Screening guidelines

On this page
🎯 Screening Fundamentals: The Medical Detective's Toolkit
Screening guidelines transform uncertainty into action by defining who to test, when to test, and how to interpret results across entire populations. You'll master the frameworks that balance sensitivity against specificity, understand how disease prevalence reshapes predictive values, and learn why age, risk factors, and test characteristics determine which patients benefit most from screening. By exploring the architecture behind major guidelines and the precision of risk-stratified approaches, you'll gain the clinical judgment to deploy screening as both population health strategy and individualized care tool.
The Screening Foundation Matrix
Effective screening programs operate on four interconnected pillars that determine program success and population impact:
-
Disease Characteristics
- High prevalence in target population (>1 per 1,000 screened)
- Significant morbidity/mortality if undetected
- Natural history well understood
- Detectable preclinical phase exists
- Treatment more effective in early stages (>20% mortality reduction)
-
Test Performance Metrics
- Sensitivity ≥80% for target conditions
- Specificity ≥95% to minimize false positives
- Positive predictive value >10% in target population
- Acceptable cost per quality-adjusted life year (<$50,000)
-
Population Factors
- Defined target demographic with clear risk stratification
- Accessible healthcare infrastructure for follow-up
- Cultural acceptance >70% participation rates
- Sustainable funding mechanisms established
📌 Remember: ASSURED criteria for screening tests - Affordable, Sensitive, Specific, User-friendly, Rapid, Equipment-free, Deliverable. Each criterion must score ≥7/10 for program viability.
Wilson-Jungner Criteria: The Gold Standard Framework
| Criterion | Threshold | Clinical Application | Success Rate | Monitoring Parameter |
|---|---|---|---|---|
| Important health problem | >5% population burden | Cancer, CVD, diabetes | 85% program adoption | Disease-specific mortality |
| Natural history understood | >10 years research base | Cervical cancer progression | 90% accuracy | Stage distribution shifts |
| Detectable early stage | 2-5 year window | Breast cancer mammography | 75% early detection | Lead time measurement |
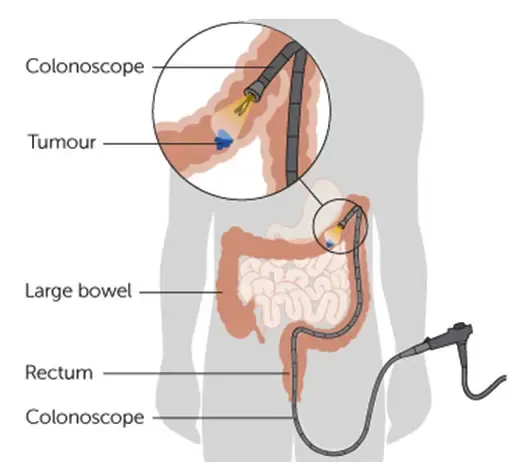
| Suitable test available | >80% sensitivity/specificity | Colonoscopy for CRC | 70% compliance | False positive rates |
| Acceptable to population | >60% participation | Pap smear acceptance | 65% repeat screening | Patient satisfaction scores |
Evidence Hierarchy and Implementation Science
Modern screening programs require Level 1 evidence from randomized controlled trials demonstrating mortality reduction, not just earlier detection. The evidence pyramid prioritizes:
-
Systematic Reviews/Meta-analyses
- ≥3 high-quality RCTs with >10,000 participants
- Mortality reduction ≥15% with p<0.01
- Number needed to screen <1,000 for benefit
- Follow-up duration ≥10 years minimum
-
Individual RCTs
- Population-based recruitment with >80% eligibility
- Intention-to-treat analysis preserving randomization
- Contamination rates <10% between groups
- Loss to follow-up <20% at study completion
💡 Master This: The lead time bias inflates survival statistics by 2-5 years without true mortality benefit. Demand mortality endpoints, not just survival curves, when evaluating screening evidence.

USPSTF Grading System: Clinical Translation Framework
The United States Preventive Services Task Force translates research evidence into clinical recommendations using a structured grading system that guides practice decisions:
-
Grade A Recommendations (High Certainty, Substantial Benefit)
- Mammography ages 50-74 years (mortality reduction 19%)
- Colonoscopy ages 45-75 years (mortality reduction 15%)
- Cervical cancer screening ages 21-65 years
- Blood pressure screening ≥18 years annually
-
Grade B Recommendations (High Certainty, Moderate Benefit)
- Lung cancer screening 55-80 years, 30+ pack-years
- Osteoporosis screening ≥65 years women
- Depression screening with treatment systems
- Hepatitis C screening 1945-1965 birth cohort
⭐ Clinical Pearl: Grade C recommendations require individualized decision-making based on patient values and risk factors. Grade D recommendations show net harm and should be actively discouraged. Grade I statements indicate insufficient evidence for recommendation.
Connect these foundational principles through population-specific applications to understand how screening guidelines adapt across diverse demographic groups and clinical contexts.
🎯 Screening Fundamentals: The Medical Detective's Toolkit
🔬 Population Dynamics: The Screening Equation Mastery
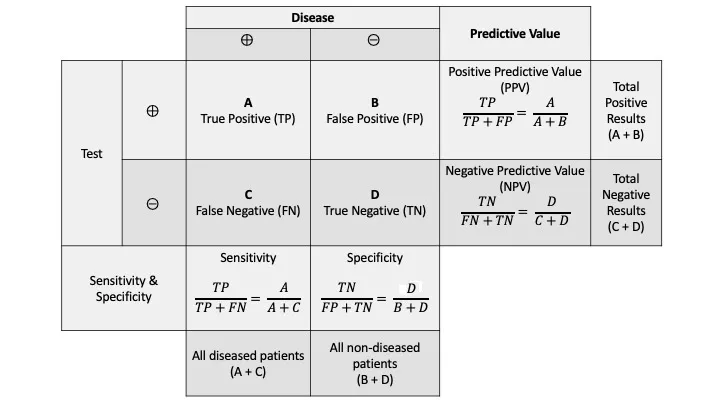
Prevalence-Performance Relationship Matrix
Test performance metrics demonstrate dramatic variation across population prevalence rates, fundamentally altering clinical utility and cost-effectiveness:
-
High-Prevalence Populations (>5% disease prevalence)
- Positive predictive value increases 10-fold compared to general population
- Number needed to screen decreases to <200 for one true positive
- False positive rate impact minimized (<2% absolute increase)
- Cost per quality-adjusted life year <$25,000
-
Moderate-Prevalence Populations (1-5% disease prevalence)
- Balanced risk-benefit ratio with acceptable false positive burden
- Screening intervals can be shortened by 25-50% for optimal detection
- Requires robust follow-up systems for 15-20% positive results
- Cost-effectiveness threshold $25,000-$50,000 per QALY
-
Low-Prevalence Populations (<1% disease prevalence)
- False positives outnumber true positives 10:1 even with 95% specificity
- Extended screening intervals reduce harm without compromising mortality benefit
- Shared decision-making essential for informed participation
- Cost per QALY often exceeds $100,000 threshold
📌 Remember: PPV = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + ((1-Specificity) × (1-Prevalence))] - This equation determines whether your positive result represents true disease or screening harm.
Risk Stratification Architecture
| Risk Category | Prevalence Multiplier | Screening Intensity | Interval Modification | Cost-Effectiveness | Participation Target |
|---|---|---|---|---|---|
| Very High Risk | 5-10x baseline | Enhanced protocols | 50% shorter intervals | <$15,000/QALY | >90% uptake |
| High Risk | 3-5x baseline | Standard plus adjuncts | 25% shorter intervals | $15,000-$30,000/QALY | >80% uptake |
| Average Risk | 1x baseline | Standard guidelines | Guideline intervals | $30,000-$50,000/QALY | >70% uptake |
| Low Risk | 0.3-0.5x baseline | Extended intervals | 50% longer intervals | $50,000-$100,000/QALY | >60% uptake |
| Very Low Risk | <0.3x baseline | Consider discontinuation | No screening | >$100,000/QALY | Individualized |
Demographic Modifiers and Clinical Applications
Age, sex, ethnicity, and socioeconomic factors create 2-10 fold variations in disease prevalence, fundamentally altering screening program design and effectiveness:
-
Age-Related Prevalence Curves
- Cancer incidence increases exponentially after age 50 years
- Cardiovascular disease risk doubles every decade after age 40 years
- Osteoporosis prevalence triples in postmenopausal women
- Cognitive decline screening becomes cost-effective after age 65 years
-
Ethnic and Genetic Variations
- BRCA mutations in Ashkenazi Jewish populations (1 in 40 vs 1 in 400 general)
- Sickle cell disease in African Americans (1 in 365 vs 1 in 16,300 Caucasians)
- Tay-Sachs disease screening in specific populations
- Hepatitis B prevalence 10-15x higher in Asian populations
💡 Master This: Bayes' theorem governs all screening decisions - prior probability (prevalence) determines post-test probability more than test characteristics. A 99% specific test in a 0.1% prevalence population yields only 9% positive predictive value.
Implementation Science and Program Sustainability
Successful screening programs require systems thinking that addresses population reach, clinical infrastructure, and long-term sustainability:
-
Population Reach Optimization
- Reminder systems increase participation by 15-25%
- Community health workers improve uptake in underserved populations by 30-40%
- Mobile screening units reach rural populations with 2-3x baseline participation
- Electronic health record integration automates 85% of screening reminders
-
Quality Assurance Frameworks
- Double reading of screening tests reduces false negative rates by 15%
- Standardized protocols decrease inter-observer variation by 40%
- Continuous medical education maintains >95% accuracy standards
- Performance feedback improves detection rates by 10-20%
⭐ Clinical Pearl: Programs with <60% population participation show minimal mortality benefit regardless of test performance. Equity considerations require targeted outreach to populations with 2-3x higher disease burden but 50% lower screening rates.
Connect population dynamics through evidence-based guideline development to understand how statistical principles translate into clinical recommendations and practice standards.
🔬 Population Dynamics: The Screening Equation Mastery
🎯 Guideline Architecture: The Clinical Decision Framework
USPSTF Recommendation Framework Architecture
The United States Preventive Services Task Force employs a rigorous methodology that transforms research evidence into clinical recommendations through systematic evidence review and benefit-harm analysis:
-
Evidence Review Process
- Systematic literature search covering ≥20 years of publications
- ≥2 independent reviewers assess study quality using standardized criteria
- Meta-analysis when ≥3 comparable studies with >5,000 participants
- Risk of bias assessment eliminates 30-40% of initial studies
-
Benefit-Harm Assessment Matrix
- Mortality reduction weighted as primary outcome (coefficient 1.0)
- Morbidity reduction receives secondary weighting (coefficient 0.6-0.8)
- False positive harms quantified through anxiety scores and unnecessary procedures
- Overdiagnosis rates calculated from screening vs non-screening populations
📌 Remember: GRADE methodology - Grading of Recommendations Assessment, Development and Evaluation. Evidence quality: High (confident), Moderate (likely), Low (uncertain), Very Low (very uncertain). Recommendation strength: Strong (most patients) vs Weak (many patients).
Evidence Quality and Recommendation Strength Matrix
| Evidence Quality | Mortality Benefit | Harm Profile | Recommendation Grade | Clinical Action | Implementation Rate |
|---|---|---|---|---|---|
| High | >15% reduction | Minimal harms | Grade A | Offer/provide service | >85% adoption |
| High | 10-15% reduction | Low harms | Grade B | Offer/provide service | 70-85% adoption |
| Moderate | 5-10% reduction | Moderate harms | Grade C | Individualized decision | 40-60% adoption |
| Low/Moderate | <5% reduction | High harms | Grade D | Discourage service | <20% adoption |
| Insufficient | Unclear benefit | Unknown harms | Grade I | Insufficient evidence | Variable adoption |
Guideline Implementation and Clinical Translation
Evidence-based recommendations require systematic implementation strategies that address clinician behavior, system barriers, and patient engagement:
-
Clinician-Level Interventions
- Electronic health record alerts increase screening rates by 20-35%
- Performance feedback with peer comparison improves compliance by 15-25%
- Clinical decision support tools reduce inappropriate screening by 40%
- Continuing medical education with case-based learning shows sustained behavior change
-
System-Level Implementation
- Standing orders for eligible patients increase screening rates by 30-50%
- Nurse-led protocols achieve equivalent outcomes with 25% lower costs
- Population health registries identify 90% of eligible patients
- Quality improvement collaboratives accelerate adoption by 6-12 months
💡 Master This: The knowledge-to-practice gap averages 17 years for guideline adoption. Implementation science reduces this to 2-5 years through systematic barrier identification and multi-level interventions.
Guideline Conflicts and Resolution Strategies
Multiple professional organizations often generate conflicting recommendations for identical screening scenarios, requiring clinicians to navigate evidence interpretation differences and organizational priorities:
-
Common Conflict Patterns
- Starting age disagreements (typically 5-10 year differences between organizations)
- Screening interval variations (annual vs biennial vs triennial approaches)
- Stopping age controversies (life expectancy >10 years vs chronological age)
- Risk stratification thresholds (2-fold vs 4-fold risk elevation requirements)
-
Resolution Framework Approach
- USPSTF recommendations receive regulatory preference for coverage decisions
- Specialty society guidelines often provide more aggressive screening approaches
- Patient preference integration through shared decision-making protocols
- Local adaptation based on population characteristics and resource availability
⭐ Clinical Pearl: When guidelines conflict, prioritize USPSTF Grade A/B recommendations for population-level decisions and specialty society guidelines for high-risk individuals. Document rationale for deviation from standard guidelines in medical records.
Quality Measurement and Outcome Monitoring
Guideline effectiveness requires continuous monitoring through quality metrics that assess both process measures (screening rates) and outcome measures (mortality reduction):
-
Process Quality Indicators
- Screening participation rates by demographic subgroups
- Time to diagnostic resolution for abnormal results (<30 days target)
- False positive rates and patient anxiety scores
- Provider adherence to age-appropriate screening recommendations
-
Outcome Quality Indicators
- Stage distribution shifts toward earlier disease detection
- Mortality trends in screened vs unscreened populations
- Cost-effectiveness ratios with annual recalculation
- Health equity metrics across racial/ethnic groups
💡 Master This: Donabedian's framework - Structure (resources), Process (activities), Outcomes (results) - guides comprehensive quality assessment. Leading indicators (process) predict lagging indicators (outcomes) by 2-5 years.
Connect guideline architecture through risk-stratified implementation to understand how evidence-based recommendations adapt to individual patient characteristics and clinical contexts.
🎯 Guideline Architecture: The Clinical Decision Framework
⚖️ Risk Stratification Mastery: The Precision Screening Matrix
Genetic Risk Architecture and Clinical Applications
Hereditary cancer syndromes create 5-50 fold increased disease risk, requiring intensive surveillance protocols that begin 10-25 years earlier than population-based recommendations:
-
High-Penetrance Genetic Mutations
- BRCA1/2 mutations: Breast cancer risk 40-87%, ovarian cancer 11-40%
- Lynch syndrome: Colorectal cancer risk 52-82%, endometrial cancer 25-60%
- TP53 mutations (Li-Fraumeni): >90% lifetime cancer risk by age 70
- APC mutations (FAP): 100% colorectal cancer risk without prophylactic surgery
-
Moderate-Penetrance Variants
- CHEK2, ATM, PALB2: 2-4 fold increased breast cancer risk
- Polygenic risk scores: 1.5-3 fold risk modification across multiple variants
- Pharmacogenomic markers: CYP2D6 variants affect tamoxifen efficacy
- Ancestry-specific variants: BRCA founder mutations in Ashkenazi populations
📌 Remember: NCCN genetic testing criteria - National Comprehensive Cancer Network guidelines define ≥10% probability thresholds for genetic counseling referral. Multigene panels detect pathogenic variants in 5-10% of tested individuals.
Family History Risk Quantification Matrix
| Risk Factor | Relative Risk | Absolute Risk Increase | Screening Modification | Evidence Level | Clinical Action |
|---|---|---|---|---|---|
| 1st degree, age <50 | 2.0-4.0x | +10-25% lifetime | Start 10 years earlier | Level A | Enhanced screening |
| 2+ 1st degree relatives | 3.0-6.0x | +15-35% lifetime | Annual vs biennial | Level A | Genetic counseling |
| 1st degree, bilateral | 4.0-8.0x | +20-45% lifetime | Add MRI screening | Level B | High-risk clinic |
| Male breast cancer | 5.0-10.0x | +25-50% lifetime | BRCA testing indicated | Level A | Cascade testing |
| Ovarian cancer history | 10.0-20.0x | +40-70% lifetime | Intensive surveillance | Level A | Prophylactic options |
Environmental and Lifestyle Risk Integration
Environmental exposures and lifestyle factors create modifiable risk profiles that influence screening recommendations and prevention strategies:
-
Occupational and Environmental Exposures
- Asbestos exposure: 5-10 fold increased mesothelioma and lung cancer risk
- Radiation exposure: Linear dose-response for breast cancer risk (>10 Gy cumulative)
- Benzene exposure: 2-5 fold increased leukemia risk in chemical workers
- Radon exposure: Second leading cause of lung cancer (>4 pCi/L action level)
-
Lifestyle Risk Modification Opportunities
- Smoking cessation: 50% lung cancer risk reduction within 10 years
- Alcohol reduction: 7% breast cancer risk reduction per 10g/day decrease
- Weight management: 30% endometrial cancer risk reduction with BMI <25
- Physical activity: 20-25% colorectal cancer risk reduction with ≥150 min/week
💡 Master This: Attributable risk quantifies preventable disease burden - 85% of lung cancers attributable to smoking, 30% of cancers attributable to diet and physical activity. Population attributable fraction guides public health priorities.
Comorbidity-Adjusted Screening Strategies
Medical comorbidities and life expectancy considerations fundamentally alter screening benefit-harm ratios, requiring individualized approaches that balance potential benefits against competing mortality risks:
-
Life Expectancy Integration
- ≥10 years life expectancy required for screening mortality benefit
- Charlson Comorbidity Index predicts 10-year survival with 85% accuracy
- Functional status assessment using activities of daily living scales
- Geriatric assessment incorporating cognitive function and frailty markers
-
Competing Risk Analysis
- Cardiovascular disease mortality >cancer mortality in diabetes patients >75 years
- Chronic kidney disease reduces screening benefit due to limited treatment options
- Severe COPD (FEV1 <50%) contraindicates lung cancer screening
- Dementia eliminates screening benefit due to treatment intolerance
⭐ Clinical Pearl: Shared decision-making becomes mandatory when life expectancy 5-10 years or significant comorbidities present. Decision aids improve patient understanding by 40% and reduce decisional conflict by 25%.
Precision Medicine Integration and Future Directions
Emerging technologies enable molecular risk stratification that promises personalized screening protocols based on individual biological signatures:
-
Circulating Biomarker Panels
- Circulating tumor DNA detection for early cancer screening
- Protein biomarker signatures for organ-specific cancer risk
- MicroRNA profiles predicting cancer development 2-5 years before clinical detection
- Metabolomic signatures identifying high-risk metabolic states
-
Artificial Intelligence Risk Prediction
- Machine learning algorithms integrating >1,000 variables for risk prediction
- Imaging-based AI detecting subtle abnormalities missed by human readers
- Electronic health record mining for automated risk stratification
- Wearable device integration providing continuous risk monitoring
💡 Master This: Precision screening will shift from age-based protocols to risk-based algorithms incorporating genetic, environmental, and molecular factors. Implementation challenges include cost-effectiveness, health equity, and clinical workflow integration.
Connect risk stratification mastery through screening modality selection to understand how individual risk profiles determine optimal test selection and surveillance protocols.
⚖️ Risk Stratification Mastery: The Precision Screening Matrix
🔬 Screening Modality Optimization: The Diagnostic Arsenal
Imaging Modality Performance Matrix
Different screening technologies demonstrate distinct performance profiles that determine optimal applications across risk-stratified populations:
-
Mammography Performance Characteristics
- Sensitivity 85-90% in average-risk women ages 50-74
- Specificity 88-95% with digital breast tomosynthesis improvement
- False positive rate 8-12% requiring additional imaging
- Radiation dose 0.4 mGy per bilateral examination
-
Magnetic Resonance Imaging Applications
- Sensitivity 95-99% in BRCA mutation carriers
- Specificity 70-85% with higher false positive burden
- Contrast enhancement required with gadolinium-based agents
- Cost 8-10x higher than mammography per examination
-
Computed Tomography Screening Protocols
- Low-dose CT for lung cancer screening in high-risk smokers
- Sensitivity 85-95% for ≥6mm nodules with volumetric analysis
- False positive rate 20-25% in baseline screening rounds
- Radiation dose 1.5 mGy per chest examination
📌 Remember: ALARA principle - As Low As Reasonably Achievable radiation exposure. Cumulative radiation from annual CT screening over 20 years may induce 1-2 cancers per 10,000 screened, requiring benefit-harm balance.
Biomarker-Based Screening Technologies
| Screening Test | Sensitivity | Specificity | PPV (High Risk) | PPV (Average Risk) | Clinical Application |
|---|---|---|---|---|---|
| PSA (>4.0 ng/mL) | 85% | 30% | 25-30% | 15-20% | Prostate cancer |
| CA-125 (>35 U/mL) | 80% | 95% | 10-15% | 2-5% | Ovarian cancer |
| CEA (>5.0 ng/mL) | 70% | 90% | 15-20% | 5-8% | Colorectal cancer |
| AFP (>20 ng/mL) | 75% | 85% | 30-40% | 8-12% | Hepatocellular carcinoma |
| Circulating tumor DNA | 90% | 98% | 60-80% | 40-60% | Multi-cancer detection |
Endoscopic and Invasive Screening Procedures
Direct visualization techniques provide gold standard accuracy but require procedural expertise and carry intervention-related risks:
-
Colonoscopy Performance Standards
- Sensitivity >95% for adenomas ≥10mm with high-definition imaging
- Cecal intubation rate >95% with adequate bowel preparation
- Adenoma detection rate >25% in men >50 years, >15% in women >50 years
- Withdrawal time ≥6 minutes correlates with improved detection rates
-
Alternative Colorectal Screening Modalities
- CT colonography sensitivity 85-90% for ≥6mm polyps
- Fecal immunochemical testing detects 75-85% of colorectal cancers
- Stool DNA testing combines FIT with molecular markers
- Capsule endoscopy emerging for average-risk screening
💡 Master This: Procedural complications occur in 0.1-0.3% of screening colonoscopies, including perforation (1 in 1,000) and bleeding (1 in 300). Risk-benefit analysis favors colonoscopy when life expectancy >10 years.
Emerging Technologies and Future Screening Platforms
Next-generation screening technologies promise improved accuracy with reduced patient burden through non-invasive approaches:
-
Liquid Biopsy Applications
- Circulating tumor cells detection in early-stage cancers
- Cell-free DNA methylation patterns for tissue-of-origin identification
- Protein biomarker panels using machine learning algorithms
- Exosome analysis for cancer-specific signatures
-
Artificial Intelligence Integration
- Computer-aided detection improves mammography sensitivity by 5-10%
- Deep learning algorithms for pathology image analysis
- Natural language processing for risk factor extraction from clinical notes
- Predictive modeling using electronic health record data
⭐ Clinical Pearl: Multi-cancer early detection tests using circulating tumor DNA show 50-60% sensitivity for 12+ cancer types with >99% specificity. False positive rates <1% make population screening feasible, but cost-effectiveness remains under evaluation.
Quality Assurance and Performance Monitoring
Screening program effectiveness requires continuous quality monitoring across technical, interpretive, and clinical domains:
-
Technical Quality Standards
- Mammography facilities must meet FDA certification requirements
- CT lung screening requires dose optimization and nodule management protocols
- Laboratory proficiency testing for biomarker assays
- Equipment calibration and maintenance schedules
-
Interpretive Performance Metrics
- Radiologist double-reading reduces false negative rates by 15%
- Audit and feedback systems improve detection rates by 10-20%
- Continuing medical education requirements for screening certification
- Performance benchmarking against national standards
💡 Master This: Screening program success depends on system integration - patient identification, test performance, result communication, abnormal result follow-up, and outcome tracking. Failure at any step compromises program effectiveness.
Connect screening modality optimization through implementation strategies to understand how technological capabilities translate into real-world screening program success and population health impact.
🔬 Screening Modality Optimization: The Diagnostic Arsenal
🎯 Implementation Excellence: The Screening System Architecture
System-Level Implementation Framework
Successful screening programs require multi-level interventions that address organizational, provider, and patient factors simultaneously:
-
Organizational Infrastructure Requirements
- Electronic health record integration with automated eligibility identification
- Population health registries tracking screening due dates and overdue patients
- Quality improvement teams with dedicated screening coordinators
- Performance dashboards providing real-time screening metrics
-
Clinical Workflow Optimization
- Standing orders for age-appropriate screening in eligible patients
- Nurse-led protocols for screening education and appointment scheduling
- Point-of-care reminders integrated into clinical decision support
- Standardized patient education materials in multiple languages
-
Quality Assurance Systems
- Tracking systems ensuring ≥95% of abnormal results receive timely follow-up
- Patient navigation for complex cases requiring multi-specialty coordination
- Outcome monitoring with cancer registry linkage
- Continuous improvement cycles using Plan-Do-Study-Act methodology
📌 Remember: Triple Aim framework - Better health outcomes, improved patient experience, lower per capita costs. Screening programs must demonstrate improvement in all three domains for sustainable implementation.
Patient Engagement and Participation Optimization
| Intervention Strategy | Participation Increase | Cost per Additional Screen | Sustainability | Evidence Level | Implementation Complexity |
|---|---|---|---|---|---|
| Automated reminders | 15-25% | $5-15 | High | Level A | Low |
| Patient navigation | 25-35% | $50-150 | Moderate | Level A | Moderate |
| Community health workers | 30-40% | $75-200 | Moderate | Level B | High |
| Mobile screening units | 40-60% | $200-500 | Low | Level B | High |
| Financial incentives | 20-30% | $25-100 | Low | Level C | Moderate |
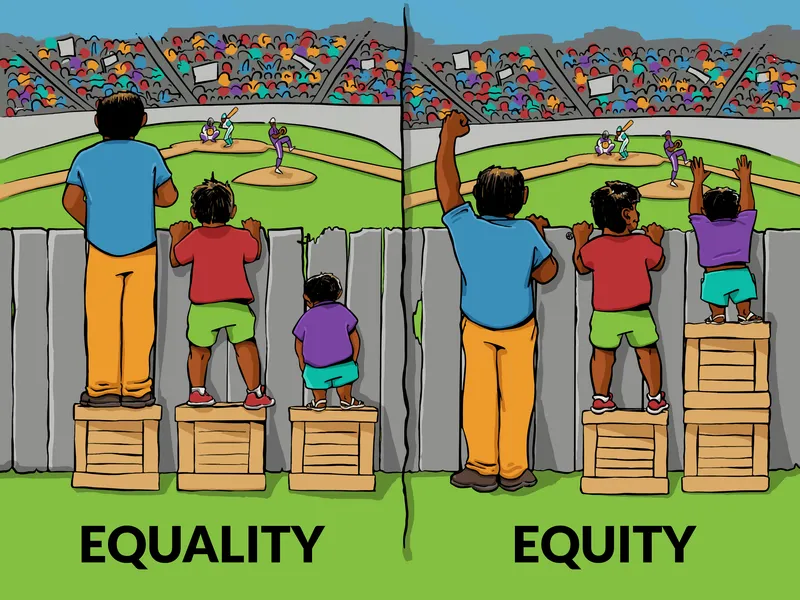
Health Equity and Disparities Reduction
Screening programs must actively address systematic barriers that create 2-3 fold disparities in screening participation and cancer outcomes across racial, ethnic, and socioeconomic groups:
-
Structural Barrier Interventions
- Extended clinic hours including evenings and weekends
- Transportation assistance and childcare support during screening appointments
- Same-day screening and diagnostic services to reduce appointment burden
- Telemedicine consultations for pre-screening education and result discussion
-
Cultural Competency Enhancements
- Bilingual staff and professional interpreters for non-English speakers
- Community partnerships with faith-based organizations and cultural groups
- Peer educators from target communities providing culturally relevant messaging
- Provider training in cultural humility and implicit bias recognition
💡 Master This: Social determinants of health account for 60-80% of health outcomes. Screening programs must address upstream factors including housing stability, food security, and healthcare access to achieve equitable outcomes.
Technology Integration and Digital Health Solutions
Modern screening programs leverage digital technologies to automate processes, improve efficiency, and enhance patient experience:
-
Electronic Health Record Optimization
- Clinical decision support rules identifying screening-eligible patients with >95% accuracy
- Automated order sets for age-appropriate screening with risk stratification
- Results management workflows ensuring timely follow-up of abnormal findings
- Population health analytics tracking screening metrics across patient panels
-
Patient-Facing Digital Tools
- Patient portals with screening reminders and educational resources
- Mobile applications for appointment scheduling and result notification
- Text messaging campaigns with personalized screening reminders
- Wearable device integration for continuous health monitoring
⭐ Clinical Pearl: Artificial intelligence can predict screening non-adherence with 85-90% accuracy using electronic health record data, enabling targeted interventions for high-risk patients. Machine learning algorithms optimize outreach timing and messaging content.
Quality Measurement and Continuous Improvement
Screening program excellence requires comprehensive measurement systems that track process, outcome, and equity metrics:
-
Process Quality Indicators
- Screening participation rates by age, race, ethnicity, insurance status
- Time to diagnostic resolution for abnormal screening results (<30 days target)
- Patient satisfaction scores with screening experience
- Provider adherence to evidence-based guidelines
-
Outcome Quality Indicators
- Cancer detection rates and stage distribution in screened populations
- Interval cancer rates between screening examinations
- False positive rates and unnecessary procedures
- Cost-effectiveness ratios with annual updates
💡 Master This: Balanced scorecards integrate clinical quality, patient experience, operational efficiency, and financial performance metrics. Statistical process control methods identify special cause variation requiring targeted interventions.
Sustainability and Scale-Up Strategies
Long-term screening program success requires sustainable financing, workforce development, and continuous adaptation to changing evidence and population needs:
-
Financial Sustainability Models
- Value-based payment contracts linking screening performance to quality bonuses
- Shared savings programs capturing downstream cost reductions from early detection
- Grant funding for pilot programs with transition to operational funding
- Public-private partnerships leveraging community resources
-
Workforce Development and Training
- Competency-based training for screening coordinators and patient navigators
- Continuing education requirements for screening providers
- Leadership development for quality improvement champions
- Succession planning ensuring program continuity
⭐ Clinical Pearl: Successful screening programs demonstrate return on investment within 3-5 years through reduced treatment costs and improved outcomes. Business case development requires comprehensive cost-benefit analysis including indirect benefits.
Connect implementation excellence through outcome evaluation to understand how systematic screening programs translate into measurable population health improvements and healthcare value creation.
🎯 Implementation Excellence: The Screening System Architecture
Practice Questions: Screening guidelines
Test your understanding with these related questions
A scientist in Chicago is studying a new blood test to detect Ab to EBV with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity much greater than what she had originally hoped for. She travels to China to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with EBV. The scientist tests these 1,200 patients' blood and finds that only 120 of them tested negative with her new exam. Of the patients who are known to be EBV-free, only 20 of them tested positive. Given these results, which of the following correlates with the exam's specificity?











