Scarring process and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Scarring process and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Scarring process and management US Medical PG Question 1: A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?
- A. Fibroblasts
- B. Myofibroblasts (Correct Answer)
- C. Neutrophils
- D. Macrophages
- E. Endothelial cells
Scarring process and management Explanation: ***Myofibroblasts***
- The patient presents with a **contracture** (restricted range of motion and hyperextension of the hand due to a thick scar) after a burn, which is characteristic of the action of **myofibroblasts**.
- Myofibroblasts are specialized cells that possess features of both fibroblasts (synthesizing **collagen** and extracellular matrix) and smooth muscle cells (containing **actin microfilaments**), allowing them to exert contractile force which leads to scar contraction.
*Fibroblasts*
- While fibroblasts are crucial for **wound healing** by producing collagen and other extracellular matrix components, they primarily lay down the foundation for scar tissue.
- They lack the strong contractile capabilities that lead to significant **tissue retraction** and contracture.
*Neutrophils*
- Neutrophils are **acute inflammatory cells** that primarily function in the early stages of wound healing to phagocytose debris and pathogens.
- They do not play a direct role in the formation of **scar tissue** or **contractures**.
*Macrophages*
- Macrophages are important **immune cells** involved in clearing debris, presenting antigens, and releasing growth factors during the later stages of wound healing.
- They also influence fibroblast activity, but they do not directly cause **tissue contraction** or scar formation.
*Endothelial cells*
- Endothelial cells line **blood vessels** and are essential for **angiogenesis** (formation of new blood vessels) during wound healing.
- They are not involved in the **contractile process** that leads to scar contracture.
Scarring process and management US Medical PG Question 2: During examination of a stab wound, a forensic pathologist notes that one end is sharp and pointed while the other is square or blunt. The wound track shows a consistent width. Which of the following weapon characteristics is most likely?
- A. Ice pick
- B. Double-edged knife
- C. Scissors
- D. Single-edged knife (Correct Answer)
Scarring process and management Explanation: ***Single-edged knife***
- A **single-edged knife** has one sharp cutting edge and one blunt or squared-off spine, which accounts for one end of the stab wound being pointed and the other being square or blunt.
- The **consistent width of the wound track** suggests that the blade was relatively flat and inserted perpendicular to the skin, with the width matching the blade's thickness.
*Ice pick*
- An **ice pick** typically produces a small, round, or oval wound that is often deeper than it is wide, and both ends would appear similar rather than one sharp and one blunt.
- The wound edges would typically be uniform, not exhibiting a distinct sharp and blunt end indicative of a blade.
*Double-edged knife*
- A **double-edged knife** has two sharp cutting edges; therefore, both ends of the stab wound would appear sharp and pointed, contrary to the description of one blunt end.
- The resulting wound might be more uniformly incised on both sides.
*Scissors*
- **Scissors**, when used to stab, typically create two parallel incised wounds or a jagged, irregular hole, depending on whether they were open or closed during impact.
- It would be unlikely to produce a single stab wound with one sharp and one blunt end unless only one blade penetrated, which would still result in a different morphology than described.
Scarring process and management US Medical PG Question 3: A 35-year-old woman with no significant past medical, past surgical, family or social history presents to clinic with a recently identified area of flat, intact, pigmented skin. The patient believes that this is a large freckle, and she states that it becomes darker during the summer when she is outdoors. On physical examination, you measure the lesion to be 6 mm in diameter. Which of the following is the best descriptor of this patient’s skin finding?
- A. Wheal
- B. Papule
- C. Ulcer
- D. Plaque
- E. Macule (Correct Answer)
Scarring process and management Explanation: ***Macule***
- A **macule** is a **flat, discolored lesion** that is less than 1 cm in diameter, which fits the description of a **flat, pigmented skin area** that is 6 mm in diameter.
- The darkening of the lesion with sun exposure is characteristic of a **freckle**, which is a type of macule caused by increased melanin production without an increase in melanocyte numbers.
*Wheal*
- A **wheal** is a **transient, elevated lesion** caused by dermal edema, typically seen in allergic reactions like hives.
- This patient's lesion is described as a **flat, pigmented area**, not an elevated, transient swelling.
*Papule*
- A **papule** is a **solid, elevated lesion** that is less than 1 cm in diameter.
- The patient's skin finding is explicitly described as **flat** and intact, not elevated.
*Ulcer*
- An **ulcer** is a **loss of epidermis and dermis**, resulting in an open sore; it is not a flat, intact pigmented lesion.
- The description of the lesion as **intact** rules out an ulcer, which involves a break in the skin surface.
*Plaque*
- A **plaque** is a **flat-topped, elevated lesion** that is larger than 1 cm in diameter.
- While flat-topped, a plaque is **elevated**, and the patient's lesion is described as **flat**, not elevated.
Scarring process and management US Medical PG Question 4: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
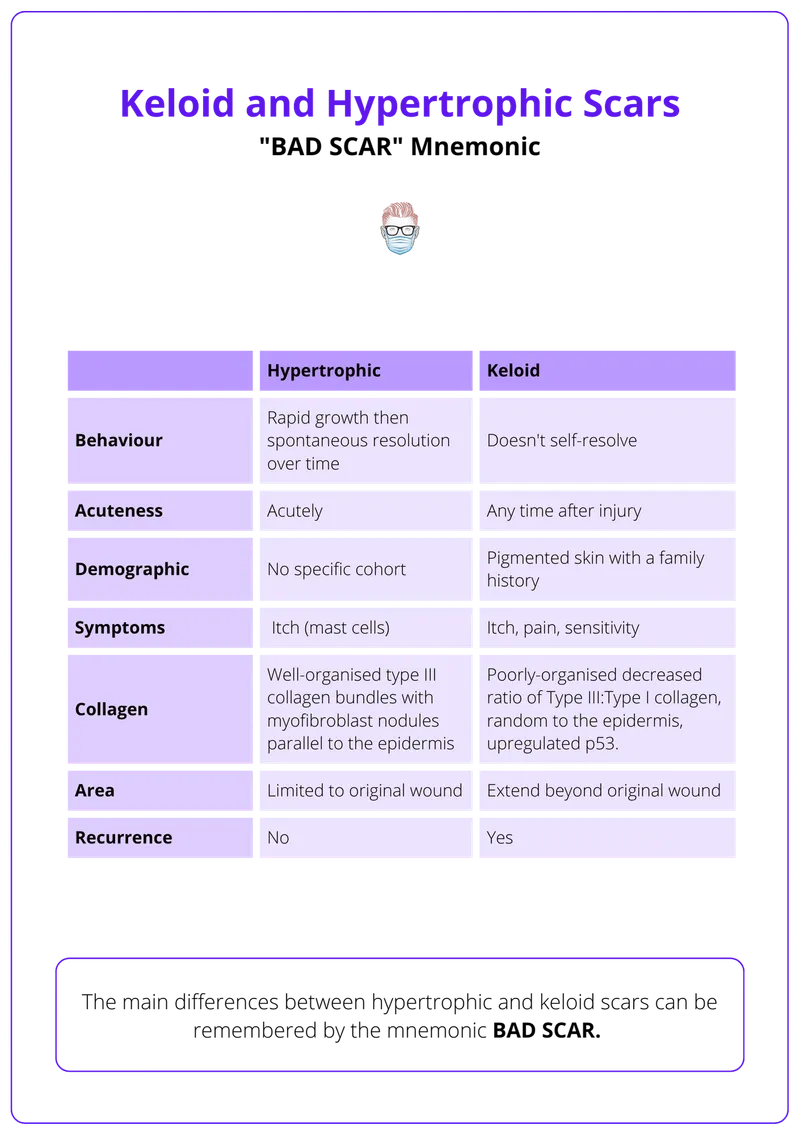
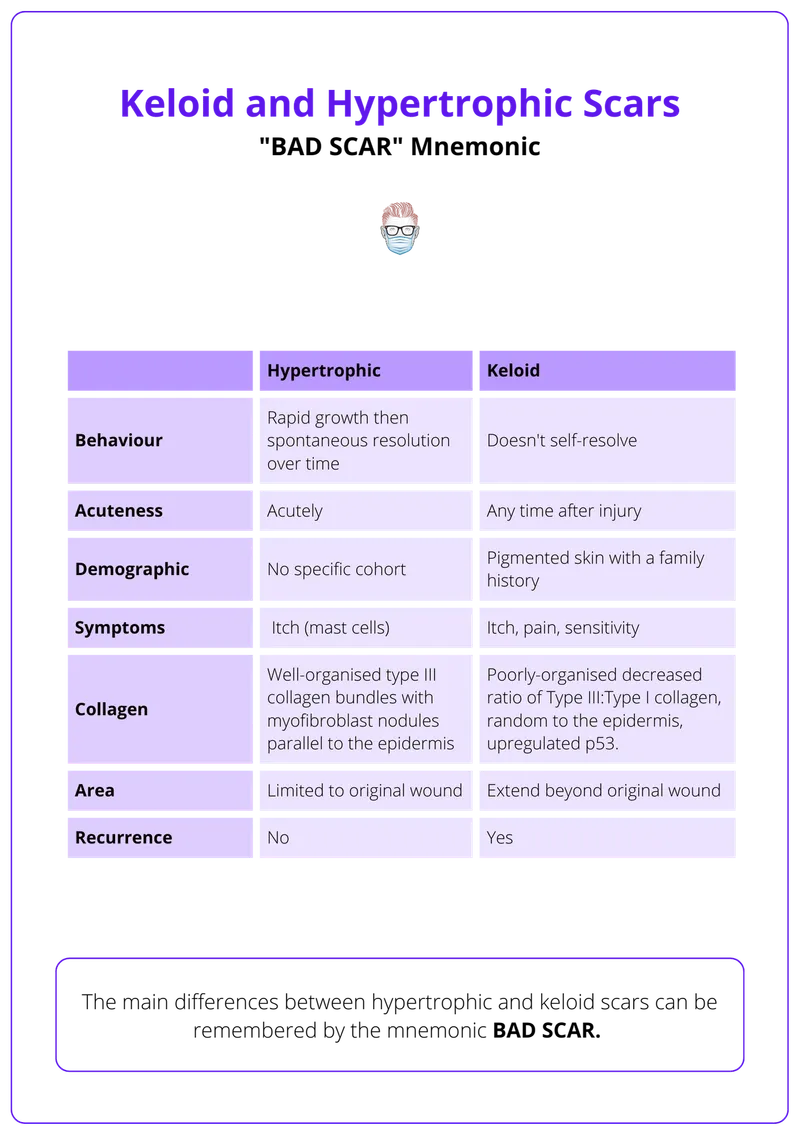
Scarring process and management Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Scarring process and management US Medical PG Question 5: A 60-year-old male presents with fatigue, dyspnea on exertion, and lower extremity edema. Physical examination reveals an elevated jugular venous pressure and an S3 heart sound. Which of the following medications is most likely to improve this patient's symptoms?
- A. Metoprolol
- B. Furosemide (Correct Answer)
- C. Losartan
- D. Lisinopril
- E. Spironolactone
Scarring process and management Explanation: ***Correct: Furosemide***
- The patient presents with classic signs of **heart failure with fluid overload**: dyspnea on exertion, lower extremity edema, elevated jugular venous pressure, and an S3 heart sound (indicating volume overload).
- **Furosemide**, a **loop diuretic**, is the most effective medication for **rapid symptomatic relief** in heart failure with congestion. It works by blocking sodium and water reabsorption in the loop of Henle, promoting diuresis and reducing **pulmonary congestion** and **peripheral edema**.
- While other medications like ACE inhibitors, beta-blockers, and aldosterone antagonists are crucial for **long-term mortality reduction** and disease modification, loop diuretics provide the **fastest and most direct symptomatic improvement** for fluid overload.
*Incorrect: Metoprolol*
- **Metoprolol** is a **beta-blocker** that is essential for chronic HFrEF management, providing **mortality reduction** and **reverse cardiac remodeling**.
- However, beta-blockers take **weeks to months** to show symptomatic benefit and can initially **worsen symptoms** due to negative inotropic effects, especially in acute decompensation.
- While important for long-term management, metoprolol does not provide immediate symptomatic relief from fluid overload.
*Incorrect: Losartan*
- **Losartan** is an **angiotensin receptor blocker (ARB)** used as an alternative to ACE inhibitors in HFrEF, particularly in patients who develop cough with ACE inhibitors.
- ARBs reduce **afterload** and prevent **cardiac remodeling**, contributing to improved long-term outcomes and mortality reduction.
- However, they do not directly address fluid overload and do not provide rapid symptomatic relief compared to diuretics.
*Incorrect: Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that improves mortality in HFrEF by preventing myocardial fibrosis, reducing cardiac remodeling, and preventing potassium loss.
- While beneficial for long-term management, spironolactone has **weak diuretic effects** and takes weeks to provide symptomatic benefit.
- It is not the first-line choice for **acute symptomatic relief** of volume overload, though it is an important component of chronic HFrEF therapy.
*Incorrect: Lisinopril*
- **Lisinopril** is an **ACE inhibitor** and a cornerstone of HFrEF therapy, reducing **mortality**, **hospitalizations**, and preventing **cardiac remodeling** by reducing afterload and preload.
- While ACE inhibitors improve symptoms over time, they do not provide the **rapid diuretic effect** needed for immediate relief of dyspnea and edema.
- Lisinopril is essential for long-term management but is not the most effective option for acute symptomatic improvement of fluid overload.
Scarring process and management US Medical PG Question 6: A 30-year-old woman dies shortly after admission to the emergency department. The family requests an autopsy to determine cause of death. During the autopsy, multiple linear, parallel marks are noted across her wrists. Which of the following patterns suggests these are hesitation marks rather than defensive wounds?
- A. Irregular, scattered marks
- B. Diagonal, deep lacerations
- C. Deep, single cuts
- D. Superficial, parallel cuts (Correct Answer)
Scarring process and management Explanation: ***Superficial, parallel cuts***
- **Hesitation marks** are typically numerous, **superficial**, and **parallel**, reflecting a tentative or indecisive attempt and often made in the same direction.
- They tend to be concentrated in an area of the body chosen for self-harm, such as the wrists, and are usually consistent with a non-fatal intent.
*Irregular, scattered marks*
- This pattern is more indicative of **defensive wounds**, which are often scattered and irregular due to attempts to ward off an attack.
- Defensive wounds are typically found on the palms, forearms, and other areas used for protection.
*Diagonal, deep lacerations*
- **Deep lacerations**, especially if diagonal and singular, are less characteristic of hesitation marks and more suggestive of a determined attempt to inflict fatal injury or could be defensive.
- **Hesitation marks** are typically not aimed at quickly causing fatal harm.
*Deep, single cuts*
- A single, **deep cut** is often associated with a resolute intent to cause significant injury or death, rather than the hesitant, superficial nature of hesitation marks.
- This pattern would warrant further investigation into the intent and circumstances surrounding the injury.
Scarring process and management US Medical PG Question 7: A 45-year-old man comes to his primary care provider for a routine visit. The patient mentions that while he was cooking 5 days ago, he accidentally cut himself with a meat cleaver and lost the skin at the tip of his finger. After applying pressure and ice, the bleeding stopped and he did not seek treatment. The patient is otherwise healthy and does not take any daily medications. The patient’s temperature is 98.2°F (36.8°C), blood pressure is 114/72 mmHg, pulse is 60/min, and respirations are 12/min. On exam, the patient demonstrates a 0.5 x 0.3 cm wound on the tip of his left third finger. No bone is involved, and the wound is red, soft, and painless. There are no signs of infection. Which of the following can be expected on histopathological examination of the wounded area?
- A. Platelet aggregates
- B. Epithelial cell migration from the wound borders
- C. Neutrophil migration into the wound
- D. Deposition of type III collagen (Correct Answer)
- E. Deposition of type I collagen
Scarring process and management Explanation: ***Deposition of type III collagen***
- Five days post-injury, the **proliferative phase of wound healing** is active, characterized by the formation of an initial **granulation tissue** matrix primarily composed of **Type III collagen**.
- This type of collagen forms thinner, more flexible fibers that provide a temporary scaffold for tissue regeneration before being gradually replaced by stronger Type I collagen.
*Platelet aggregates*
- **Platelet aggregation** occurs immediately after injury as part of **hemostasis**, forming a plug to stop bleeding.
- By five days, this initial phase would have concluded, and the primary focus would be on tissue repair and regeneration.
*Epithelial cell migration from the wound borders*
- **Epithelial cell migration** for re-epithelialization typically occurs within the first 24-48 hours after injury, forming a new epidermal layer over the wound.
- While it continues, the dominant histological feature at day 5 in an open wound of this size would be **granulation tissue formation** in the dermis.
*Neutrophil migration into the wound*
- **Neutrophil migration** is a hallmark of the **inflammatory phase**, peaking within 24-48 hours post-injury to clear debris and microbes.
- By day 5, the inflammatory phase would be subsiding, and macrophages would be more prevalent, signaling the transition to the proliferative phase.
*Deposition of type I collagen*
- **Type I collagen** is the predominant collagen found in mature scar tissue and is deposited during the later **remodeling phase** of wound healing.
- While some Type I collagen may be present, **Type III collagen** is characteristic of the early granulation tissue prominent at day 5.
Scarring process and management US Medical PG Question 8: A 42-year-old man sustains a deep laceration requiring surgical debridement. The wound care team debates between primary closure versus healing by secondary intention. The wound is 6 cm long, 2 cm wide, located on the lower leg with mild contamination from soil exposure, and the patient is a heavy smoker with peripheral vascular disease. Evaluate which approach best synthesizes the risk-benefit analysis for optimal outcome?
- A. Skin grafting after granulation tissue formation
- B. Immediate primary closure with prophylactic antibiotics
- C. Delayed primary closure after 3-5 days of wound observation (Correct Answer)
- D. Healing by secondary intention with negative pressure therapy
- E. Primary closure with tension-relieving retention sutures
Scarring process and management Explanation: ***Delayed primary closure after 3-5 days of wound observation***
- This approach, also known as **tertiary intention**, is ideal for **contaminated wounds** as it allows time for the inflammatory phase to reduce bacterial load before final closure.
- It balances the risk of infection from **soil exposure** and **peripheral vascular disease** with the benefit of better functional and cosmetic outcomes compared to secondary intention.
*Skin grafting after granulation tissue formation*
- This technique is typically reserved for **extensive skin loss** or large defects where edges cannot be approximated, which is not indicated for a 6 cm linear laceration.
- It involves a more complex surgical procedure and carries a high risk of failure in patients with **peripheral vascular disease** and **smoking-related** poor microcirculation.
*Immediate primary closure with prophylactic antibiotics*
- Primary closure of a **contaminated wound** significantly increases the risk of **wound dehiscence** and abscess formation, especially in a low-perfusion area like the lower leg.
- The patient’s history of **smoking** and **vascular disease** further impairs oxygen delivery and immune response, making immediate closure premature.
*Healing by secondary intention with negative pressure therapy*
- While this reduces infection risk, it leads to a prolonged healing period and significant **scar contracture**, which can impair movement on the lower leg.
- It is less efficient than delayed primary closure for a cleanable laceration and is usually reserved for **chronically infected** or non-approximable wounds.
*Primary closure with tension-relieving retention sutures*
- Placing sutures under tension in a patient with **peripheral vascular disease** further compromises **capillary perfusion**, leading to skin flap necrosis.
- Retention sutures do not address the primary concern of **bacterial contamination** from the soil, which remains trapped within the closed wound space.
Scarring process and management US Medical PG Question 9: A 35-year-old woman with known deficiency in Ehlers-Danlos syndrome presents with recurrent wound dehiscence following multiple abdominal surgeries. Genetic testing confirms a mutation affecting type III collagen synthesis. She now requires another laparotomy for adhesive bowel obstruction. The surgical team must decide on closure technique. Synthesizing knowledge of collagen biochemistry and surgical principles, which approach best addresses her specific wound healing defect?
- A. Vacuum-assisted closure followed by skin grafting
- B. Standard layer closure with permanent sutures only
- C. Delayed primary closure after 5-7 days
- D. Retention sutures with permanent mesh reinforcement (Correct Answer)
- E. Biological mesh with early suture removal
Scarring process and management Explanation: ***Retention sutures with permanent mesh reinforcement***
- In patients with **Vascular Ehlers-Danlos syndrome (Type IV)**, deficiency in **Type III collagen** results in inherently weak connective tissue that never reaches normal tensile strength.
- **Retention sutures** distribute tension across a larger surface area, and **permanent mesh** provides life-long mechanical reinforcement to compensate for the permanent **collagen synthesis defect**.
*Vacuum-assisted closure followed by skin grafting*
- While useful for infected wounds, this approach does not provide the **structural integrity** required to prevent future dehiscence or incisional hernias.
- **Skin grafts** do not address the primary issue of **fascial weakness** and tensile failure in deep tissue layers.
*Standard layer closure with permanent sutures only*
- Standard techniques are insufficient because the patient's tissues are too **fragile** to hold individual sutures under the stress of abdominal pressure.
- Permanent sutures may "cheese-wire" through the weak **collagen-deficient fascia**, leading to immediate or early **wound dehiscence**.
*Delayed primary closure after 5-7 days*
- This technique is primarily used to reduce **surgical site infection** risk in contaminated wounds but does not alter the biochemical quality of collagen.
- It fails to address the fundamental problem of **poor wound healing** and mechanical fragility seen in **Ehlers-Danlos syndrome**.
*Biological mesh with early suture removal*
- **Biological meshes** are designed to be resorbed and replaced by host collagen, which in this patient would still be defective **Type III collagen**.
- **Early suture removal** is contraindicated as these patients require prolonged or permanent mechanical support due to delayed and **incomplete wound maturation**.
Scarring process and management US Medical PG Question 10: A 58-year-old man with chronic kidney disease (creatinine 4.2 mg/dL) and uremia undergoes arteriovenous fistula creation for dialysis access. Four weeks postoperatively, the wound continues to show poor healing with minimal tensile strength. Laboratory studies show elevated blood urea nitrogen. Considering the multiple factors affecting wound healing in uremia, evaluate which intervention would most comprehensively address the wound healing deficit?
- A. Systemic corticosteroid therapy to reduce inflammation
- B. High-dose vitamin C and zinc supplementation
- C. Initiation of hemodialysis to reduce uremia (Correct Answer)
- D. Hyperbaric oxygen therapy sessions
- E. Local application of platelet-derived growth factor
Scarring process and management Explanation: ***Initiation of hemodialysis to reduce uremia***
- **Uremia** inhibits wound healing by impairing **fibroblast proliferation**, **collagen synthesis**, and **neoangiogenesis**, thus reducing the **tensile strength** of the wound.
- Initiating **hemodialysis** directly reduces the concentration of **uremic toxins**, which is the most comprehensive way to reverse the cellular and metabolic dysfunction hindering the healing process.
*Systemic corticosteroid therapy to reduce inflammation*
- **Corticosteroids** actually impair wound healing further by inhibiting **inflammatory cells**, **angiogenesis**, and **fibroblast activity**.
- Using them in a uremic patient would increase the risk of **wound dehiscence** and **infection**, rather than improving healing outcomes.
*High-dose vitamin C and zinc supplementation*
- While **vitamin C** and **zinc** are essential for **collagen cross-linking**, supplementation alone cannot overcome the broad systemic inhibitory effects of **uremic toxins**.
- These nutrients are only beneficial if a documented **deficiency** exists and do not address the primary pathophysiology of **uremic wound failure**.
*Hyperbaric oxygen therapy sessions*
- **Hyperbaric oxygen** therapy is primarily indicated for **hypoxic wounds** or **chronic non-healing ulcers** in diabetic patients with vascular compromise.
- It does not address the metabolic inhibition caused by **uremia** and would be an inappropriate and expensive primary intervention in this clinical scenario.
*Local application of platelet-derived growth factor*
- **Growth factors** are specialized interventions that target specific signaling pathways but do not correct the **environment of uremia** that suppresses overall cell function.
- Without addressing the patient's **azotemia**, the local cellular response to exogenous **PDGF** remains blunted and ineffective.
More Scarring process and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.