Primary vs. secondary intention US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Primary vs. secondary intention. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Primary vs. secondary intention US Medical PG Question 1: A 55-year-old African American female presents to her breast surgeon for a six-month follow-up visit after undergoing a modified radical mastectomy for invasive ductal carcinoma of the left breast. She reports that she feels well and her pain has been well controlled with ibuprofen. However, she is frustrated that her incisional scar is much larger than she expected. She denies any pain or pruritus associated with the scar. Her past medical history is notable for systemic lupus erythematosus and multiple dermatofibromas on her lower extremities. She has had no other surgeries. She currently takes hydroxychloroquine. On examination, a raised hyperpigmented rubbery scar is noted at the inferior border of the left breast. It appears to have extended beyond the boundaries of the initial incision. Left arm range of motion is limited due to pain at the incisional site. Abnormal deposition of which of the following molecules is most likely responsible for the appearance of this patient’s scar?
- A. Type III collagen
- B. Proteoglycan
- C. Elastin
- D. Type I collagen (Correct Answer)
- E. Type II collagen
Primary vs. secondary intention Explanation: ***Correct: Type I collagen***
- Keloids are characterized by an **overgrowth of dense, disorganized type I collagen fibers** that extend beyond the original wound boundaries. The patient's scar is described as a **"raised, hyperpigmented, rubbery scar" that "extended beyond the boundaries of the initial incision,"** which is characteristic of a keloid.
- Patients with **African American ethnicity**, a history of **dermatofibromas** (which can predispose to keloid formation), and a lack of pain or pruritus are all consistent with a keloid.
- Type I collagen comprises **over 80% of the collagen in mature keloid tissue** and accounts for the characteristic firm, raised appearance.
*Incorrect: Type III collagen*
- **Type III collagen** is prominent during the **initial proliferative phase of wound healing** and is later replaced by type I collagen in mature scars.
- While present early in wound healing, its excessive deposition is not the primary feature of a **mature keloid** that extends beyond the wound margins.
- Normal scars have a type I to type III collagen ratio of approximately 4:1, while keloids have a much higher ratio.
*Incorrect: Proteoglycan*
- **Proteoglycans**, such as decorin and biglycan, are components of the extracellular matrix that play a role in collagen fibril assembly and tissue hydration.
- Although proteoglycans are found in keloids, their **abnormal deposition** is secondary to the extensive collagen formation and not the primary structural molecule responsible for the bulk and characteristic appearance of the scar.
*Incorrect: Elastin*
- **Elastin** provides **elasticity and recoil** to tissues, such as skin, blood vessels, and ligaments.
- Keloids are characterized by **fibrosis and rigidity**, not increased elasticity, and abnormal elastin deposition is not the hallmark of their pathogenesis.
*Incorrect: Type II collagen*
- **Type II collagen** is primarily found in **hyaline cartilage** and vitreous humor, providing resistance to intermittent pressure.
- It is **not a significant component of skin or scar tissue**, making its abnormal deposition irrelevant to the pathogenesis of cutaneous keloids.
Primary vs. secondary intention US Medical PG Question 2: An investigator is studying muscle contraction in tissue obtained from the thigh muscle of an experimental animal. After injection of radiolabeled ATP, the tissue is stimulated with electrical impulses. Radioassay of these muscle cells is most likely to show greatest activity in which of the following structures?
- A. H zone
- B. M line
- C. A band (Correct Answer)
- D. Z line
- E. I band
Primary vs. secondary intention Explanation: ***A band***
- The **A band** contains the entire length of the **thick myosin filaments** along with the **overlap zone** where myosin and actin interact. Myosin has **ATPase activity**, meaning it binds and hydrolyzes **ATP** to power muscle contraction through cross-bridge cycling.
- Therefore, the greatest accumulation of **radiolabeled ATP** and its breakdown products would be found where **myosin heads** are located throughout the A band.
- The A band represents the most complete answer as it encompasses all regions containing myosin ATPase activity.
*H zone*
- The **H zone** is the central part of the **A band** where only **thick myosin filaments** are present, with no overlap with thin actin filaments.
- While myosin heads with ATPase activity are present here and would show radiolabeled ATP, the **H zone** is only a **subset** of the A band. The **A band** is the more comprehensive answer as it includes both the H zone and the overlap regions where most cross-bridge cycling occurs.
*M line*
- The **M line** is the very center of the **H zone** and anchors the **thick filaments**.
- It consists of structural proteins like **myomesin** and **creatine kinase**. While creatine kinase can phosphorylate ADP to regenerate ATP, it does not directly hydrolyze ATP for muscle contraction the way myosin ATPase does.
*Z line*
- The **Z line** (or Z disc) marks the boundaries of a **sarcomere** and anchors the **thin actin filaments**.
- It contains proteins like **alpha-actinin** and **desmin** but does not directly consume ATP for muscle contraction.
*I band*
- The **I band** contains only **thin actin filaments** and extends from the edge of the A band to the Z line.
- While actin is crucial for contraction, it does not possess **ATPase activity**; ATP hydrolysis primarily occurs at the **myosin heads** located in the A band.
Primary vs. secondary intention US Medical PG Question 3: A 14-year-old girl is brought to the physician after she accidentally cut her right forearm earlier that morning while working with her mother's embroidery scissors. She has no history of serious illness. The mother says she went to elementary and middle school abroad and is not sure if she received all of her childhood vaccinations. She appears healthy. Her temperature is 37°C (98.6 °F), pulse 90/min, and blood pressure is 102/68 mm Hg. Examination shows a clean 2-cm laceration on her right forearm with surrounding edema. There is no erythema or discharge. The wound is irrigated with water and washed with soap. Which of the following is the most appropriate next step in management?
- A. Administer Tdap only (Correct Answer)
- B. Administer DTaP only
- C. No further steps are necessary
- D. Administer TIG only
- E. Intravenous metronidazole
Primary vs. secondary intention Explanation: ***Administer Tdap only***
- A 14-year-old with an unknown or incomplete vaccination history requires a **Tdap (tetanus, diphtheria, acellular pertussis) booster** for **tetanus prophylaxis** after a wound.
- The wound is clean, and there are no signs of active infection or high-risk features that would necessitate tetanus immune globulin (TIG).
*Administer DTaP only*
- **DTaP (diphtheria, tetanus, acellular pertussis)** is typically administered to children younger than 7 years of age.
- This patient is 14 years old, making Tdap the more appropriate vaccine formulation for her age group.
*No further steps are necessary*
- Given the patient's **unknown vaccination history** and a laceration, tetanus prophylaxis is crucial to prevent **tetanus**, a potentially life-threatening condition.
- Simply cleaning the wound is insufficient protection without adequate vaccination status.
*Administer TIG only*
- **Tetanus immune globulin (TIG)** is typically reserved for patients with **dirty or severe wounds** and an unknown or incomplete vaccination history, or for those who are immunocompromised.
- This patient has a **clean laceration** with no indication of high-risk features that would warrant TIG.
*Intravenous metronidazole*
- **Metronidazole** is an antibiotic used to treat **anaerobic bacterial infections** and certain parasitic infections.
- The patient has no signs of infection (no erythema, discharge, or fever) that would necessitate antibiotic treatment at this time.
Primary vs. secondary intention US Medical PG Question 4: A 60-year-old male presents with fatigue, dyspnea on exertion, and lower extremity edema. Physical examination reveals an elevated jugular venous pressure and an S3 heart sound. Which of the following medications is most likely to improve this patient's symptoms?
- A. Metoprolol
- B. Furosemide (Correct Answer)
- C. Losartan
- D. Lisinopril
- E. Spironolactone
Primary vs. secondary intention Explanation: ***Correct: Furosemide***
- The patient presents with classic signs of **heart failure with fluid overload**: dyspnea on exertion, lower extremity edema, elevated jugular venous pressure, and an S3 heart sound (indicating volume overload).
- **Furosemide**, a **loop diuretic**, is the most effective medication for **rapid symptomatic relief** in heart failure with congestion. It works by blocking sodium and water reabsorption in the loop of Henle, promoting diuresis and reducing **pulmonary congestion** and **peripheral edema**.
- While other medications like ACE inhibitors, beta-blockers, and aldosterone antagonists are crucial for **long-term mortality reduction** and disease modification, loop diuretics provide the **fastest and most direct symptomatic improvement** for fluid overload.
*Incorrect: Metoprolol*
- **Metoprolol** is a **beta-blocker** that is essential for chronic HFrEF management, providing **mortality reduction** and **reverse cardiac remodeling**.
- However, beta-blockers take **weeks to months** to show symptomatic benefit and can initially **worsen symptoms** due to negative inotropic effects, especially in acute decompensation.
- While important for long-term management, metoprolol does not provide immediate symptomatic relief from fluid overload.
*Incorrect: Losartan*
- **Losartan** is an **angiotensin receptor blocker (ARB)** used as an alternative to ACE inhibitors in HFrEF, particularly in patients who develop cough with ACE inhibitors.
- ARBs reduce **afterload** and prevent **cardiac remodeling**, contributing to improved long-term outcomes and mortality reduction.
- However, they do not directly address fluid overload and do not provide rapid symptomatic relief compared to diuretics.
*Incorrect: Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that improves mortality in HFrEF by preventing myocardial fibrosis, reducing cardiac remodeling, and preventing potassium loss.
- While beneficial for long-term management, spironolactone has **weak diuretic effects** and takes weeks to provide symptomatic benefit.
- It is not the first-line choice for **acute symptomatic relief** of volume overload, though it is an important component of chronic HFrEF therapy.
*Incorrect: Lisinopril*
- **Lisinopril** is an **ACE inhibitor** and a cornerstone of HFrEF therapy, reducing **mortality**, **hospitalizations**, and preventing **cardiac remodeling** by reducing afterload and preload.
- While ACE inhibitors improve symptoms over time, they do not provide the **rapid diuretic effect** needed for immediate relief of dyspnea and edema.
- Lisinopril is essential for long-term management but is not the most effective option for acute symptomatic improvement of fluid overload.
Primary vs. secondary intention US Medical PG Question 5: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Primary vs. secondary intention Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Primary vs. secondary intention US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Primary vs. secondary intention Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Primary vs. secondary intention US Medical PG Question 7: A 35-year-old man is brought to the emergency department 40 minutes after spilling hot oil over himself in a kitchen accident. Examination shows multiple tense blisters over the abdomen, anterior chest, and right upper extremity. On deroofing the blisters, the skin over the right upper extremity is tender, pink, and blanches with pressure. The skin over the abdomen and anterior chest is tender, mottled, and does not blanch with pressure. The left thigh shows erythema only, is tender, and shows quick capillary refill after blanching with pressure. Which of the following most closely approximates the body surface area affected by 2nd-degree burns in this patient?
- A. 45%
- B. 18%
- C. 54%
- D. 9% (Correct Answer)
- E. 36%
Primary vs. secondary intention Explanation: ***9%***
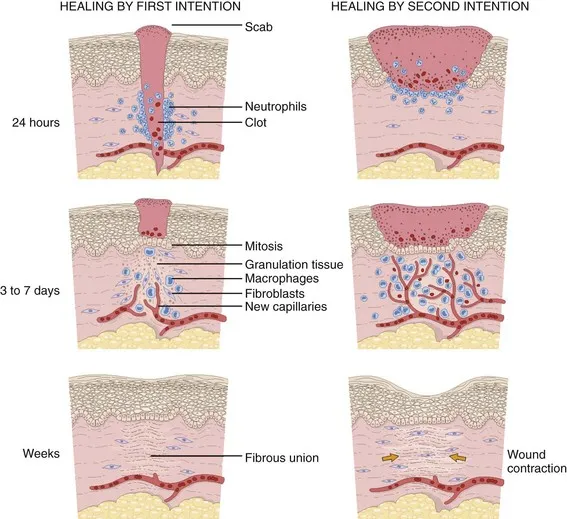
- **2nd-degree (partial-thickness) burns** are characterized by blistering with an intact dermis that remains **painful and blanches with pressure**.
- In this patient, the **right upper extremity** shows tense blisters that, when deroofed, reveal tender, pink skin that **blanches with pressure** - this is consistent with **superficial to mid-partial-thickness (2nd-degree) burns**.
- Using the **Rule of Nines**: the entire upper extremity (arm) = **9%**.
- The abdomen and anterior chest show **mottled, non-blanching skin**, which indicates **full-thickness (3rd-degree) burns**, NOT 2nd-degree.
- The left thigh shows only **erythema with blanching**, consistent with **1st-degree (superficial) burns**.
*18%*
- This would represent two full segments using the Rule of Nines (e.g., both upper extremities or anterior trunk).
- The described 2nd-degree burns affect only the right upper extremity (9%), not two segments.
*36%*
- This would represent the anterior chest (9%) + abdomen (9%) + both upper extremities (18%).
- However, the abdomen and anterior chest show **non-blanching, mottled skin**, indicating **3rd-degree burns**, not 2nd-degree.
*45%*
- This represents approximately half the body surface area.
- Far exceeds the single upper extremity affected by 2nd-degree burns in this patient.
*54%*
- This represents more than half the total body surface area.
- Significantly overestimates the 2nd-degree burn involvement, which is limited to one upper extremity.
Primary vs. secondary intention US Medical PG Question 8: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Primary vs. secondary intention Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
Primary vs. secondary intention US Medical PG Question 9: A 42-year-old man sustains a deep laceration requiring surgical debridement. The wound care team debates between primary closure versus healing by secondary intention. The wound is 6 cm long, 2 cm wide, located on the lower leg with mild contamination from soil exposure, and the patient is a heavy smoker with peripheral vascular disease. Evaluate which approach best synthesizes the risk-benefit analysis for optimal outcome?
- A. Skin grafting after granulation tissue formation
- B. Immediate primary closure with prophylactic antibiotics
- C. Delayed primary closure after 3-5 days of wound observation (Correct Answer)
- D. Healing by secondary intention with negative pressure therapy
- E. Primary closure with tension-relieving retention sutures
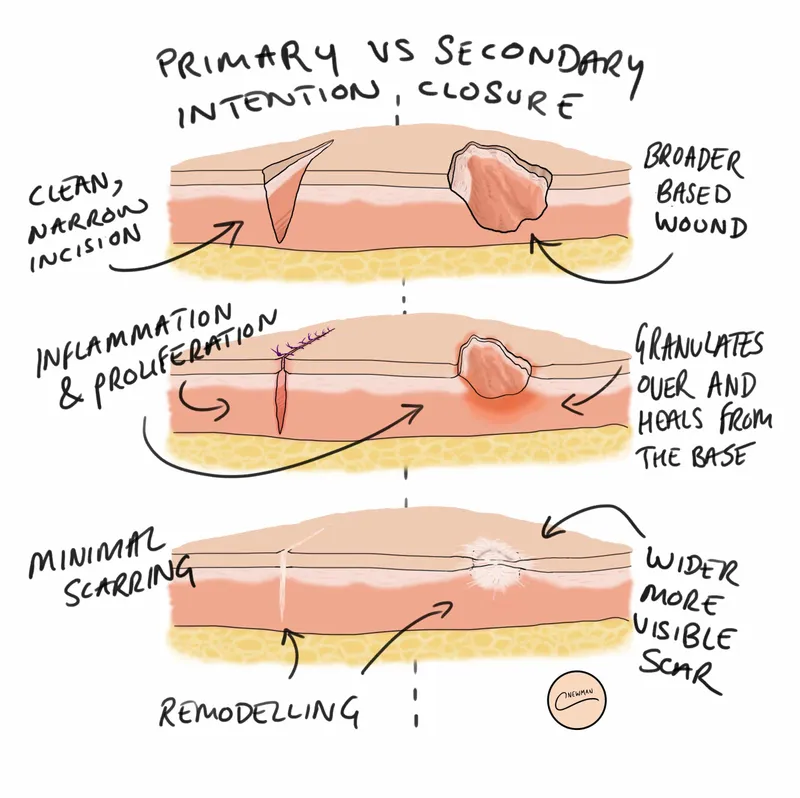
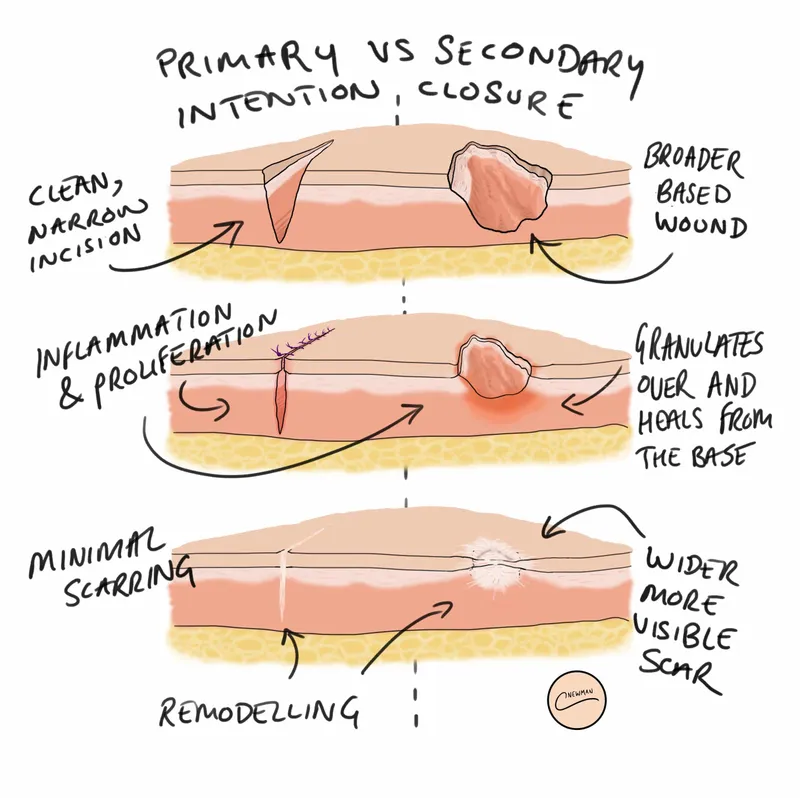
Primary vs. secondary intention Explanation: ***Delayed primary closure after 3-5 days of wound observation***
- This approach, also known as **tertiary intention**, is ideal for **contaminated wounds** as it allows time for the inflammatory phase to reduce bacterial load before final closure.
- It balances the risk of infection from **soil exposure** and **peripheral vascular disease** with the benefit of better functional and cosmetic outcomes compared to secondary intention.
*Skin grafting after granulation tissue formation*
- This technique is typically reserved for **extensive skin loss** or large defects where edges cannot be approximated, which is not indicated for a 6 cm linear laceration.
- It involves a more complex surgical procedure and carries a high risk of failure in patients with **peripheral vascular disease** and **smoking-related** poor microcirculation.
*Immediate primary closure with prophylactic antibiotics*
- Primary closure of a **contaminated wound** significantly increases the risk of **wound dehiscence** and abscess formation, especially in a low-perfusion area like the lower leg.
- The patient’s history of **smoking** and **vascular disease** further impairs oxygen delivery and immune response, making immediate closure premature.
*Healing by secondary intention with negative pressure therapy*
- While this reduces infection risk, it leads to a prolonged healing period and significant **scar contracture**, which can impair movement on the lower leg.
- It is less efficient than delayed primary closure for a cleanable laceration and is usually reserved for **chronically infected** or non-approximable wounds.
*Primary closure with tension-relieving retention sutures*
- Placing sutures under tension in a patient with **peripheral vascular disease** further compromises **capillary perfusion**, leading to skin flap necrosis.
- Retention sutures do not address the primary concern of **bacterial contamination** from the soil, which remains trapped within the closed wound space.
Primary vs. secondary intention US Medical PG Question 10: A 35-year-old woman with known deficiency in Ehlers-Danlos syndrome presents with recurrent wound dehiscence following multiple abdominal surgeries. Genetic testing confirms a mutation affecting type III collagen synthesis. She now requires another laparotomy for adhesive bowel obstruction. The surgical team must decide on closure technique. Synthesizing knowledge of collagen biochemistry and surgical principles, which approach best addresses her specific wound healing defect?
- A. Vacuum-assisted closure followed by skin grafting
- B. Standard layer closure with permanent sutures only
- C. Delayed primary closure after 5-7 days
- D. Retention sutures with permanent mesh reinforcement (Correct Answer)
- E. Biological mesh with early suture removal
Primary vs. secondary intention Explanation: ***Retention sutures with permanent mesh reinforcement***
- In patients with **Vascular Ehlers-Danlos syndrome (Type IV)**, deficiency in **Type III collagen** results in inherently weak connective tissue that never reaches normal tensile strength.
- **Retention sutures** distribute tension across a larger surface area, and **permanent mesh** provides life-long mechanical reinforcement to compensate for the permanent **collagen synthesis defect**.
*Vacuum-assisted closure followed by skin grafting*
- While useful for infected wounds, this approach does not provide the **structural integrity** required to prevent future dehiscence or incisional hernias.
- **Skin grafts** do not address the primary issue of **fascial weakness** and tensile failure in deep tissue layers.
*Standard layer closure with permanent sutures only*
- Standard techniques are insufficient because the patient's tissues are too **fragile** to hold individual sutures under the stress of abdominal pressure.
- Permanent sutures may "cheese-wire" through the weak **collagen-deficient fascia**, leading to immediate or early **wound dehiscence**.
*Delayed primary closure after 5-7 days*
- This technique is primarily used to reduce **surgical site infection** risk in contaminated wounds but does not alter the biochemical quality of collagen.
- It fails to address the fundamental problem of **poor wound healing** and mechanical fragility seen in **Ehlers-Danlos syndrome**.
*Biological mesh with early suture removal*
- **Biological meshes** are designed to be resorbed and replaced by host collagen, which in this patient would still be defective **Type III collagen**.
- **Early suture removal** is contraindicated as these patients require prolonged or permanent mechanical support due to delayed and **incomplete wound maturation**.
More Primary vs. secondary intention US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.