Types of wound closure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Types of wound closure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Types of wound closure US Medical PG Question 1: A 23-year-old man comes to the emergency department with an open wound on his right hand. He states that he got into a bar fight about an hour ago. He appears heavily intoxicated and does not remember the whole situation, but he does recall lying on the ground in front of the bar after the fight. He does not recall any history of injuries but does remember a tetanus shot he received 6 years ago. His temperature is 37°C (98.6°F), pulse is 77/min, and blood pressure is 132/78 mm Hg. Examination shows a soft, nontender abdomen. His joints have no bony deformities and display full range of motion. There is a 4-cm (1.6-in) lesion on his hand with the skin attached only on the ulnar side. The wound, which appears to be partly covered with soil and dirt, is irrigated and debrided by the hospital staff. Minimal erythema and no purulence is observed in the area surrounding the wound. What is the most appropriate next step in management?
- A. Apposition of wound edges under tension + rifampin
- B. Surgical treatment with skin flap + ciprofloxacin
- C. Surgical treatment with skin graft + tetanus vaccine
- D. Tension-free apposition of wound edges + sterile dressing
- E. Application of moist sterile dressing + tetanus vaccine (Correct Answer)
Types of wound closure Explanation: ***Application of moist sterile dressing + tetanus vaccine***
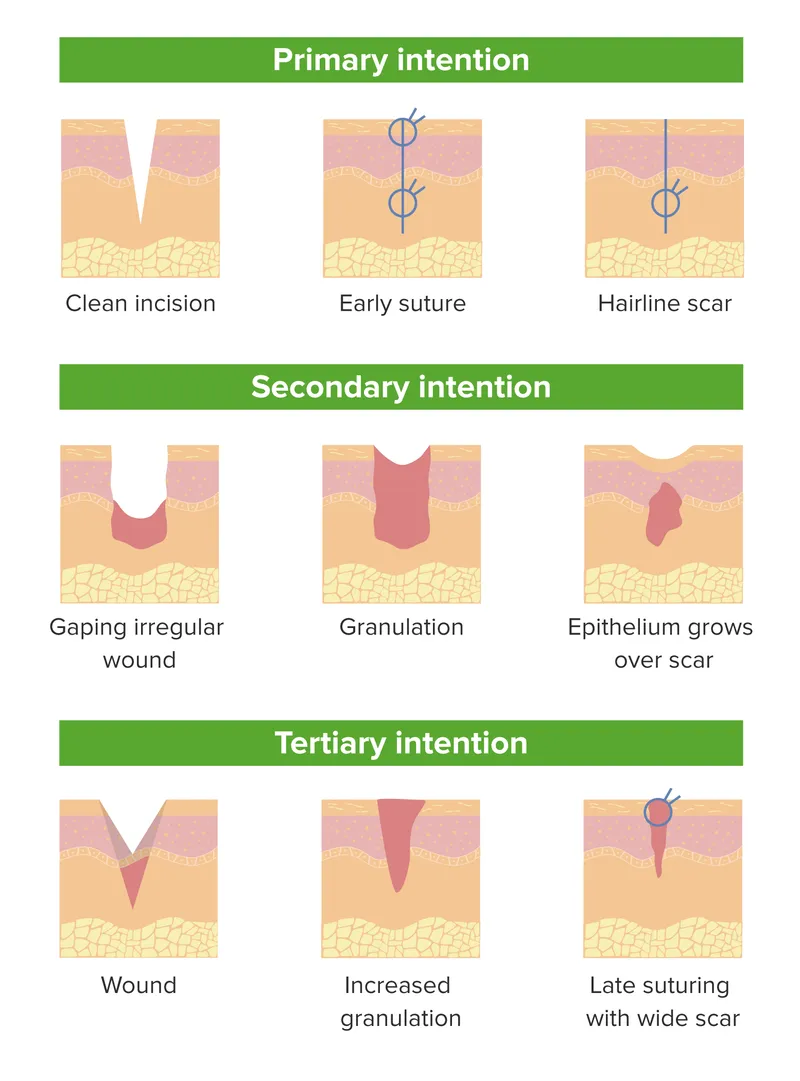
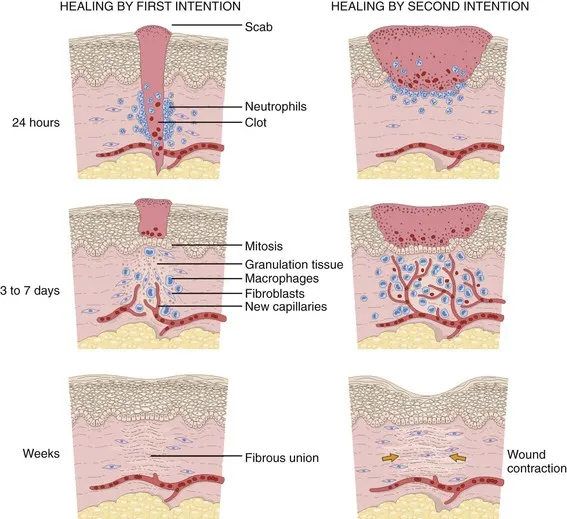
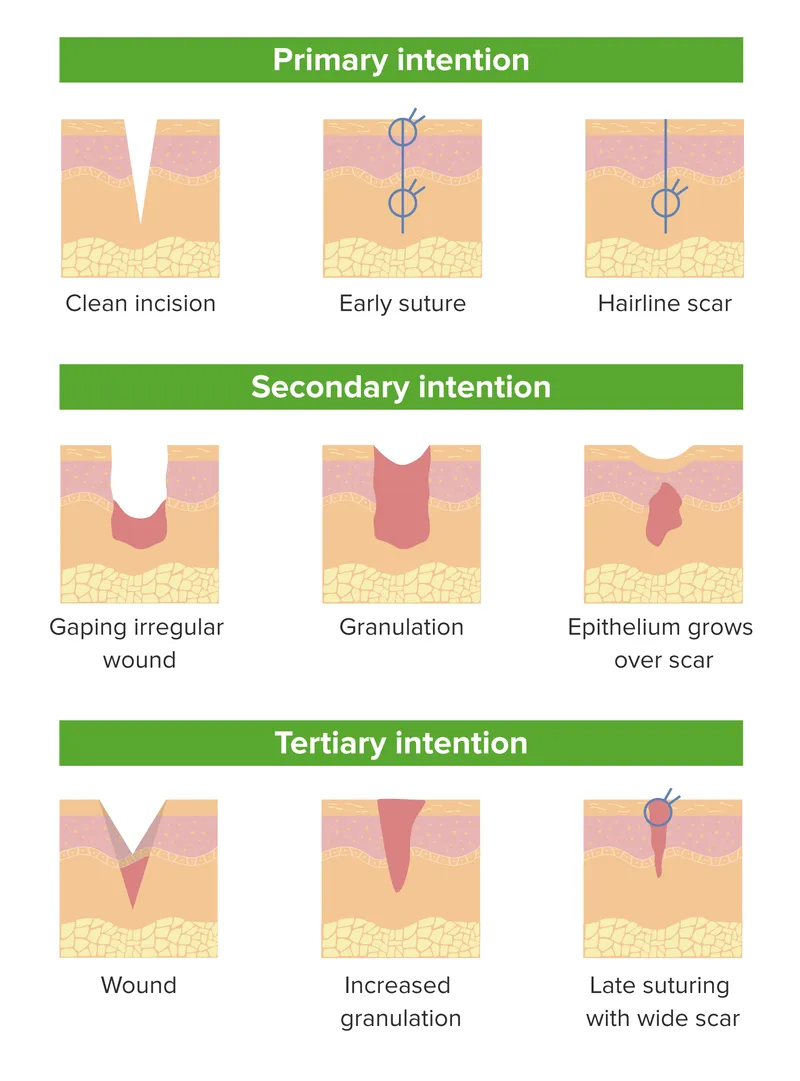
- This approach is appropriate for a **contaminated, high-risk avulsion wound** to prevent infection and promote healing by secondary intention.
- The patient needs an updated **tetanus vaccine** because his last one was six years ago, and he has a contaminated wound.
*Apposition of wound edges under tension + rifampin*
- **Closing a contaminated wound under tension** is contraindicated as it increases the risk of infection and necrosis.
- **Rifampin is generally not the first-line prophylactic antibiotic** for this type of wound injury and is not needed if the wound has been thoroughly cleaned.
*Surgical treatment with skin flap + ciprofloxacin*
- This is an **overly aggressive initial approach** for an acute, contaminated wound, as the priority is preventing infection before definitive closure or reconstruction.
- **Ciprofloxacin** is not typically the first-choice prophylactic antibiotic for contaminated soft tissue wounds.
*Surgical treatment with skin graft + tetanus vaccine*
- A **skin graft** is a definitive reconstructive procedure and is not indicated as the immediate next step for a fresh, contaminated avulsion wound.
- The wound first needs to be thoroughly cleaned and monitored for infection before considering graft options.
*Tension-free apposition of wound edges + sterile dressing*
- While **tension-free closure** is ideal, this wound is **heavily contaminated with soil and dirt** and has some avulsion, making primary closure risky due to a high infection rate.
- **Allowing the wound to heal by secondary intention** with a moist dressing is safer in this situation.
Types of wound closure US Medical PG Question 2: A 23-year-old woman is brought to the emergency department 30 minutes after stepping on a piece of broken glass. Physical examination shows a 3-cm, ragged laceration on the plantar aspect of the left foot. The physician uses hydrogen peroxide to clean the wound. Which of the following is the most likely mechanism of action of this disinfectant?
- A. Formation of free radicals (Correct Answer)
- B. Intercalation of DNA
- C. Crosslinking of proteins
- D. Halogenation of nucleic acids
- E. Congealing of cytoplasm
Types of wound closure Explanation: ***Formation of free radicals***
- **Hydrogen peroxide** acts as an **oxidizing agent**, generating highly reactive **oxygen-free radicals** (e.g., superoxide, hydroxyl radicals) that damage microbial cellular components.
- This **oxidative damage** disrupts proteins, lipids, and nucleic acids, leading to bacterial and viral cell death.
*Intercalation of DNA*
- This mechanism is characteristic of certain **chemotherapeutic agents** (e.g., doxorubicin, ethidium bromide) and some **antimicrobials**, which insert themselves between DNA base pairs, disrupting replication and transcription.
- Hydrogen peroxide does not typically target DNA in this manner for its disinfectant action.
*Crosslinking of proteins*
- This mechanism is characteristic of **aldehydes** like **formaldehyde** and **glutaraldehyde**, which form covalent bonds between amino groups of proteins, denaturing them and disrupting cellular function.
- While hydrogen peroxide can modify proteins, its primary disinfectant action is not through widespread protein crosslinking.
*Halogenation of nucleic acids*
- This mechanism is primarily associated with **halogens** such as **chlorine** and **iodine**, which react with nucleic acids to form halogenated compounds, thereby inactivating them.
- Hydrogen peroxide, while an oxidizer, does not lead to halogenation as its primary mode of action.
*Congealing of cytoplasm*
- This mechanism, which refers to the coagulation or solidification of cellular contents, is typical of **alcohols** (e.g., ethanol, isopropanol) and some **heavy metal salts** that denature proteins and lipids, leading to cell lysis.
- Hydrogen peroxide's action is more specific to oxidative damage rather than general cytoplasmic congealing.
Types of wound closure US Medical PG Question 3: During examination of a stab wound, a forensic pathologist notes that one end is sharp and pointed while the other is square or blunt. The wound track shows a consistent width. Which of the following weapon characteristics is most likely?
- A. Ice pick
- B. Double-edged knife
- C. Scissors
- D. Single-edged knife (Correct Answer)
Types of wound closure Explanation: ***Single-edged knife***
- A **single-edged knife** has one sharp cutting edge and one blunt or squared-off spine, which accounts for one end of the stab wound being pointed and the other being square or blunt.
- The **consistent width of the wound track** suggests that the blade was relatively flat and inserted perpendicular to the skin, with the width matching the blade's thickness.
*Ice pick*
- An **ice pick** typically produces a small, round, or oval wound that is often deeper than it is wide, and both ends would appear similar rather than one sharp and one blunt.
- The wound edges would typically be uniform, not exhibiting a distinct sharp and blunt end indicative of a blade.
*Double-edged knife*
- A **double-edged knife** has two sharp cutting edges; therefore, both ends of the stab wound would appear sharp and pointed, contrary to the description of one blunt end.
- The resulting wound might be more uniformly incised on both sides.
*Scissors*
- **Scissors**, when used to stab, typically create two parallel incised wounds or a jagged, irregular hole, depending on whether they were open or closed during impact.
- It would be unlikely to produce a single stab wound with one sharp and one blunt end unless only one blade penetrated, which would still result in a different morphology than described.
Types of wound closure US Medical PG Question 4: A 27-year-old man presents to the emergency department after a dog bite. The patient was intoxicated and pulled the dog’s tail while it was eating. The dog belongs to his friend and is back at his friend’s house currently. Physical exam is notable for a dog bite on the patient’s right arm. The wound is irrigated and explored with no retained bodies found. A tetanus vaccination is administered. Which of the following is appropriate management of this patient?
- A. Administer the rabies vaccine and rabies immunoglobulin
- B. Administer amoxicillin-clavulanic acid (Correct Answer)
- C. Discharge the patient with outpatient follow up
- D. Close the wound with sutures and discharge the patient
- E. Administer trimethoprim-sulfamethoxazole
Types of wound closure Explanation: ***Administer amoxicillin-clavulanic acid***
- Dog bite wounds are at high risk for bacterial infection, particularly from oral flora like *Pasteurella multocida* and *Capnocytophaga canimorsus*. **Amoxicillin-clavulanic acid** provides broad-spectrum coverage against these common pathogens.
- Due to the nature of the wound (puncture, crush), the risk of infection is significant, warranting **prophylactic antibiotics** even after wound irrigation and exploration.
*Administer the rabies vaccine and rabies immunoglobulin*
- **Rabies post-exposure prophylaxis (PEP)** is indicated if the animal is high-risk, unprovoked, or cannot be observed. In this case, the dog is known and provoked, and its vaccination status can be ascertained.
- The dog is owned by a friend and is presumably available for **observation** or vaccination status confirmation, which would typically negate the immediate need for rabies PEP.
*Discharge the patient with outpatient follow up*
- Discharging the patient without further intervention, specifically **antibiotic prophylaxis**, would be inappropriate given the high risk of infection associated with dog bites.
- While follow-up is important, the immediate concern is **infection prevention**, which requires an initial intervention in the emergency department.
*Close the wound with sutures and discharge the patient*
- Dog bite wounds, especially **puncture or crush wounds**, are generally **not primarily closed by suturing** due to the high risk of trapping bacteria and increasing infection rates.
- Instead, these wounds are typically left **open to heal by secondary intention** after thorough cleaning and antibiotic prophylaxis.
*Administer trimethoprim-sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole** is not the antibiotic of choice for dog bite wounds. It lacks sufficient coverage against the common anaerobic and gram-negative organisms, such as *Pasteurella*, found in dog oral flora.
- **Amoxicillin-clavulanic acid** is preferred due to its superior coverage for typical dog bite pathogens.
Types of wound closure US Medical PG Question 5: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Types of wound closure Explanation: ***Keloid scar formation***
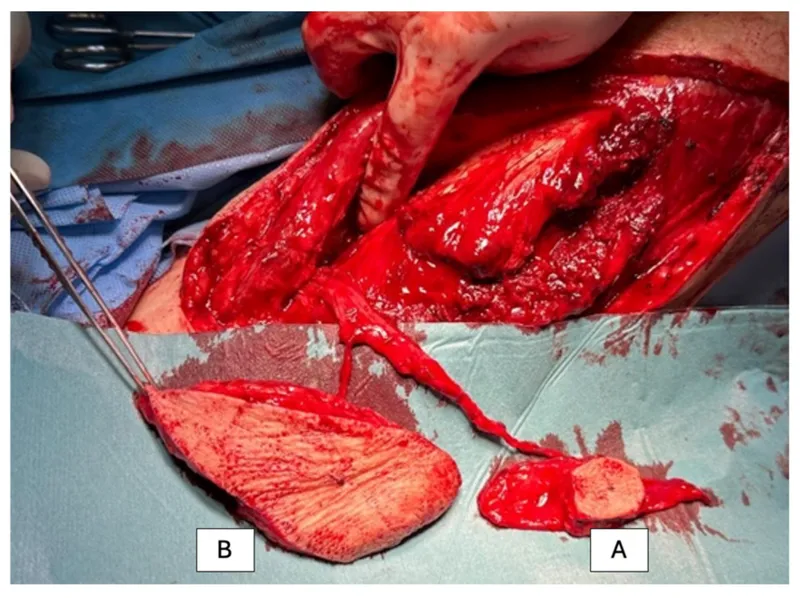
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Types of wound closure US Medical PG Question 6: A 15-year-old boy presents to the emergency department after a rusty nail pierced through his right foot. He was able to pull out the nail, but is unable to walk on his foot. He believes he had all his shots as a child, but his mother is unsure and cannot recall the specific vaccination dates or details. His last documented tetanus vaccination was at age 12. The vital signs are within normal limits. Physical examination reveals a 0.5-inch puncture wound on the right heel. The site is tender, erythematous, with flecks of reddish-brown particles in the base. No blood or discharge is seen. Which of the following is the most appropriate next step in management?
- A. Administer DT
- B. Administer Td only
- C. Clean and dress the wound only
- D. Administer Td and TIG (Correct Answer)
- E. Administer Tdap, Td, and TIG (tetanus immune globulin)
Types of wound closure Explanation: ***Administer Td and TIG***
- This patient has a **dirty wound** (rusty nail, reddish-brown particles indicating contamination) with **uncertain immunization history** (mother cannot recall vaccination details or confirm completion of primary series).
- Although the last documented tetanus vaccination was at age 12 (3 years ago), the **uncertainty about whether the primary vaccination series was completed** necessitates treating this as an incomplete immunization history.
- For dirty wounds with uncertain/incomplete immunization history, both **Td (active immunity)** and **Tetanus Immune Globulin/TIG (immediate passive immunity)** are required per CDC guidelines.
- TIG provides immediate protection against circulating tetanus toxin while Td stimulates the patient's own immune response.
*Administer DT*
- **DT** (diphtheria and tetanus toxoids) is formulated for children **younger than 7 years old**.
- This patient is 15 years old, so **Td** (adult formulation with reduced diphtheria component) is the appropriate vaccine.
*Administer Td only*
- While a **Td booster** addresses active immunity, it takes **2-4 weeks** to produce protective antibody levels.
- For a **high-risk dirty wound with uncertain immunization history**, this delayed protection is insufficient.
- **TIG is essential** to provide immediate passive immunity and neutralize any tetanus toxin that may be produced before the Td vaccine becomes effective.
*Clean and dress the wound only*
- **Wound care** (cleaning, irrigation, debridement of devitalized tissue) is essential but **insufficient** as sole management.
- Given the high-risk wound and uncertain immunization history, **tetanus prophylaxis is mandatory** to prevent potentially fatal tetanus infection.
*Administer Tdap, Td, and TIG (tetanus immune globulin)*
- Administering both **Tdap and Td simultaneously is redundant** and not recommended.
- **Tdap** (which includes pertussis) can be used instead of Td for wound prophylaxis if the patient has never received Tdap, but giving both Tdap AND Td is unnecessary.
- While TIG is appropriate for this scenario, the dual vaccine administration (Tdap + Td) is **not standard practice**.
Types of wound closure US Medical PG Question 7: A 14-year-old girl is brought to the physician after she accidentally cut her right forearm earlier that morning while working with her mother's embroidery scissors. She has no history of serious illness. The mother says she went to elementary and middle school abroad and is not sure if she received all of her childhood vaccinations. She appears healthy. Her temperature is 37°C (98.6 °F), pulse 90/min, and blood pressure is 102/68 mm Hg. Examination shows a clean 2-cm laceration on her right forearm with surrounding edema. There is no erythema or discharge. The wound is irrigated with water and washed with soap. Which of the following is the most appropriate next step in management?
- A. Administer Tdap only (Correct Answer)
- B. Administer DTaP only
- C. No further steps are necessary
- D. Administer TIG only
- E. Intravenous metronidazole
Types of wound closure Explanation: ***Administer Tdap only***
- A 14-year-old with an unknown or incomplete vaccination history requires a **Tdap (tetanus, diphtheria, acellular pertussis) booster** for **tetanus prophylaxis** after a wound.
- The wound is clean, and there are no signs of active infection or high-risk features that would necessitate tetanus immune globulin (TIG).
*Administer DTaP only*
- **DTaP (diphtheria, tetanus, acellular pertussis)** is typically administered to children younger than 7 years of age.
- This patient is 14 years old, making Tdap the more appropriate vaccine formulation for her age group.
*No further steps are necessary*
- Given the patient's **unknown vaccination history** and a laceration, tetanus prophylaxis is crucial to prevent **tetanus**, a potentially life-threatening condition.
- Simply cleaning the wound is insufficient protection without adequate vaccination status.
*Administer TIG only*
- **Tetanus immune globulin (TIG)** is typically reserved for patients with **dirty or severe wounds** and an unknown or incomplete vaccination history, or for those who are immunocompromised.
- This patient has a **clean laceration** with no indication of high-risk features that would warrant TIG.
*Intravenous metronidazole*
- **Metronidazole** is an antibiotic used to treat **anaerobic bacterial infections** and certain parasitic infections.
- The patient has no signs of infection (no erythema, discharge, or fever) that would necessitate antibiotic treatment at this time.
Types of wound closure US Medical PG Question 8: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Types of wound closure Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
Types of wound closure US Medical PG Question 9: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Types of wound closure Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Types of wound closure US Medical PG Question 10: A 15-year-old boy is brought to the emergency department by ambulance after his mother found him having muscle spasms and stiffness in his room. His mother stated he scraped his foot on a rusty razor on the bathroom floor 2 days prior. On presentation, his temperature is 102.0°F (38.9°C), blood pressure is 108/73 mmHg, pulse is 122/min, and respirations are 18/min. On physical exam, he is found to have severe muscle spasms and rigid abdominal muscles. In addition, he has a dirty appearing wound on his right foot. The patient's mother does not recall any further vaccinations since age 12. Finally, he is found to have difficulty opening his mouth so he is intubated. Which of the following treatment(s) should be provided to this patient?
- A. Wound debridement and antitoxin
- B. Antitoxin
- C. Wound debridement
- D. Wound debridement and booster vaccine
- E. Wound debridement, antitoxin, and booster vaccine (Correct Answer)
Types of wound closure Explanation: ***Wound debridement, antitoxin, and booster vaccine***
- The patient presents with classic symptoms of **tetanus** (muscle spasms, stiffness, trismus, fever) following a contaminated wound, and an uncertain vaccination history.
- **Wound debridement** removes the source of toxin production, **antitoxin** (tetanus immune globulin) neutralizes circulating toxin, and a **booster vaccine** provides active immunity against future infections.
*Wound debridement and antitoxin*
- While **wound debridement** and **antitoxin** are critical for acute management, omitting the booster vaccine leaves the patient vulnerable to future tetanus infections.
- A booster dose is essential to stimulate the patient's own immune system and provide **long-term immunity**, especially with a history of unknown vaccination status.
*Antitoxin*
- Administering only **antitoxin** would neutralize circulating toxins but would not address the ongoing production of toxins from the contaminated wound.
- It also wouldn't provide **active immunization** to protect against future exposures.
*Wound debridement*
- **Wound debridement** alone removes the bacterial source but does not neutralize the already circulating **tetanus toxin**, which is responsible for the severe neurological symptoms.
- It also fails to provide immediate passive immunity with antitoxin or active immunization with a booster.
*Wound debridement and booster vaccine*
- This option correctly addresses removing the source and providing active immunity but critically misses the immediate need for **antitoxin** to neutralize existing toxins and alleviate the life-threatening symptoms.
- The **tetanus toxin** acts rapidly, and prompt neutralization is crucial to prevent further neurological damage and improve prognosis.
More Types of wound closure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.