Wound assessment techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Wound assessment techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Wound assessment techniques US Medical PG Question 1: A family doctor in a rural area is treating a patient for dyspepsia. The patient had chronic heartburn and abdominal pain for the last 2 months and peptic ulcer disease due to a suspected H. pylori infection. For reasons relating to affordability and accessibility, the doctor decides to perform a diagnostic test in the office that is less invasive and more convenient. Which of the following is the most likely test used?
- A. Steiner's stain
- B. Culture of organisms from gastric specimen
- C. Stool antigen test (Correct Answer)
- D. Detection of the breakdown products of urea in biopsy
- E. Serology (ELISA testing)
Wound assessment techniques Explanation: ***Stool antigen test***
- This **non-invasive** and **cost-effective** test detects *H. pylori* antigens in stool, making it suitable for a rural setting with limited resources.
- It is highly sensitive and specific, useful for both initial diagnosis and confirming eradication after treatment.
*Steiner's stain*
- **Steiner's stain** (Steiner silver stain) is primarily used for histological visualization of *Legionella* species, and **not for** *H. pylori* detection in routine clinical practice.
- It requires an **endoscopic biopsy**, making it more invasive and costly than the stool antigen test.
*Culture of organisms from gastric specimen*
- This method requires an **endoscopic biopsy** and specialized culture facilities, which may not be available in a rural doctor's office.
- It is more expensive and time-consuming, and primarily used when **antibiotic resistance** is suspected.
*Detection of the breakdown products of urea in biopsy*
- This refers to the **rapid urease test** (e.g., CLOtest), which is performed on a **gastric biopsy** obtained during endoscopy.
- While quick, it is an **invasive procedure** requiring endoscopy, which contradicts the patient's and doctor's preferences for a less invasive test.
*Serology (ELISA testing)*
- **Serology** detects antibodies to *H. pylori* but cannot differentiate between **active infection** and **past exposure**.
- Its utility in monitoring eradication is limited, and it's generally not recommended as the primary diagnostic test due to its inability to confirm active infection.
Wound assessment techniques US Medical PG Question 2: A 56-year-old woman undergoes open reduction and internal fixation of the distal tibia 1 day after a fall. She has had rheumatoid arthritis for 12 years and diabetes mellitus for 2 years. Her medications over the past year have included metformin, prednisone, calcium supplements, and methotrexate. Prior to surgery, insulin was added to her medications, and the dose of prednisone was increased. She has had appropriate nutrition over the years with regular follow-ups with her healthcare professional. Which of the following is the most appropriate supplement to prevent wound failure in this patient?
- A. Glutamine
- B. Zinc
- C. Vitamin A
- D. Arginine
- E. Vitamin C (Correct Answer)
Wound assessment techniques Explanation: ***Vitamin C***
- This patient is at high risk for **wound healing complications** due to her comorbidities (diabetes, rheumatoid arthritis) and medications (prednisone, methotrexate). **Vitamin C** (ascorbic acid) is essential for **collagen synthesis** and cross-linking, which is crucial for wound strength and tissue repair.
- While other options play a role in wound healing, Vitamin C is particularly important in patients with **impaired healing** due to chronic inflammation, corticosteroid use, and metabolic disorders, as it counteracts their negative effects on collagen formation.
*Glutamine*
- **Glutamine** is an important fuel for rapidly dividing cells, including immune cells and fibroblasts, and can be beneficial in catabolic states.
- However, its role in directly counteracting the specific challenges of this patient's wound healing (corticosteroid use, diabetes, rheumatoid arthritis) is **less direct** compared to Vitamin C's role in collagen synthesis.
*Zinc*
- **Zinc** is a cofactor for numerous enzymes involved in cell proliferation, immune function, and collagen synthesis.
- While important, zinc deficiency is not explicitly indicated, and its role as a primary intervention to prevent wound failure in a patient with **prednisone-induced healing impairment** is secondary to vitamin C.
*Vitamin A*
- **Vitamin A** can help reverse the negative effects of **corticosteroids** on wound healing by promoting epithelialization and collagen synthesis.
- While relevant due to prednisone use, its overall importance in **collagen formation** and direct wound strength is not as profound or broad as Vitamin C.
*Arginine*
- **Arginine** is a precursor for nitric oxide, which improves blood flow to wounds, and is involved in collagen formation and immune function.
- Although beneficial for wound healing, particularly in critically ill patients, it is **not the most appropriate single supplement** for addressing the specific collagen synthesis impairment seen in this patient's context of corticosteroid use and chronic disease.
Wound assessment techniques US Medical PG Question 3: A 30-year-old woman dies shortly after admission to the emergency department. The family requests an autopsy to determine cause of death. During the autopsy, multiple linear, parallel marks are noted across her wrists. Which of the following patterns suggests these are hesitation marks rather than defensive wounds?
- A. Irregular, scattered marks
- B. Diagonal, deep lacerations
- C. Deep, single cuts
- D. Superficial, parallel cuts (Correct Answer)
Wound assessment techniques Explanation: ***Superficial, parallel cuts***
- **Hesitation marks** are typically numerous, **superficial**, and **parallel**, reflecting a tentative or indecisive attempt and often made in the same direction.
- They tend to be concentrated in an area of the body chosen for self-harm, such as the wrists, and are usually consistent with a non-fatal intent.
*Irregular, scattered marks*
- This pattern is more indicative of **defensive wounds**, which are often scattered and irregular due to attempts to ward off an attack.
- Defensive wounds are typically found on the palms, forearms, and other areas used for protection.
*Diagonal, deep lacerations*
- **Deep lacerations**, especially if diagonal and singular, are less characteristic of hesitation marks and more suggestive of a determined attempt to inflict fatal injury or could be defensive.
- **Hesitation marks** are typically not aimed at quickly causing fatal harm.
*Deep, single cuts*
- A single, **deep cut** is often associated with a resolute intent to cause significant injury or death, rather than the hesitant, superficial nature of hesitation marks.
- This pattern would warrant further investigation into the intent and circumstances surrounding the injury.
Wound assessment techniques US Medical PG Question 4: A 45-year-old man comes to his primary care provider for a routine visit. The patient mentions that while he was cooking 5 days ago, he accidentally cut himself with a meat cleaver and lost the skin at the tip of his finger. After applying pressure and ice, the bleeding stopped and he did not seek treatment. The patient is otherwise healthy and does not take any daily medications. The patient’s temperature is 98.2°F (36.8°C), blood pressure is 114/72 mmHg, pulse is 60/min, and respirations are 12/min. On exam, the patient demonstrates a 0.5 x 0.3 cm wound on the tip of his left third finger. No bone is involved, and the wound is red, soft, and painless. There are no signs of infection. Which of the following can be expected on histopathological examination of the wounded area?
- A. Platelet aggregates
- B. Epithelial cell migration from the wound borders
- C. Neutrophil migration into the wound
- D. Deposition of type III collagen (Correct Answer)
- E. Deposition of type I collagen
Wound assessment techniques Explanation: ***Deposition of type III collagen***
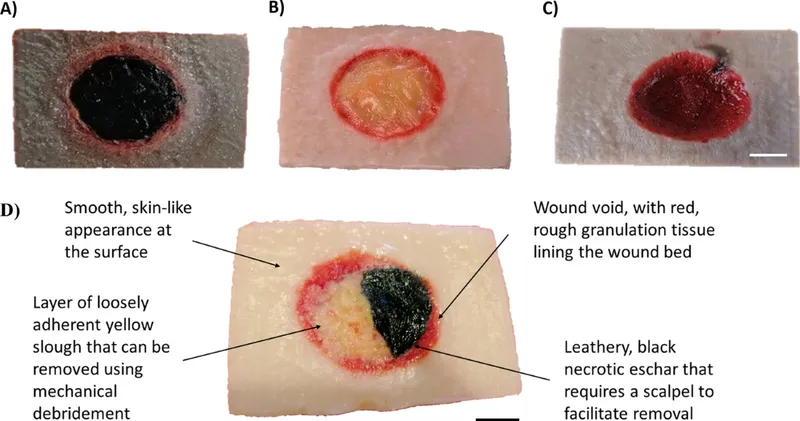
- Five days post-injury, the **proliferative phase of wound healing** is active, characterized by the formation of an initial **granulation tissue** matrix primarily composed of **Type III collagen**.
- This type of collagen forms thinner, more flexible fibers that provide a temporary scaffold for tissue regeneration before being gradually replaced by stronger Type I collagen.
*Platelet aggregates*
- **Platelet aggregation** occurs immediately after injury as part of **hemostasis**, forming a plug to stop bleeding.
- By five days, this initial phase would have concluded, and the primary focus would be on tissue repair and regeneration.
*Epithelial cell migration from the wound borders*
- **Epithelial cell migration** for re-epithelialization typically occurs within the first 24-48 hours after injury, forming a new epidermal layer over the wound.
- While it continues, the dominant histological feature at day 5 in an open wound of this size would be **granulation tissue formation** in the dermis.
*Neutrophil migration into the wound*
- **Neutrophil migration** is a hallmark of the **inflammatory phase**, peaking within 24-48 hours post-injury to clear debris and microbes.
- By day 5, the inflammatory phase would be subsiding, and macrophages would be more prevalent, signaling the transition to the proliferative phase.
*Deposition of type I collagen*
- **Type I collagen** is the predominant collagen found in mature scar tissue and is deposited during the later **remodeling phase** of wound healing.
- While some Type I collagen may be present, **Type III collagen** is characteristic of the early granulation tissue prominent at day 5.
Wound assessment techniques US Medical PG Question 5: A 60-year-old man presents with pain, swelling, and a purulent discharge from his left foot. He says that the symptoms began 7 days ago with mild pain and swelling on the medial side of his left foot, but have progressively worsened. He states that there has been a foul-smelling discharge for the past 2 days. The medical history is significant for type 2 diabetes mellitus that was diagnosed 10 years ago and is poorly managed, and refractory peripheral artery disease that failed revascularization 6 months ago. The current medications include aspirin (81 mg orally daily) and metformin (500 mg orally twice daily). He has a 20-pack-year smoking history but quit 6 months ago. The family history is significant for type 2 diabetes mellitus in both parents and his father died of a myocardial infarction at 50 years of age. His temperature is 38.9°C (102°F); blood pressure 90/65 mm Hg; pulse 102/min; respiratory rate 22/min; and oxygen saturation 99% on room air. On physical examination, he appears ill and diaphoretic. The skin is flushed and moist. There is 2+ pitting edema of the left foot with blistering and black discoloration (see picture). The lower legs are hairless and the lower extremity peripheral pulses are 1+ bilaterally. Laboratory tests are pending. Blood cultures are positive for Staphylococcus aureus. Which of the following findings is the strongest indication for amputation of the left lower extremity in this patient?
- A. Presence of wet gangrene (Correct Answer)
- B. Positive blood cultures
- C. Diminished peripheral pulses
- D. Poorly managed blood glucose
- E. Smoking history
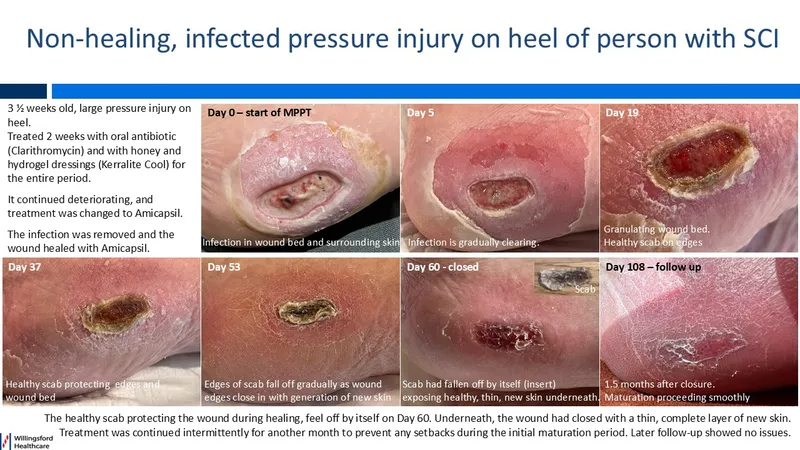
Wound assessment techniques Explanation: ***Presence of wet gangrene***
- The presence of **wet gangrene**, evidenced by black discoloration, blistering, and purulent discharge, indicates widespread tissue necrosis and severe infection.
- Wet gangrene progresses rapidly and is associated with a high risk of **sepsis** and mortality, often necessitating amputation to save the patient's life.
*Positive blood cultures*
- While positive blood cultures for **Staphylococcus aureus** indicate a serious infection, they do not, by themselves, directly necessitate amputation.
- They guide antibiotic therapy but do not confirm the extent of tissue damage (e.g., gangrene) that mandates amputation.
*Diminished peripheral pulses*
- **Diminished peripheral pulses** (1+ bilaterally) suggest peripheral artery disease, which contributes to poor wound healing and infection risk.
- However, poor circulation alone is not an immediate indication for amputation; the presence of irreversible tissue death (gangrene) is the critical factor.
*Poorly managed blood glucose*
- **Poorly managed diabetes** is a significant risk factor for peripheral neuropathy, impaired immunity, and vascular disease, predisposing to foot infections.
- While it contributes to the overall severity and complexity of the patient's condition, it is not an acute indication for amputation.
*Smoking history*
- A **20-pack-year smoking history** contributes to vascular disease and impaired wound healing, increasing the risk for foot complications.
- This is a long-term risk factor and contributor to the patient's overall health status, but not an immediate surgical indication for amputation itself.
Wound assessment techniques US Medical PG Question 6: A previously healthy 5-year-old boy is brought to the emergency department 15 minutes after sustaining an injury to his right hand. His mother says that she was cleaning the bathroom when he accidentally knocked over the drain cleaner bottle and spilled the liquid onto his hand. On arrival, he is crying and holding his right hand in a flexed position. His temperature is 37.7°C (99.8°F), pulse is 105/min, respirations are 25/min, and blood pressure is 105/65 mm Hg. Examination of the right hand shows a 4 x 4 cm area of reddened, blistered skin. The area is very tender to light touch. His ability to flex and extend the right hand are diminished. Radial pulses are palpable. Capillary refill time is less than 3 seconds. Which of the following is the most appropriate next step in management?
- A. Irrigate with water (Correct Answer)
- B. Apply split-thickness skin graft
- C. Apply silver sulfadiazine
- D. Apply mineral oil
- E. Perform escharotomy
Wound assessment techniques Explanation: ***Irrigate with water***
- The immediate and most crucial step for a **chemical burn** is copious **irrigation with water** to remove the offending agent and prevent further tissue damage.
- This action minimizes the duration of contact between the **corrosive substance** and the skin, halting the chemical reaction.
*Apply split-thickness skin graft*
- A **skin graft** is a surgical procedure typically reserved for **deep burns** and is not the immediate first step for chemical exposure.
- It would be considered later in management if the burn resulted in **full-thickness tissue loss** and incomplete wound healing.
*Apply silver sulfadiazine*
- **Silver sulfadiazine** is an antimicrobial cream used to prevent infection in **thermal burns** after initial wound care.
- It is not indicated as the first line of treatment for a **chemical burn** and would not remove the chemical agent from the skin.
*Apply mineral oil*
- Applying **mineral oil** is not the appropriate initial treatment for a **chemical burn** and could potentially trap the chemical, worsening the injury.
- The priority is to dilute and remove the chemical, which mineral oil cannot do effectively.
*Perform escharotomy*
- An **escharotomy** is a surgical incision through burn eschar used to relieve pressure in **circumferential full-thickness burns** that compromise circulation.
- This procedure is not indicated as the initial management for a **chemical burn** and is only considered for severe, deep burns with vascular compromise.
Wound assessment techniques US Medical PG Question 7: A 15-year-old boy is brought to the emergency department by ambulance after his mother found him having muscle spasms and stiffness in his room. His mother stated he scraped his foot on a rusty razor on the bathroom floor 2 days prior. On presentation, his temperature is 102.0°F (38.9°C), blood pressure is 108/73 mmHg, pulse is 122/min, and respirations are 18/min. On physical exam, he is found to have severe muscle spasms and rigid abdominal muscles. In addition, he has a dirty appearing wound on his right foot. The patient's mother does not recall any further vaccinations since age 12. Finally, he is found to have difficulty opening his mouth so he is intubated. Which of the following treatment(s) should be provided to this patient?
- A. Wound debridement and antitoxin
- B. Antitoxin
- C. Wound debridement
- D. Wound debridement and booster vaccine
- E. Wound debridement, antitoxin, and booster vaccine (Correct Answer)
Wound assessment techniques Explanation: ***Wound debridement, antitoxin, and booster vaccine***
- The patient presents with classic symptoms of **tetanus** (muscle spasms, stiffness, trismus, fever) following a contaminated wound, and an uncertain vaccination history.
- **Wound debridement** removes the source of toxin production, **antitoxin** (tetanus immune globulin) neutralizes circulating toxin, and a **booster vaccine** provides active immunity against future infections.
*Wound debridement and antitoxin*
- While **wound debridement** and **antitoxin** are critical for acute management, omitting the booster vaccine leaves the patient vulnerable to future tetanus infections.
- A booster dose is essential to stimulate the patient's own immune system and provide **long-term immunity**, especially with a history of unknown vaccination status.
*Antitoxin*
- Administering only **antitoxin** would neutralize circulating toxins but would not address the ongoing production of toxins from the contaminated wound.
- It also wouldn't provide **active immunization** to protect against future exposures.
*Wound debridement*
- **Wound debridement** alone removes the bacterial source but does not neutralize the already circulating **tetanus toxin**, which is responsible for the severe neurological symptoms.
- It also fails to provide immediate passive immunity with antitoxin or active immunization with a booster.
*Wound debridement and booster vaccine*
- This option correctly addresses removing the source and providing active immunity but critically misses the immediate need for **antitoxin** to neutralize existing toxins and alleviate the life-threatening symptoms.
- The **tetanus toxin** acts rapidly, and prompt neutralization is crucial to prevent further neurological damage and improve prognosis.
Wound assessment techniques US Medical PG Question 8: A 37-year-old-woman presents to the emergency room with complaints of fever and abdominal pain. Her blood pressure is 130/74 mmHg, pulse is 98/min, temperature is 101.5°F (38.6°C), and respirations are 23/min. The patient reports that she had a laparoscopic cholecystectomy 4 days ago but has otherwise been healthy. She is visiting her family from Nebraska and just arrived this morning from a 12-hour drive. Physical examination revealed erythema and white discharge from abdominal incisions and tenderness upon palpations at the right upper quadrant. What is the most probable cause of the patient’s fever?
- A. Pulmonary atelectasis
- B. Residual gallstones
- C. Urinary tract infection
- D. Wound infection (Correct Answer)
- E. Pulmonary embolism
Wound assessment techniques Explanation: ***Wound infection***
- The presence of **erythema**, **white discharge from abdominal incisions**, and **fever** 4 days post-laparoscopic cholecystectomy strongly indicates a surgical site infection.
- This is a common complication after surgery, especially with visible signs of local inflammation and purulent discharge.
*Pulmonary atelectasis*
- **Atelectasis** typically presents within **24-48 hours post-op** and usually resolves spontaneously.
- While it can cause fever, the prominent local wound signs and the timing (4 days post-op) make it less likely to be the primary cause of fever.
*Residual gallstones*
- **Residual gallstones** would typically present with symptoms resembling acute cholecystitis or cholangitis, such as **right upper quadrant pain**, **jaundice**, or **elevated liver enzymes**, without direct signs of wound infection.
- These do not account for the **erythema and discharge from the incision sites**.
*Urinary tract infection*
- A **urinary tract infection (UTI)** would present with **dysuria**, **frequency**, **urgency**, or **suprapubic pain**, and would not explain the local wound findings.
- While surgery can increase the risk of nosocomial UTIs, the clinical presentation is primarily focused on the surgical site.
*Pulmonary embolism*
- A **pulmonary embolism (PE)** would likely cause **dyspnea**, **tachycardia**, **hypoxia**, and **pleuritic chest pain**, which are not reported in this case.
- Though prolonged immobility (e.g., long drive) is a risk factor, the specific local signs of infection are not consistent with PE.
Wound assessment techniques US Medical PG Question 9: A 63-year-old man presents to the clinic complaining of burning bilateral leg pain which has been increasing gradually over the past several months. It worsens when he walks but improves with rest. His past medical and surgical history are significant for hypertension, hyperlipidemia, diabetes, and a 40-pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 167/108 mm Hg, pulse is 88/min, respirations are 13/min, and oxygen saturation is 95% on room air. Physical exam of the lower extremities reveals palpable but weak posterior tibial and dorsalis pedis pulses bilaterally. Which of the following is the best initial treatment for this patient's symptoms?
- A. Exercise and smoking cessation (Correct Answer)
- B. Lovenox and atorvastatin
- C. Lisinopril and atorvastatin
- D. Balloon angioplasty with stenting
- E. Femoral-popliteal bypass
Wound assessment techniques Explanation: ***Exercise and smoking cessation***
- This patient presents with symptoms highly suggestive of **peripheral artery disease (PAD)**, characterized by **intermittent claudication** (leg pain worsening with activity and improving with rest), and risk factors like diabetes, hypertension, hyperlipidemia, and smoking.
- **Smoking cessation** is the single most important modifiable risk factor, and a supervised **exercise program** (walking to the point of claudication) is the most effective initial treatment to improve walking distance and quality of life for PAD patients.
*Lovenox and atorvastatin*
- **Atorvastatin** is appropriate for dyslipidemia and cardiovascular risk reduction in PAD patients, but **Lovenox (low molecular weight heparin)** is an anticoagulant typically used for acute thrombotic events or VTE prophylaxis, not initial management of chronic stable claudication.
- While statins are important for secondary prevention, Lovenox does not directly address the primary management of claudication symptoms or underlying atherosclerotic progression in this stable setting.
*Lisinopril and atorvastatin*
- **Lisinopril** is an ACE inhibitor suitable for hypertension, which is important for overall cardiovascular health but not the primary initial treatment for claudication symptoms.
- While both medications address risk factors, they do not directly target the improvement of walking function and symptom relief as effectively as exercise and smoking cessation in the initial phase.
*Balloon angioplasty with stenting*
- Invasive revascularization procedures like **balloon angioplasty with stenting** are typically reserved for patients with more severe symptoms (e.g., rest pain, non-healing ulcers, critical limb ischemia) or those who have failed conservative management like exercise therapy.
- This is not the **best initial treatment** for a patient with stable claudication.
*Femoral-popliteal bypass*
- **Femoral-popliteal bypass** is a surgical revascularization procedure indicated for more severe PAD, particularly in cases of critical limb ischemia or long-segment occlusions that are not amenable to endovascular repair.
- Like angioplasty, it is a more aggressive intervention and not the **initial treatment of choice** for intermittent claudication.
Wound assessment techniques US Medical PG Question 10: A 54-year-old man comes to the physician because of a painful mass in his left thigh for 3 days. He underwent a left lower limb angiography for femoral artery stenosis and had a stent placed 2 weeks ago. He has peripheral artery disease, coronary artery disease, hypercholesterolemia and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 34 years. Current medications include enalapril, aspirin, simvastatin, metformin, and sitagliptin. His temperature is 36.7°C (98°F), pulse is 88/min, and blood pressure is 116/72 mm Hg. Examination shows a 3-cm (1.2-in) tender, pulsatile mass in the left groin. The skin over the area of the mass shows no erythema and is cool to the touch. A loud bruit is heard on auscultation over this area. The remainder of the examination shows no abnormalities. Results of a complete blood count and serum electrolyte concentrations show no abnormalities. Duplex ultrasonography shows an echolucent sac connected to the common femoral artery, with pulsatile and turbulent blood flow between the artery and the sac. Which of the following is the most appropriate next best step in management?
- A. Ultrasound-guided thrombin injection (Correct Answer)
- B. Covered stent implantation
- C. Ultrasound-guided compression
- D. Coil embolization
- E. Schedule surgical repair
Wound assessment techniques Explanation: ***Ultrasound-guided thrombin injection***
- The patient presents with a **post-catheterization pseudoaneurysm** as indicated by the pulsatile, tender mass with a bruit after recent femoral angiography, and confirmed by duplex ultrasonography showing an echolucent sac connected to the common femoral artery with pulsatile flow.
- **Ultrasound-guided thrombin injection** is the preferred treatment for pseudoaneurysms that are larger than 2-3 cm or have been present for more than 1 week, as it effectively closes the pseudoaneurysm sac with a high success rate and minimal invasiveness.
*Covered stent implantation*
- This is a treatment for arterial injury or aneurysm, but it is generally reserved for **larger or more complex pseudoaneurysms**, or those that have failed less invasive treatments, due to its greater invasiveness and potential complications.
- It involves placing a stent graft to exclude the pseudoaneurysm from the circulation.
*Ultrasound-guided compression*
- This technique involves applying sustained pressure to the pseudoaneurysm neck, which can lead to thrombosis. However, it has a **lower success rate** compared to thrombin injection, especially for larger pseudoaneurysms, and is often painful and time-consuming.
- It is often considered a first-line therapy for smaller pseudoaneurysms (<2-3 cm) before thrombin injection, but in this case, the pseudoaneurysm is 3 cm.
*Coil embolization*
- This procedure is typically used to treat **arteriovenous malformations** or high-flow bleeding rather than pseudoaneurysms.
- It involves placing coils into the vessel to induce thrombosis, but carries risks of distal embolization and might be overly aggressive for a femoral pseudoaneurysm.
*Schedule surgical repair*
- **Surgical repair** is indicated for pseudoaneurysms that are rapidly expanding, symptomatic with critical limb ischemia, infected, or those that have failed less invasive treatments.
- In this case, given the patient's stable condition and the availability of less invasive options, surgical repair is not the initial best step.
More Wound assessment techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.