Pressure ulcers staging and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pressure ulcers staging and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pressure ulcers staging and management US Medical PG Question 1: A 43-year-old woman comes to the physician because of a 3-month history of a painless ulcer on the sole of her right foot. There is no history of trauma. She has been dressing the ulcer once daily at home with gauze. She has a 15-year history of poorly-controlled type 1 diabetes mellitus and hypertension. Current medications include insulin and lisinopril. Vital signs are within normal limits. Examination shows a 2 x 2-cm ulcer on the plantar aspect of the base of the great toe with whitish, loose tissue on the floor of the ulcer and a calloused margin. A blunt metal probe reaches the deep plantar space. Sensation to vibration and light touch is decreased over both feet. Pedal pulses are intact. An x-ray of the right foot shows no abnormalities. Which of the following is the most appropriate initial step in management?
- A. Surgical revascularization of the right foot
- B. Amputation of the right forefoot
- C. Total contact casting of right foot
- D. Intravenous antibiotic therapy
- E. Sharp surgical debridement of the ulcer (Correct Answer)
Pressure ulcers staging and management Explanation: ***Sharp surgical debridement of the ulcer***
- The presence of a **painless ulcer**, decreased sensation (neuropathy), and a calloused margin with loose tissue indicates a **neuropathic ulcer** common in diabetic patients. **Sharp surgical debridement** is crucial to remove non-viable tissue and promote healing.
- The probe reaching the deep plantar space suggests a potential deep infection or osteomyelitis, which needs aggressive debridement to remove all infected and necrotic tissue. However, since the X-ray is normal, it is less likely to have osteomyelitis, but it needs to be ruled out by further investigations.
*Surgical revascularization of the right foot*
- This is primarily indicated for **ischemic ulcers** where blood supply is compromised.
- The patient has **intact pedal pulses**, meaning good distal blood flow, making revascularization unnecessary at this stage.
*Amputation of the right forefoot*
- Amputation is a measure of last resort for **severe, non-healing ulcers** with extensive infection or gangrene that fail to respond to conservative and surgical debridement.
- The current presentation does not warrant such an extreme intervention as a first step.
*Total contact casting of right foot*
- **Total contact casting** is used for **off-loading pressure** from a neuropathic ulcer to facilitate healing.
- While it's an important step in management, it should generally follow **debridement** to ensure a clean wound bed.
*Intravenous antibiotic therapy*
- This is indicated if there are definitive signs of **spreading infection** (e.g., cellulitis, fever, purulence).
- While debridement helps prevent infection by removing necrotic tissue, there is no mention of systemic signs of infection or severe local infection requiring immediate IV antibiotics.
Pressure ulcers staging and management US Medical PG Question 2: A 15-year-old boy is brought to the emergency department by ambulance after his mother found him having muscle spasms and stiffness in his room. His mother stated he scraped his foot on a rusty razor on the bathroom floor 2 days prior. On presentation, his temperature is 102.0°F (38.9°C), blood pressure is 108/73 mmHg, pulse is 122/min, and respirations are 18/min. On physical exam, he is found to have severe muscle spasms and rigid abdominal muscles. In addition, he has a dirty appearing wound on his right foot. The patient's mother does not recall any further vaccinations since age 12. Finally, he is found to have difficulty opening his mouth so he is intubated. Which of the following treatment(s) should be provided to this patient?
- A. Wound debridement and antitoxin
- B. Antitoxin
- C. Wound debridement
- D. Wound debridement and booster vaccine
- E. Wound debridement, antitoxin, and booster vaccine (Correct Answer)
Pressure ulcers staging and management Explanation: ***Wound debridement, antitoxin, and booster vaccine***
- The patient presents with classic symptoms of **tetanus** (muscle spasms, stiffness, trismus, fever) following a contaminated wound, and an uncertain vaccination history.
- **Wound debridement** removes the source of toxin production, **antitoxin** (tetanus immune globulin) neutralizes circulating toxin, and a **booster vaccine** provides active immunity against future infections.
*Wound debridement and antitoxin*
- While **wound debridement** and **antitoxin** are critical for acute management, omitting the booster vaccine leaves the patient vulnerable to future tetanus infections.
- A booster dose is essential to stimulate the patient's own immune system and provide **long-term immunity**, especially with a history of unknown vaccination status.
*Antitoxin*
- Administering only **antitoxin** would neutralize circulating toxins but would not address the ongoing production of toxins from the contaminated wound.
- It also wouldn't provide **active immunization** to protect against future exposures.
*Wound debridement*
- **Wound debridement** alone removes the bacterial source but does not neutralize the already circulating **tetanus toxin**, which is responsible for the severe neurological symptoms.
- It also fails to provide immediate passive immunity with antitoxin or active immunization with a booster.
*Wound debridement and booster vaccine*
- This option correctly addresses removing the source and providing active immunity but critically misses the immediate need for **antitoxin** to neutralize existing toxins and alleviate the life-threatening symptoms.
- The **tetanus toxin** acts rapidly, and prompt neutralization is crucial to prevent further neurological damage and improve prognosis.
Pressure ulcers staging and management US Medical PG Question 3: A 16-year-old boy presents to the emergency department after a skateboarding accident. He fell on a broken bottle and received a 4 cm wound on the dorsal aspect of his left hand. His vitals are stable and he was evaluated by the surgeon on call who determined that suturing was not required. After several weeks the wound has almost completely healed (see image). Which of the following is the correct description of this patient's wound before healing?
- A. Incised wound (Correct Answer)
- B. Abrasion
- C. Laceration
- D. Avulsion
- E. Puncture
Pressure ulcers staging and management Explanation: ***Incised wound***
- An **incised wound** is caused by a sharp object, such as a broken bottle, resulting in a clean, straight cut with well-defined edges and minimal tissue damage.
- The characteristics of the injury (sharp object mechanism, 4 cm linear wound) and the clinical decision that suturing was not required suggest a relatively clean incised wound with edges that could approximate well.
- Incised wounds typically heal with **fine linear scars** as shown in the image, especially when the edges are well-approximated.
*Abrasion*
- An abrasion is a **superficial wound** caused by friction or scraping, leading to removal of the epidermis and sometimes the superficial dermis.
- This mechanism does not match the described injury from a broken bottle, and abrasions produce broad, shallow wounds rather than deep linear cuts.
- Abrasions heal with minimal scarring and would not produce the linear scar pattern shown.
*Laceration*
- A laceration is a wound with **irregular, torn edges** typically caused by blunt force trauma or crushing injury.
- While broken glass can sometimes cause lacerations, the description of a clean "4 cm wound" from falling on a broken bottle more strongly suggests a sharp cutting mechanism rather than tearing.
- Lacerations have jagged edges with more tissue damage and typically require debridement or careful closure.
*Avulsion*
- An **avulsion** involves forcible tearing away of tissue, often resulting in significant tissue loss with irregular, gaping wounds.
- This injury pattern is much more severe than described and would typically require complex surgical management, including possible skin grafting.
- The mechanism (falling on broken glass) and the relatively straightforward healing do not support an avulsion injury.
*Puncture*
- A puncture wound is caused by a **pointed object** penetrating the skin, creating a small entry hole with depth greater than width.
- The description of a "4 cm wound" indicates a linear length, not a deep narrow penetration typical of puncture wounds.
- Puncture wounds carry high infection risk and would not produce the linear scar pattern shown in the image.
Pressure ulcers staging and management US Medical PG Question 4: A 54-year-old male carpenter accidentally amputated his right thumb while working in his workshop 30 minutes ago. He reports that he was cutting a piece of wood, and his hand became caught up in the machinery. He is calling the emergency physician for advice on how to transport his thumb and if it is necessary. Which of the following is the best information for this patient?
- A. Place thumb in cup of cold milk
- B. Wrap thumb in saline-moistened, sterile gauze and place in sterile bag (Correct Answer)
- C. Wrap thumb in sterile gauze and submerge in a cup of saline
- D. There is no need to save the thumb
- E. Place thumb directly into cooler of ice
Pressure ulcers staging and management Explanation: ***Wrap thumb in saline-moistened, sterile gauze and place in sterile bag***
- This method provides a **moist, sterile environment** for the amputated part, which is crucial for preserving tissue viability.
- The use of a sterile bag helps prevent contamination and allows the part to be placed inside a cooler without direct ice contact, preventing **frostbite**.
*Place thumb in cup of cold milk*
- While cold milk might offer some cooling, it is **not sterile** and could introduce bacteria, increasing the risk of infection.
- Milk's composition is **not ideal for cell preservation** compared to saline, which is more isotonic.
*Wrap thumb in sterile gauze and submerge in a cup of saline*
- Submerging the amputated part directly in saline, even with sterile gauze, can lead to **tissue maceration** due to overhydration.
- This method also makes it more difficult to prevent contamination during transportation if the cup is not sealed.
*There is no need to save the thumb*
- **Replantation surgery** is often possible and highly desirable for thumb amputations due to its critical functional role.
- Dismissing the amputated part would deprive the patient of a chance to restore function, especially given the short time since amputation.
*Place thumb directly into cooler of ice*
- Direct contact with ice can cause **frostbite** and **tissue damage**, compromising the viability of the amputated part.
- The preferred method is to keep the amputated part cool, but not frozen, usually by placing it in a sealed bag within an ice-filled container.
Pressure ulcers staging and management US Medical PG Question 5: A 42-year-old man presents to the physician with a painful ulcer in the mouth for 1 week. He has had similar episodes of ulcers over the past year. Every episode lasts about a week and heals without leaving a scar. He has also had similar ulcers on the scrotum, but the ulcers have left scars. He takes no medications. His temperature is 36.8°C (98.2°F), and the rest of the vital signs are stable. On physical examination, a 1-cm yellowish ulcer with a necrotic base is seen on the right buccal mucosa. Also, there are several tender nodules of different sizes on both shins. An image of one of the nodules is shown. Which of the following is the most likely complication of this patient’s current condition?
- A. Uveitis (Correct Answer)
- B. Cerebral vein thrombosis
- C. Pulmonary embolism
- D. Gastrointestinal ulceration
- E. Deforming arthritis
Pressure ulcers staging and management Explanation: ***Uveitis***
- The constellation of **recurrent oral and genital ulcers**, **skin lesions** (erythema nodosum-like nodules on the shins), and positive pathergy test (implied by the "scars" from ulcers which may suggest an exaggerated skin response) is highly suggestive of **Behçet's disease**.
- **Uveitis** is a common and serious ocular complication of Behçet's disease, often leading to visual impairment or blindness if untreated.
*Cerebral vein thrombosis*
- While **central nervous system (CNS) involvement** can occur in Behçet's disease, leading to various neurological symptoms including **thrombosis**, it is less common than ocular complications like uveitis.
- **Cerebral vein thrombosis** is a severe but less frequent manifestation compared to the high prevalence of ocular involvement.
*Pulmonary embolism*
- **Vascular involvement**, including thrombophlebitis and arterial aneurysms, is a known feature of Behçet's disease, increasing the risk of **thrombosis**.
- However, **pulmonary embolism** specifically is a less frequent direct complication compared to other arterial or venous thromboses, and ocular issues are more prevalent.
*Gastrointestinal ulceration*
- Behçet's disease can affect the **gastrointestinal tract**, causing **ulcerations**, particularly in the ileocecal region.
- While a possible complication, gastrointestinal involvement is not as universally noted or as likely to be the *most likely* complication as uveitis, which affects a higher percentage of patients.
*Deforming arthritis*
- **Arthritis** is a common manifestation in Behçet's disease, typically presenting as **non-erosive and non-deforming** polyarthritis, predominantly affecting large joints like the knees and ankles.
- Unlike conditions like rheumatoid arthritis, Behçet's-associated arthritis rarely leads to **joint destruction or deformity**.
Pressure ulcers staging and management US Medical PG Question 6: A 72-year-old man is seen in the hospital for a sacral rash. The patient has been hospitalized for the past 3 weeks for a heart failure exacerbation. When the nurse went to bathe him this morning, she noticed a red rash over his sacrum. The patient reports mild discomfort and denies pruritus. The patient has chronic kidney disease, urinary incontinence, ischemic cardiomyopathy, gout, and poor mobility. His current medications include aspirin, furosemide, metoprolol, lisinopril, spironolactone, and prednisone that was started for a recent gout flare. The patient’s temperature is 97°F (37.2°C), blood pressure is 110/62 mmHg, pulse is 68/min, and respirations are 13/min with an oxygen saturation of 98% on room air. On physical examination, there is a 4 cm x 6 cm patch of non-blanchable erythema over the patient’s sacrum that is mildly tender to palpation. Labs are obtained, as shown below:
Leukocyte count: 10,000/mm^3 with normal differential
Hemoglobin: 15.2 g/dL
Platelet count: 400,000/mm^3
Serum:
Na: 138 mEq/L
K+: 4.3 mEq/L
Cl-: 104 mEq/L
HCO3-: 25 mEq/L
BUN: 26 mg/dL
Creatinine: 1.5 mg/dL
Glucose: 185 mg/dL
A hemoglobin A1c is pending. Which of the following is the best management for the patient’s most likely diagnosis?
- A. Surgical debridement
- B. Repositioning (Correct Answer)
- C. Topical silver sulfadiazine
- D. Metformin
- E. Prophylactic oral ciprofloxacin
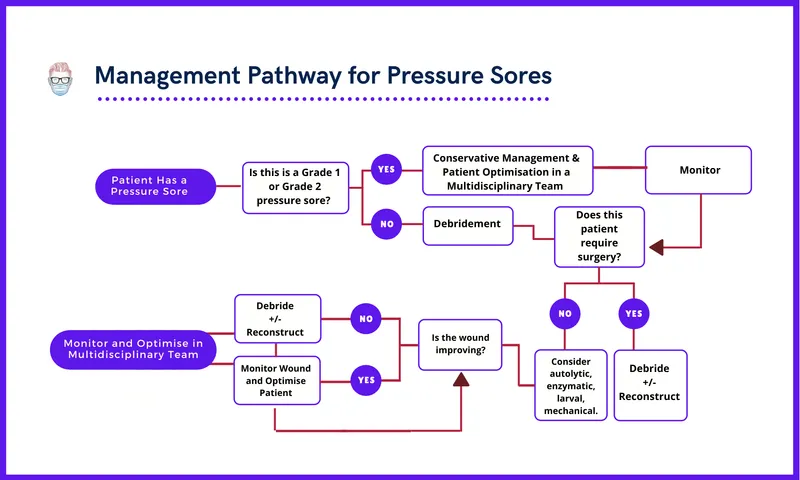
Pressure ulcers staging and management Explanation: ***Repositioning***
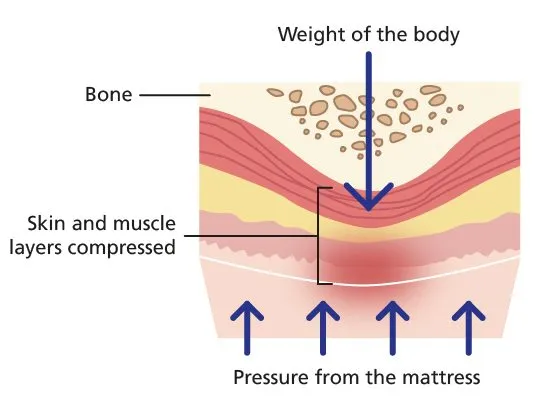
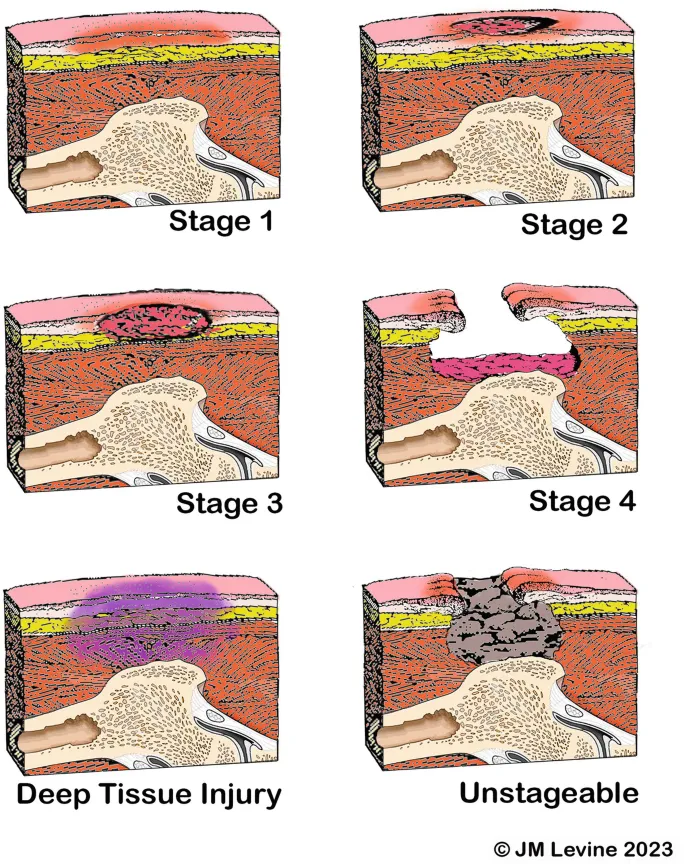
- The patient's presentation of a **non-blanchable erythematous rash** over the sacrum in a bedridden patient indicates a **Stage 1 pressure injury**.
- **Repositioning** is the cornerstone of management for preventing progression and promoting healing of pressure injuries by relieving pressure on affected areas.
*Surgical debridement*
- This is typically reserved for **Stage 3 or 4 pressure ulcers** with significant tissue necrosis or infection, which is not present in a Stage 1 injury.
- Debridement would be unnecessary and potentially harmful for an intact, non-infected area of non-blanchable erythema.
*Topical silver sulfadiazine*
- This is an **antimicrobial cream** used for burn wounds and infected ulcers.
- It is not indicated for a Stage 1 pressure injury, which is characterized by intact skin without infection or open wounds.
*Metformin*
- **Metformin** is an oral hypoglycemic agent used to manage type 2 diabetes.
- While the patient's elevated glucose and pending HbA1c suggest potential diabetes or stress hyperglycemia, metformin does not directly address the sacral rash.
*Prophylactic oral ciprofloxacin*
- **Prophylactic antibiotics** are generally not indicated for Stage 1 pressure injuries, as there is no evidence of infection.
- Unnecessary antibiotic use can contribute to **antibiotic resistance** and potential side effects.
Pressure ulcers staging and management US Medical PG Question 7: An 8-year-old boy is shifted to a post-surgical floor following neck surgery. The surgeon has restricted his oral intake for the next 24 hours. He does not have diarrhea, vomiting, or dehydration. His calculated fluid requirement is 1500 mL/day. However, he receives 2000 mL of intravenous isotonic fluids over 24 hours. Which of the following physiological parameters in the boy’s circulatory system is most likely to be increased?
- A. Interstitial oncotic pressure
- B. Interstitial hydrostatic pressure
- C. Capillary wall permeability
- D. Capillary oncotic pressure
- E. Capillary hydrostatic pressure (Correct Answer)
Pressure ulcers staging and management Explanation: ***Capillary hydrostatic pressure***
- Giving 2000 mL of intravenous isotonic fluids when the calculated requirement is 1500 mL/day leads to a **positive fluid balance** and **fluid overload**.
- This excess fluid directly increases the **intravascular volume**, thereby raising the **capillary hydrostatic pressure**, which pushes fluid out of the capillaries.
*Interstitial oncotic pressure*
- This pressure is primarily determined by the **protein concentration** in the interstitial fluid.
- While fluid overload can dilute interstitial proteins, it generally does not directly increase interstitial oncotic pressure; rather, it might decrease it due to fluid movement.
*Interstitial hydrostatic pressure*
- As fluid moves out of the capillaries due to increased capillary hydrostatic pressure, the **interstitial hydrostatic pressure** will also increase.
- However, the primary driving force for this change, and thus the most direct consequence of fluid overload, is the increase in capillary hydrostatic pressure.
*Capillary wall permeability*
- This parameter refers to the ease with which substances, including fluid and proteins, can cross the capillary wall.
- Fluid overload does not typically affect **capillary wall permeability** unless there is an underlying condition causing inflammation or damage to the capillary endothelium.
*Capillary oncotic pressure*
- This pressure is mainly determined by the **protein concentration** within the capillaries.
- In a state of fluid overload with isotonic fluids, the plasma proteins are diluted, leading to a **decrease** in capillary oncotic pressure, not an increase.
Pressure ulcers staging and management US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pressure ulcers staging and management Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pressure ulcers staging and management US Medical PG Question 9: A 39-year-old man comes to the physician for a follow-up examination. He was treated for a urinary tract infection with trimethoprim-sulfamethoxazole 2 months ago. He is paraplegic as a result of a burst lumbar fracture that occurred after a fall 5 years ago. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He performs clean intermittent catheterization daily. He has smoked one pack of cigarettes daily for 19 years. His temperature is 37.1°C (98.8°F), pulse is 95/min, respirations are 14/min, and blood pressure is 120/80 mm Hg. He appears malnourished. Examination shows palpable pedal pulse. Multiple dilated tortuous veins are present over both lower extremities. There is a 2-cm wound surrounded by partial-thickness loss of skin and a pink wound bed over the right calcaneum. Neurologic examination shows paraparesis. His hemoglobin A1c is 6.5%, and fingerstick blood glucose concentration is 134 mg/dL. Which of the following is most likely to have prevented this patient's wound?
- A. Broad-spectrum antibiotic therapy
- B. Cessation of smoking
- C. Heparin therapy
- D. Topical antibiotic therapy
- E. Frequent position changes (Correct Answer)
Pressure ulcers staging and management Explanation: ***Frequent position changes***
- This patient is paraplegic, which increases his risk for **pressure ulcers** due to prolonged immobility and sustained pressure on bony prominences like the calcaneum.
- **Frequent repositioning** redistributes pressure, preventing skin breakdown and promoting circulation, thereby avoiding pressure injuries.
*Broad-spectrum antibiotic therapy*
- The wound is described as a **partial-thickness loss** with a pink wound bed, suggesting it's not primarily an infected wound requiring broad-spectrum antibiotics to prevent its formation.
- Antibiotics are used to **treat existing infections**, not prevent pressure ulcers in a non-infected state.
*Cessation of smoking*
- While **smoking impairs wound healing** and overall vascular health, it is not the most direct or primary preventative measure for a pressure ulcer caused by immobility.
- Smoking cessation would improve **long-term vascular health** and *ulcer healing*, but frequent position changes addresses the immediate cause of pressure.
*Heparin therapy*
- **Heparin** is an anticoagulant used to prevent **thrombosis** (blood clots), which is not the primary mechanism behind pressure ulcer formation.
- While immobility can contribute to deep vein thrombosis, heparin would not prevent the **mechanical pressure-induced skin damage** that causes a calcaneal wound.
*Topical antibiotic therapy*
- Similar to systemic antibiotics, topical antibiotics are used for **treating localized infections** or preventing them in *open wounds*.
- This wound is a result of pressure, and preventing its formation requires addressing the pressure itself, not merely applying antibiotics to the skin surface.
Pressure ulcers staging and management US Medical PG Question 10: A patient presents to the emergency department with arm pain. The patient recently experienced an open fracture of his radius when he fell from a ladder while cleaning his house. Surgical reduction took place and the patient's forearm was put in a cast. Since then, the patient has experienced worsening pain in his arm. The patient has a past medical history of hypertension and asthma. His current medications include albuterol, fluticasone, loratadine, and lisinopril. His temperature is 99.5°F (37.5°C), blood pressure is 150/95 mmHg, pulse is 90/min, respirations are 19/min, and oxygen saturation is 99% on room air. The patient's cast is removed. On physical exam, the patient's left arm is tender to palpation. Passive motion of the patient's wrist and fingers elicits severe pain. The patient's left radial and ulnar pulse are both palpable and regular. The forearm is soft and does not demonstrate any bruising but is tender to palpation. Which of the following is the next best step in management?
- A. Replace the cast with a sling
- B. Measurement of compartment pressure (Correct Answer)
- C. Ibuprofen and reassurance
- D. Emergency fasciotomy
- E. Radiography
Pressure ulcers staging and management Explanation: ***Measurement of compartment pressure***
- The patient exhibits classic signs of **compartment syndrome**, including severe pain out of proportion to injury, pain with passive stretching, and a history of trauma followed by casting. Measuring compartment pressure is crucial for diagnosis despite palpable pulses.
- Early measurement of compartment pressures can confirm the diagnosis and guide the decision for an **emergency fasciotomy** to prevent irreversible tissue damage.
*Replace the cast with a sling*
- This action would likely worsen the patient's condition by delaying the diagnosis and treatment of potential **compartment syndrome**.
- A sling does not address the underlying issue of increased pressure within the muscle compartments.
*Ibuprofen and reassurance*
- Administering **Ibuprofen (NSAID)** might mask the pain but will not resolve the increased pressure within the compartment, which is a surgical emergency.
- Reassurance without proper assessment of compartment syndrome could lead to irreversible muscle and nerve damage.
*Emergency fasciotomy*
- While a fasciotomy is the definitive treatment for confirmed compartment syndrome, it should only be performed **after compartment pressures have been measured** and the diagnosis confirmed, unless the clinical suspicion is extremely high and pressures cannot be obtained.
- Performing a fasciotomy without objective confirmation is generally not the immediate next step, as it is an invasive procedure with its own risks.
*Radiography*
- **Radiography** would be useful to assess the healing of the fracture or rule out new fractures, but it will not provide information about the soft tissue pressure changes characteristic of compartment syndrome.
- The patient's symptoms are more indicative of a circulatory or soft tissue issue rather than a new bony problem.
More Pressure ulcers staging and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.