor for minimum 12 months. Clopidogrel 75 mg, prasugrel 10 mg, or ticagrelor 90 mg twice daily provide P2Y12 inhibition with different bleeding profiles and efficacy rates. Extended DAPT beyond 12 months reduces ischemic events but increases bleeding risk.
-
Statin Therapy Optimization
- High-intensity statins: Atorvastatin 40-80 mg or rosuvastatin 20-40 mg
- LDL target: <70 mg/dL for secondary prevention, <55 mg/dL for very high risk
- Non-statin therapy: Ezetimibe 10 mg if LDL >70 mg/dL on maximum statin
- PCSK9 inhibitors: Evolocumab or alirocumab if LDL >70 mg/dL despite statin + ezetimibe
- Monitoring: Lipid panel at 4-6 weeks and every 3 months until target achieved
- Muscle symptoms: Check CK and consider statin rechallenge or alternative therapy
-
ACE Inhibitor/ARB Therapy
- Lisinopril 5-40 mg daily or metoprolol 25-200 mg twice daily
- Target dose: Maximum tolerated dose based on BP and renal function
- Monitoring: Creatinine and potassium at 1-2 weeks after initiation/dose changes
- ARB alternative: Losartan 25-100 mg daily if ACE inhibitor intolerant
- Contraindications: Bilateral renal artery stenosis, hyperkalemia >5.5 mEq/L
- Benefits: 15-20% mortality reduction in post-MI patients with LV dysfunction
| Medication Class | Drug Examples | Target Dose | Mortality Benefit | Monitoring |
|---|---|---|---|---|
| Antiplatelet | ASA + Clopidogrel | 81mg + 75mg | 20-25% reduction | Bleeding signs |
| Statin | Atorvastatin | 40-80mg daily | 15-30% reduction | LDL, CK, LFTs |
| ACE Inhibitor | Lisinopril | 5-40mg daily | 15-20% reduction | Cr, K+, BP |
| Beta-Blocker | Metoprolol | 25-200mg BID | 10-15% reduction | HR, BP, HF signs |
| Ezetimibe | Ezetimibe | 10mg daily | 6% additional | LDL levels |
Lifestyle modifications provide substantial cardiovascular protection equivalent to pharmacological interventions. Smoking cessation reduces cardiovascular risk by 36% within 2 years, while Mediterranean diet decreases MACE by 30% in secondary prevention trials.
💡 Master This: Polypill strategy combining aspirin, statin, and ACE inhibitor in single formulation improves medication adherence by 33% and reduces cardiovascular events by 21%. Medication adherence <80% doubles cardiovascular mortality risk compared to optimal compliance.
Risk factor targets include blood pressure <130/80 mmHg, LDL cholesterol <70 mg/dL, HbA1c <7% in diabetics, and complete smoking cessation. Achieving all targets provides cumulative risk reduction >70% for recurrent cardiovascular events.
This comprehensive secondary prevention approach transforms ACS survivors from high-risk patients into optimally protected individuals with dramatically reduced cardiovascular mortality and improved long-term outcomes.
🛡️ Secondary Prevention Arsenal: The Long-Term Victory Strategy
Practice Questions: ACS
Test your understanding with these related questions
A primary care physician who focuses on treating elderly patients is researching recommendations for secondary prevention. She is particularly interested in recommendations regarding aspirin, as she has several patients who ask her if they should take it. Of the following, which patient should be started on lifelong aspirin as monotherapy for secondary prevention of atherosclerotic cardiovascular disease?













