Thorax/Abdomen

On this page
🏗️ Thoracoabdominal Architecture: The Body's Engineering Marvel
You'll master the thorax and abdomen as interconnected systems where architecture dictates function, breathing synchronizes with circulation, and symptoms reveal patterns that guide diagnosis. This lesson builds your clinical reasoning from structural foundations through respiratory-cardiovascular integration to systematic differential diagnosis, equipping you to recognize emergent conditions, apply evidence-based treatments, and synthesize multi-organ physiology into confident bedside decisions.
📌 Remember: THORAX-ABDOMEN - Thoracic cavity above, Heart in mediastinum, Organs protected by ribs, Respiratory structures, Abdominal cavity below, Xiphoid process landmark, Aorta traverses both, Breathing moves diaphragm, Digestive organs below, Outlet pelvis, Mediastinum central, Entire system coordinated, Nerves supply all regions
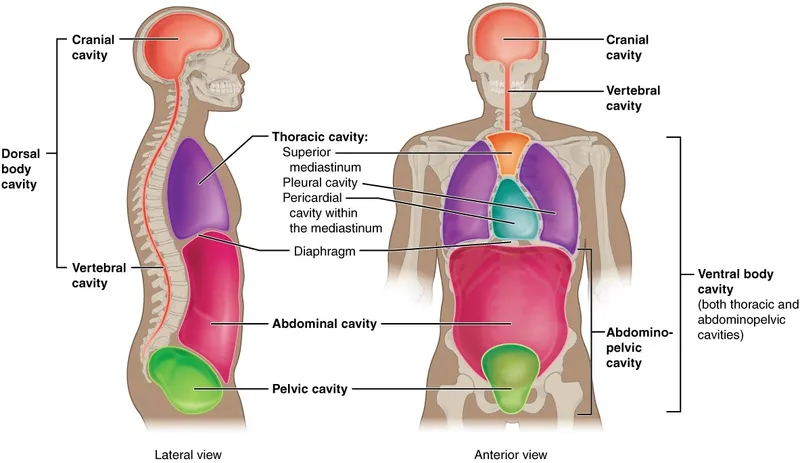
The thoracic cavity extends from the thoracic inlet (T1 level) to the diaphragm (T12-L1), containing 2 pleural cavities, 1 mediastinum, and 1 pericardial cavity. The abdominal cavity spans from diaphragm to pelvic inlet, housing peritoneal and retroperitoneal spaces with 9 anatomical regions for systematic examination.
- Thoracic Boundaries
- Superior: Thoracic inlet - T1, first ribs, manubrium
- Inferior: Diaphragm - T12-L1 vertebral levels
- Anterior: Sternum and costal cartilages - 12 pairs
- Posterior: Thoracic vertebrae - T1-T12 with ribs
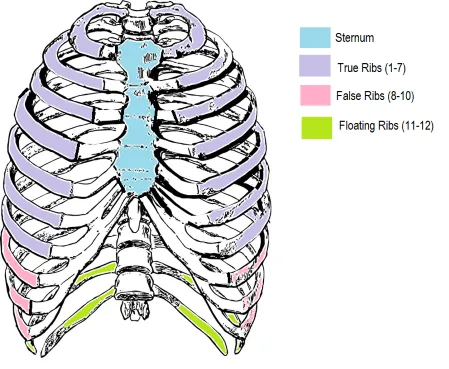
- True ribs: 1-7 (connect directly to sternum)
- False ribs: 8-12 (indirect or no sternal connection)
- Floating ribs: 11-12 (no anterior attachment)
| Cavity | Boundaries | Contents | Pressure | Clinical Significance |
|---|---|---|---|---|
| Thoracic | T1-T12, ribs, sternum | Heart, lungs, great vessels | -5 to -8 mmHg | Pneumothorax, hemothorax |
| Pleural | Visceral/parietal pleura | Lungs, pleural fluid | -5 mmHg | Pleural effusion |
| Mediastinal | Sternum to vertebrae | Heart, vessels, esophagus | Variable | Mass effect syndromes |
| Abdominal | Diaphragm to pelvis | GI organs, liver, spleen | +5 to +7 mmHg | Compartment syndrome |
| Peritoneal | Peritoneum boundaries | Intraperitoneal organs | Subatmospheric | Peritonitis, ascites |
💡 Master This: Anatomical position defines all directional relationships - superior/inferior, anterior/posterior, medial/lateral - with the diaphragm serving as the primary landmark separating thoracic from abdominal viscera at T12-L1 level.
Understanding thoracoabdominal organization provides the foundation for recognizing how respiratory mechanics coordinate with cardiovascular dynamics to maintain optimal organ perfusion across both compartments.
🏗️ Thoracoabdominal Architecture: The Body's Engineering Marvel
⚙️ Respiratory-Cardiovascular Integration: The Synchronized Engine
📌 Remember: DIAPHRAGM MECHANICS - Descends in inspiration, Increases thoracic volume, Air flows inward, Pressure gradient created, Heart filling enhanced, Returns upward in expiration, Abdominal pressure rises, Gas exchange optimized, Mechanical coupling essential
- Respiratory Mechanics Integration
- Diaphragmatic excursion: 3-5 cm normal breathing, 8-10 cm deep inspiration
- Intrathoracic pressure: -5 mmHg expiration to -8 mmHg inspiration
- Venous return enhancement: 30-40% increase during inspiration
- Inferior vena cava: Compressed by diaphragm during inspiration
- Superior vena cava: Enhanced flow with negative thoracic pressure
- Cardiac preload: Optimized through respiratory-cardiac coupling
| Phase | Diaphragm | Thoracic Pressure | Abdominal Pressure | Venous Return | Cardiac Output |
|---|---|---|---|---|---|
| Inspiration | Descends 3-5cm | -8 mmHg | +10 mmHg | ↑ 40% | ↑ 15% |
| Expiration | Ascends 3-5cm | -5 mmHg | +5 mmHg | Baseline | Baseline |
| Deep Inspiration | Descends 8-10cm | -12 mmHg | +15 mmHg | ↑ 60% | ↑ 25% |
| Forced Expiration | Ascends rapidly | +5 mmHg | +20 mmHg | ↓ 20% | ↓ 10% |
| Valsalva | Fixed position | +40 mmHg | +50 mmHg | ↓ 70% | ↓ 50% |
💡 Master This: The thoracoabdominal pressure relationship drives venous return optimization - understanding this mechanism predicts cardiovascular responses to respiratory pathology, mechanical ventilation, and surgical positioning.
This respiratory-cardiovascular integration establishes the foundation for understanding how pathological processes in either compartment create predictable clinical patterns through shared anatomical relationships.
⚙️ Respiratory-Cardiovascular Integration: The Synchronized Engine
🎯 Clinical Pattern Recognition: The Diagnostic Framework
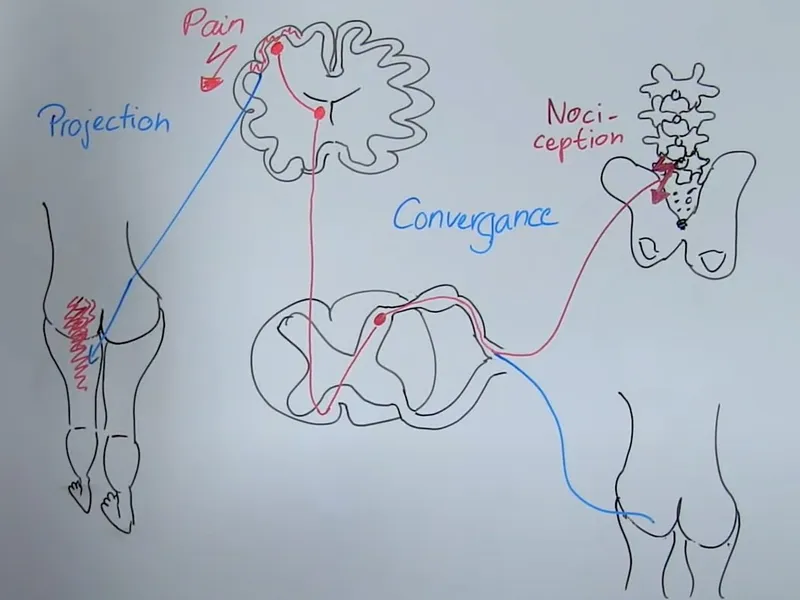
📌 Remember: PAIN PATTERNS - Phrenic nerve C3-C5 (shoulder pain), Angina radiates left arm, Inferior MI diaphragmatic irritation, Nausea with visceral pain, Peritoneal irritation localizes, Appendix McBurney's point, Thoracic pain band-like, Tension pneumothorax shifts mediastinum, Esophageal pain substernal, Renal colic flank to groin, Nerve distributions predict patterns, Somatic vs visceral differences
- Systematic Clinical Assessment Framework
- Inspection: Respiratory rate 12-20/min, chest wall symmetry, abdominal contour
- Palpation: Tactile fremitus, organ borders, tenderness patterns
- Percussion: Lung resonance, liver span 6-12 cm, spleen dullness
- Auscultation: Breath sounds, heart sounds, bowel sounds
- Normal breath sounds: Vesicular over lung fields
- Cardiac auscultation: 4 standard areas plus additional points
- Bowel sounds: 5-35 per minute normal frequency
| Region | Primary Organs | Pain Character | Radiation Pattern | Associated Symptoms |
|---|---|---|---|---|
| Chest | Heart, lungs, esophagus | Crushing, sharp, burning | Left arm, jaw, back | SOB, diaphoresis |
| Epigastric | Stomach, pancreas, heart | Gnawing, boring | Back, shoulders | Nausea, vomiting |
| RUQ | Liver, gallbladder | Colicky, constant | Right shoulder | Jaundice, fever |
| LUQ | Spleen, stomach | Sharp, dull | Left shoulder | Early satiety |
| Periumbilical | Small bowel, early appendix | Crampy, diffuse | No specific pattern | Nausea, vomiting |
💡 Master This: Visceral pain is poorly localized and dull, while somatic pain is sharp and well-localized - this distinction reflects different innervation patterns and guides diagnostic approach in 90% of presentations.
Understanding these clinical patterns enables systematic differentiation between life-threatening and benign conditions through anatomically-based assessment protocols.
🎯 Clinical Pattern Recognition: The Diagnostic Framework
🔬 Systematic Discrimination: The Differential Matrix
📌 Remember: EMERGENCY DISCRIMINATION - ECG changes distinguish cardiac, Mediastinal shift with tension pneumothorax, Elevated enzymes organ-specific, Radiographic patterns characteristic, Guarding suggests peritonitis, Echo shows cardiac tamponade, Nausea with visceral pathology, Cyanosis indicates respiratory, Yellow sclera suggests hepatic
- Quantitative Discrimination Parameters
- Cardiac markers: Troponin >0.04 ng/mL indicates myocardial injury
- Respiratory parameters: O2 sat <90% suggests significant pathology
- Hemodynamic thresholds: BP <90 systolic indicates shock
- Laboratory discrimination: WBC >15,000 suggests infection/inflammation
- Amylase >300 U/L: Pancreatic pathology likely
- Bilirubin >3 mg/dL: Hepatobiliary obstruction
- Lactate >4 mmol/L: Tissue hypoperfusion
| Condition | Pain Character | Key Diagnostic | Time Course | Mortality Risk | Treatment Priority |
|---|---|---|---|---|---|
| STEMI | Crushing substernal | ST elevation | <6 hours | 10-15% | PCI <90 min |
| Tension Pneumothorax | Sharp, unilateral | Mediastinal shift | Minutes | >50% | Needle decompression |
| Aortic Dissection | Tearing, back | Widened mediastinum | Hours | 25-30% | BP control |
| Pulmonary Embolism | Pleuritic | D-dimer + CT | Hours-days | 15-20% | Anticoagulation |
| Perforated Viscus | Sudden, severe | Free air | Hours | 20-40% | Surgical repair |
💡 Master This: Time-sensitive discrimination saves lives - STEMI requires PCI within 90 minutes, tension pneumothorax needs immediate decompression, and aortic dissection demands BP control within 20 minutes for optimal outcomes.
This systematic discrimination framework enables rapid, accurate diagnosis while minimizing unnecessary testing and optimizing treatment timing for life-threatening conditions.
🔬 Systematic Discrimination: The Differential Matrix
⚡ Treatment Algorithms: The Evidence-Based Response
Treatment algorithms integrate anatomical knowledge with evidence-based protocols to optimize patient outcomes. Timing thresholds, quantitative endpoints, and anatomical considerations guide therapeutic decision-making with measurable success rates.
📌 Remember: TREATMENT PRIORITIES - Time-sensitive interventions first, Respiratory support immediate, ECG monitoring continuous, Access vascular early, Thoracic decompression urgent, Medications evidence-based, Endoscopy when indicated, Neurovascular assessment, Trends monitor closely
- Evidence-Based Treatment Protocols
- STEMI management: Door-to-balloon <90 minutes achieves 95% success rate
- Tension pneumothorax: Needle decompression followed by chest tube within 5 minutes
- Cardiac tamponade: Pericardiocentesis with echo guidance has >90% success
- Aortic dissection: Beta-blocker first, then ACE inhibitor to SBP 100-120 mmHg
- Type A: Surgical repair within 24 hours reduces mortality to 15%
- Type B: Medical management unless complications develop
- Blood pressure control: Target SBP 100-120 mmHg within 20 minutes
| Intervention | Time Target | Success Rate | Mortality Reduction | Key Anatomical Consideration |
|---|---|---|---|---|
| PCI for STEMI | <90 minutes | 95% | 50% vs medical | Coronary anatomy |
| Chest tube | <15 minutes | 90% | 80% vs delay | Pleural space anatomy |
| Pericardiocentesis | <30 minutes | 85% | 70% vs delay | Pericardial anatomy |
| Emergency surgery | <60 minutes | 80% | 60% vs delay | Surgical approach |
| Thrombolysis | <3 hours | 75% | 40% vs delay | Vascular distribution |
💡 Master This: Anatomical landmarks guide emergency procedures - 2nd intercostal space midclavicular line for needle decompression, 5th intercostal space anterior axillary line for chest tube, and subxiphoid approach for pericardiocentesis with echo guidance.
Understanding treatment algorithms enables rapid, evidence-based intervention while minimizing complications through anatomically-guided procedures and protocol adherence.
⚡ Treatment Algorithms: The Evidence-Based Response
🌐 Multi-System Integration: The Physiological Network
System integration occurs through anatomical continuity, shared innervation, and physiological interdependence. Understanding these integration patterns reveals how pathology in one system creates predictable effects in related systems through anatomical and physiological connections.
📌 Remember: SYSTEM INTEGRATION - Sympathetic nervous system coordinates, Yield cardiovascular responses, Splanchnic circulation adjusts, Thoracic pressure affects venous return, Endocrine signals integrate, Metabolic demands drive changes, Innervation patterns overlap, Neural reflexes coordinate, Timing synchronizes systems, Equilibrium maintains homeostasis, Global responses to local changes, Regulation through feedback, Adaptation to stress, Tissue perfusion optimized, Interconnected function, Organ system cooperation, Network effects amplify
- Integration Mechanisms and Pathways
- Autonomic nervous system: Sympathetic T1-L2, parasympathetic vagus nerve
- Vascular integration: Splanchnic circulation receives 25% cardiac output
- Respiratory-cardiac coupling: Heart rate variability with respiratory cycle
- Neuroendocrine coordination: Stress response affects all systems simultaneously
- Sympathetic activation: ↑ HR 20-40%, ↑ BP 10-20%, ↓ GI motility 50%
- Parasympathetic dominance: ↓ HR 10-20%, ↑ GI secretions 200%
- Stress hormones: Cortisol, epinephrine affect multiple organ systems
| System | Primary Function | Integration Points | Stress Response | Failure Consequences |
|---|---|---|---|---|
| Cardiovascular | Oxygen delivery | Autonomic control | ↑ CO 50-100% | Shock, organ failure |
| Respiratory | Gas exchange | Medullary control | ↑ RR 100-200% | Hypoxia, acidosis |
| Digestive | Nutrient processing | Enteric nervous system | ↓ Function 70% | Malnutrition, ileus |
| Nervous | Coordination | Central integration | ↑ Activity 300% | Loss of coordination |
| Endocrine | Hormonal control | Feedback loops | ↑ Stress hormones | Metabolic dysfunction |
💡 Master This: Multi-system failure follows predictable patterns - cardiogenic shock leads to respiratory failure within 30-60 minutes, sepsis causes cardiovascular collapse in 40-60% of cases, and respiratory failure triggers cardiac arrhythmias in 25-35% of patients.
This multi-system integration understanding enables anticipation of secondary complications and proactive management of system-wide physiological responses to primary pathology.
🌐 Multi-System Integration: The Physiological Network
🎯 Clinical Mastery Arsenal: The Rapid Reference Toolkit
📌 Remember: MASTERY ESSENTIALS - Master anatomical landmarks, Assess systematically always, Standardize your approach, Time-sensitive priorities, Evidence-based decisions, Recognize patterns quickly, Yield to protocols proven, Evaluate outcomes continuously, Synthesis of knowledge, Skill through repetition, Expertise builds confidence, Never stop learning, Teach others effectively, Integrate new evidence, Adaptability essential, Lifelong commitment, Systematic excellence
- Essential Clinical Thresholds
- Vital sign red flags: SBP <90, HR >120, RR >30, O2 sat <90%
- Laboratory critical values: Troponin >0.04, Lactate >4, WBC >20,000
- Imaging priorities: Chest X-ray within 15 minutes, CT within 60 minutes
- Time-sensitive interventions: PCI <90 min, antibiotics <60 min, surgery <120 min
- Golden hour: Trauma surgery within 60 minutes reduces mortality 40%
- Door-to-needle: Thrombolysis within 30 minutes improves outcomes 25%
- Recognition-to-treatment: Sepsis protocols within 60 minutes reduce mortality 30%
| Clinical Scenario | Key Assessment | Critical Threshold | Immediate Action | Success Metric |
|---|---|---|---|---|
| Chest Pain | ECG + Troponin | ST elevation | Activate cath lab | PCI <90 min |
| Shortness of Breath | O2 sat + CXR | Sat <90% | Oxygen + workup | Sat >95% |
| Abdominal Pain | Exam + Labs | Peritoneal signs | Surgical consult | OR <2 hours |
| Hypotension | Fluid + Pressors | SBP <90 | Resuscitation | MAP >65 |
| Respiratory Distress | ABG + CXR | pH <7.30 | Ventilatory support | pH >7.35 |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | ||||
| flowchart TD |
Start["👤 Patient Intake
• Clinical arrival• Initial symptoms"]
Assess["📋 Primary Assessment
• Vital signs• Physical exam"]
Decision{"⚠️ Life Threatening?
• Evaluate ABCs• Severity check"}
Intervention["💊 Fast Intervention
• Acute care• Resus protocol"]
Stabilize["⚠️ Stabilize
• Airway management• BP maintenance"]
Systematic["📋 Clinical Eval
• Detailed history• Focused review"]
Workup["🔬 Lab Workup
• Imaging tests• Blood panels"]
Treat["💊 Definitive Care
• Specific therapy• Target pathology"]
Monitor["👁️ Monitor Progress
• Track recovery• Follow up care"]
Start --> Assess Assess --> Decision Decision -->|Yes| Intervention Decision -->|No| Systematic Intervention --> Stabilize Systematic --> Workup Stabilize --> Treat Workup --> Treat Treat --> Monitor
style Start fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Assess fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Decision fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style Intervention fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Stabilize fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style Systematic fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Workup fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Treat fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Monitor fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1
> ⭐ **Clinical Pearl**: **Pattern recognition** improves with **deliberate practice** - **expert clinicians** recognize **diagnostic patterns** within **30 seconds** of **patient encounter**, achieving **diagnostic accuracy >90%** through **systematic assessment** and **knowledge integration**.
> 💡 **Master This**: **Clinical excellence** requires **continuous integration** of **anatomical knowledge**, **physiological understanding**, and **evidence-based protocols** - **master these foundations**, and **complex clinical decisions** become **systematic**, **reproducible**, and **consistently successful**.
🎯 Clinical Mastery Arsenal: The Rapid Reference Toolkit
Practice Questions: Thorax/Abdomen
Test your understanding with these related questions
A 72-year-old man presents to the emergency department after a fall. The patient was found lying down on the floor in his room in his retirement community. The patient has a past medical history of Alzheimer dementia and a prosthetic valve. His current medications include donepezil and warfarin. His temperature is 97.7°F (36.5°C), blood pressure is 85/50 mmHg, pulse is 160/min, respirations are 13/min, and oxygen saturation is 97% on room air. The patient is started on IV fluids and a type and screen is performed. Laboratory values are ordered as seen below. Hemoglobin: 13 g/dL Hematocrit: 39% Leukocyte count: 5,500 cells/mm^3 with normal differential Platelet count: 225,000/mm^3 INR: 2.5 AST: 10 U/L ALT: 12 U/L A chest radiograph and EKG are performed and are within normal limits. A full physical exam is within normal limits. The patient's vitals are repeated. His temperature is 99.5°F (37.5°C), blood pressure is 110/70 mmHg, pulse is 90/min, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?











