Phases of wound healing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Phases of wound healing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Phases of wound healing US Medical PG Question 1: A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?
- A. Fibroblasts
- B. Myofibroblasts (Correct Answer)
- C. Neutrophils
- D. Macrophages
- E. Endothelial cells
Phases of wound healing Explanation: ***Myofibroblasts***
- The patient presents with a **contracture** (restricted range of motion and hyperextension of the hand due to a thick scar) after a burn, which is characteristic of the action of **myofibroblasts**.
- Myofibroblasts are specialized cells that possess features of both fibroblasts (synthesizing **collagen** and extracellular matrix) and smooth muscle cells (containing **actin microfilaments**), allowing them to exert contractile force which leads to scar contraction.
*Fibroblasts*
- While fibroblasts are crucial for **wound healing** by producing collagen and other extracellular matrix components, they primarily lay down the foundation for scar tissue.
- They lack the strong contractile capabilities that lead to significant **tissue retraction** and contracture.
*Neutrophils*
- Neutrophils are **acute inflammatory cells** that primarily function in the early stages of wound healing to phagocytose debris and pathogens.
- They do not play a direct role in the formation of **scar tissue** or **contractures**.
*Macrophages*
- Macrophages are important **immune cells** involved in clearing debris, presenting antigens, and releasing growth factors during the later stages of wound healing.
- They also influence fibroblast activity, but they do not directly cause **tissue contraction** or scar formation.
*Endothelial cells*
- Endothelial cells line **blood vessels** and are essential for **angiogenesis** (formation of new blood vessels) during wound healing.
- They are not involved in the **contractile process** that leads to scar contracture.
Phases of wound healing US Medical PG Question 2: A 55-year-old African American female presents to her breast surgeon for a six-month follow-up visit after undergoing a modified radical mastectomy for invasive ductal carcinoma of the left breast. She reports that she feels well and her pain has been well controlled with ibuprofen. However, she is frustrated that her incisional scar is much larger than she expected. She denies any pain or pruritus associated with the scar. Her past medical history is notable for systemic lupus erythematosus and multiple dermatofibromas on her lower extremities. She has had no other surgeries. She currently takes hydroxychloroquine. On examination, a raised hyperpigmented rubbery scar is noted at the inferior border of the left breast. It appears to have extended beyond the boundaries of the initial incision. Left arm range of motion is limited due to pain at the incisional site. Abnormal deposition of which of the following molecules is most likely responsible for the appearance of this patient’s scar?
- A. Type III collagen
- B. Proteoglycan
- C. Elastin
- D. Type I collagen (Correct Answer)
- E. Type II collagen
Phases of wound healing Explanation: ***Correct: Type I collagen***
- Keloids are characterized by an **overgrowth of dense, disorganized type I collagen fibers** that extend beyond the original wound boundaries. The patient's scar is described as a **"raised, hyperpigmented, rubbery scar" that "extended beyond the boundaries of the initial incision,"** which is characteristic of a keloid.
- Patients with **African American ethnicity**, a history of **dermatofibromas** (which can predispose to keloid formation), and a lack of pain or pruritus are all consistent with a keloid.
- Type I collagen comprises **over 80% of the collagen in mature keloid tissue** and accounts for the characteristic firm, raised appearance.
*Incorrect: Type III collagen*
- **Type III collagen** is prominent during the **initial proliferative phase of wound healing** and is later replaced by type I collagen in mature scars.
- While present early in wound healing, its excessive deposition is not the primary feature of a **mature keloid** that extends beyond the wound margins.
- Normal scars have a type I to type III collagen ratio of approximately 4:1, while keloids have a much higher ratio.
*Incorrect: Proteoglycan*
- **Proteoglycans**, such as decorin and biglycan, are components of the extracellular matrix that play a role in collagen fibril assembly and tissue hydration.
- Although proteoglycans are found in keloids, their **abnormal deposition** is secondary to the extensive collagen formation and not the primary structural molecule responsible for the bulk and characteristic appearance of the scar.
*Incorrect: Elastin*
- **Elastin** provides **elasticity and recoil** to tissues, such as skin, blood vessels, and ligaments.
- Keloids are characterized by **fibrosis and rigidity**, not increased elasticity, and abnormal elastin deposition is not the hallmark of their pathogenesis.
*Incorrect: Type II collagen*
- **Type II collagen** is primarily found in **hyaline cartilage** and vitreous humor, providing resistance to intermittent pressure.
- It is **not a significant component of skin or scar tissue**, making its abnormal deposition irrelevant to the pathogenesis of cutaneous keloids.
Phases of wound healing US Medical PG Question 3: A 3-week-old boy is brought to the pediatrician by his parents for a circumcision. The circumcision was uncomplicated; however, after a few hours, the diaper contained blood, and the bleeding has not subsided. A complete blood count was ordered, which was significant for a platelet count of 70,000/mm3. On peripheral blood smear, the following was noted (figure A). The prothrombin time was 12 seconds, partial thromboplastin time was 32 seconds, and bleeding time was 13 minutes. On platelet aggregation studies, there was no response with ristocetin. This result was not corrected with the addition of normal plasma. There was a normal aggregation response with the addition of ADP. Which of the following is most likely true of this patient's underlying disease?
- A. Protein C resistance
- B. Decreased GpIb (Correct Answer)
- C. Responsive to desmopressin
- D. Adding epinephrine would not lead to platelet aggregation
- E. Decreased GpIIb/IIIa
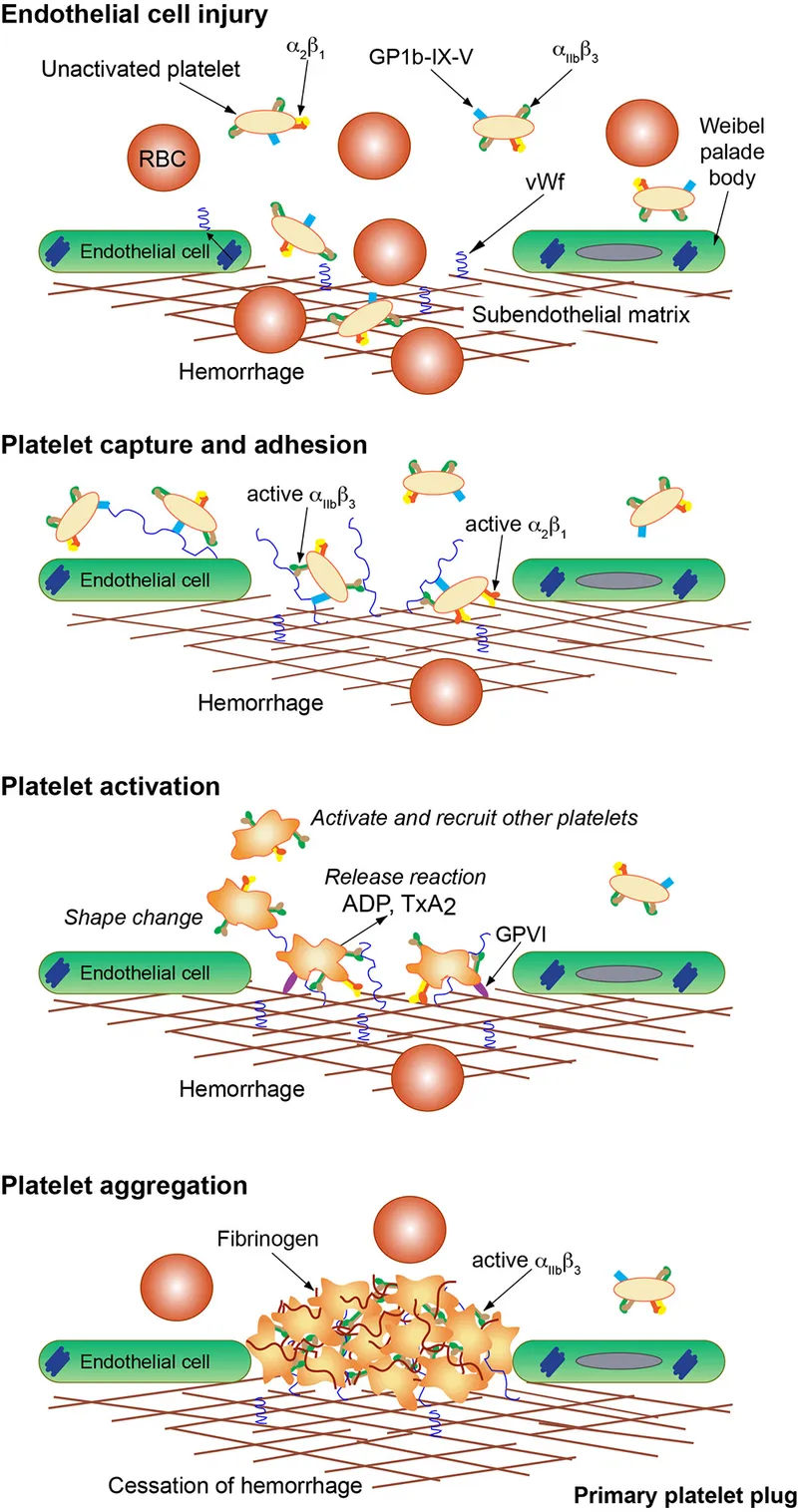
Phases of wound healing Explanation: ***Decreased GpIb***
- The presentation of **persistent severe bleeding** after circumcision, **thrombocytopenia (70,000/mm3)**, and **giant platelets** on blood smear are classic findings for **Bernard-Soulier syndrome**.
- **Bernard-Soulier syndrome** is characterized by a defect in the platelet glycoprotein Ib-IX-V (GpIb) complex, which is crucial for **platelet adhesion** to **von Willebrand factor (vWF)** on exposed subendothelium. The **lack of aggregation response to ristocetin** (which induces vWF binding to GpIb) and its **non-correction with normal plasma** further confirm this diagnosis.
*Protein C resistance*
- **Protein C resistance** is associated with an **increased risk of thrombosis**, not bleeding, and is typically due to a mutation in **Factor V (Factor V Leiden)**, which makes it resistant to inactivation by activated Protein C.
- This condition would manifest with **venous thromboembolism** or recurrent miscarriages, which contradicts the patient's bleeding symptoms.
*Responsive to desmopressin*
- **Desmopressin** (DDAVP) primarily acts by releasing **von Willebrand factor (vWF)** and **Factor VIII** from endothelial cells. It is effective in certain types of **von Willebrand disease** and **mild hemophilia A**.
- Since the issue here is with the **platelet receptor (GpIb)** for vWF, and not with vWF quantity or quality, desmopressin would **not be an effective treatment** for Bernard-Soulier syndrome.
*Adding epinephrine would not lead to platelet aggregation*
- In **Bernard-Soulier syndrome**, the defect is specific to the **GpIb-vWF interaction**. Platelet aggregation responses to other agonists like **ADP, collagen, and epinephrine** are typically **normal** or at least partially preserved, although the defect in GpIb can subtly impair secondary aggregation.
- The aggregation studies showing a **normal response to ADP** in this patient support that other aggregation pathways are intact, making this statement incorrect.
*Decreased GpIIb/IIIa*
- **Decreased GpIIb/IIIa** (or qualitative defects in it) is characteristic of **Glanzmann thrombasthenia**, another inherited platelet disorder.
- Patients with Glanzmann thrombasthenia also present with **bleeding** and **impaired platelet aggregation**, but their platelets are usually **normal in size and count**, and they show **absent aggregation to ADP, collagen, and epinephrine**, while aggregation to ristocetin is normal, which is different from this patient's findings.
Phases of wound healing US Medical PG Question 4: A 28-year-old woman and her husband are admitted to the office due to difficulties conceiving a child for the past year. Her menarche was at the age of 15 years, and her periods have been regular since then. Her medical history is positive for an abortion with curettage 5 years ago. A spermogram on the partner is performed, and it shows motile sperm cells. An ultrasound is performed on the patient and it is unremarkable. The laboratory results show that the FSH, LH, TSH, and prolactin levels are within normal ranges. A hysteroscopy is additionally performed and multiple adhesions are found in the uterus (refer to the image). Which of the following is the most likely composition of the scar tissue present in the uterus?
- A. Type 3 collagen
- B. Type 4 collagen
- C. Type 2 collagen
- D. Type 1 collagen (Correct Answer)
- E. Elastin
Phases of wound healing Explanation: ***Type 1 collagen***
- This patient presents with **Asherman's syndrome**, characterized by intrauterine adhesions, often following uterine surgery like **curettage**. These adhesions are primarily composed of **Type 1 collagen**, which is the most abundant type of collagen in the human body and a major component of scar tissue.
- **Type 1 collagen** provides tensile strength and is crucial for wound healing and forming scar tissue in most connective tissues, including the uterus.
*Type 3 collagen*
- **Type 3 collagen** is found in distensible tissues like blood vessels, the uterus, and skin, and is important during the **early stages of wound healing**.
- While present in the uterus and initially involved in wound repair, **mature scar tissue** predominantly consists of **Type 1 collagen**.
*Type 4 collagen*
- **Type 4 collagen** is a major component of the **basal lamina**, a specialized extracellular matrix that underlies epithelial and endothelial cells.
- It does not form fibrillar structures and is not the primary component of robust scar tissue found in Asherman's syndrome.
*Type 2 collagen*
- **Type 2 collagen** is the main collagen type found in **hyaline cartilage** and elastic cartilage, providing resistance to pressure.
- It is not found in significant amounts in uterine tissue or scar tissue formed within the uterus.
*Elastin*
- **Elastin** is a protein that provides **elasticity** to tissues like blood vessels, skin, and lungs, allowing them to stretch and recoil.
- While present in the uterus for its contractile properties, it is not the primary constituent of **fibrotic scar tissue** forming adhesions.
Phases of wound healing US Medical PG Question 5: A 16-year-old boy presents to the emergency department after a skateboarding accident. He fell on a broken bottle and received a 4 cm wound on the dorsal aspect of his left hand. His vitals are stable and he was evaluated by the surgeon on call who determined that suturing was not required. After several weeks the wound has almost completely healed (see image). Which of the following is the correct description of this patient's wound before healing?
- A. Incised wound (Correct Answer)
- B. Abrasion
- C. Laceration
- D. Avulsion
- E. Puncture
Phases of wound healing Explanation: ***Incised wound***
- An **incised wound** is caused by a sharp object, such as a broken bottle, resulting in a clean, straight cut with well-defined edges and minimal tissue damage.
- The characteristics of the injury (sharp object mechanism, 4 cm linear wound) and the clinical decision that suturing was not required suggest a relatively clean incised wound with edges that could approximate well.
- Incised wounds typically heal with **fine linear scars** as shown in the image, especially when the edges are well-approximated.
*Abrasion*
- An abrasion is a **superficial wound** caused by friction or scraping, leading to removal of the epidermis and sometimes the superficial dermis.
- This mechanism does not match the described injury from a broken bottle, and abrasions produce broad, shallow wounds rather than deep linear cuts.
- Abrasions heal with minimal scarring and would not produce the linear scar pattern shown.
*Laceration*
- A laceration is a wound with **irregular, torn edges** typically caused by blunt force trauma or crushing injury.
- While broken glass can sometimes cause lacerations, the description of a clean "4 cm wound" from falling on a broken bottle more strongly suggests a sharp cutting mechanism rather than tearing.
- Lacerations have jagged edges with more tissue damage and typically require debridement or careful closure.
*Avulsion*
- An **avulsion** involves forcible tearing away of tissue, often resulting in significant tissue loss with irregular, gaping wounds.
- This injury pattern is much more severe than described and would typically require complex surgical management, including possible skin grafting.
- The mechanism (falling on broken glass) and the relatively straightforward healing do not support an avulsion injury.
*Puncture*
- A puncture wound is caused by a **pointed object** penetrating the skin, creating a small entry hole with depth greater than width.
- The description of a "4 cm wound" indicates a linear length, not a deep narrow penetration typical of puncture wounds.
- Puncture wounds carry high infection risk and would not produce the linear scar pattern shown in the image.
Phases of wound healing US Medical PG Question 6: An investigator is studying the structural integrity of collagen. Human fibroblasts are cultured on a medium and different enzymes are applied. One of the cultures is supplemented with an enzyme that inhibits lysyl oxidase, preventing the formation of covalent cross-links between collagen α-chains. Which of the following processes is most likely to be impaired as a result?
- A. Internal elastic lamina formation
- B. Ligament relaxation
- C. Osteoclast activation
- D. Bone matrix synthesis (Correct Answer)
- E. Cartilaginous growth plate mineralization
Phases of wound healing Explanation: ***Bone matrix synthesis***
* **Collagen** is the primary organic component of the bone matrix (osteoid), and its proper cross-linking through **lysyl oxidase-mediated covalent bonds** is crucial for structural integrity and subsequent mineralization.
* **Lysyl oxidase** converts lysine and hydroxylysine residues to aldehydes (allysine and hydroxyallysine), which then form **aldol condensations and Schiff bases** to create stable cross-links between collagen fibrils.
* Inhibiting lysyl oxidase directly compromises the formation of stable collagen fibrils, which are essential for **osteoid production** and bone strength, leading to conditions like **lathyrism** (seen with β-aminopropionitrile exposure).
*Incorrect Option: Internal elastic lamina formation*
* The **internal elastic lamina** is primarily composed of **elastin**, not collagen, and provides arterial elasticity.
* While elastin also requires lysyl oxidase for cross-linking (desmosine and isodesmosine formation), the question specifically asks about **collagen α-chains**, making bone matrix synthesis the more direct answer.
*Incorrect Option: Ligament relaxation*
* **Ligament relaxation** refers to increased laxity, primarily influenced by hormones like relaxin during pregnancy.
* Impairing collagen cross-linking would lead to **ligament weakness and fragility** rather than physiologic relaxation, potentially causing joint instability.
*Incorrect Option: Osteoclast activation*
* **Osteoclast activation** involves bone resorption, regulated by **RANK/RANKL/OPG signaling**, and is independent of newly synthesized collagen cross-linking.
* While collagen integrity affects bone quality, lysyl oxidase inhibition impairs **osteoblast-mediated bone formation**, not osteoclast function.
*Incorrect Option: Cartilaginous growth plate mineralization*
* **Growth plate mineralization** involves calcium phosphate crystal deposition within cartilage matrix, regulated by chondrocytes and factors like alkaline phosphatase.
* While collagen integrity is important in cartilage, the defect in collagen cross-linking most critically affects **bone matrix (osteoid)** synthesis, where type I collagen predominates and provides the scaffold for mineralization.
Phases of wound healing US Medical PG Question 7: A 16-year-old male presents to the emergency department with a hematoma after falling during gym class. He claims that he has a history of prolonged nosebleeds and bruising/bleeding after minor injuries. Physical exam is unrevealing other than the hematoma. Labs are obtained showing an increased bleeding time and an abnormal ristocetin cofactor assay. Coagulation assays reveal an increased partial thromboplastin time (PTT) but a normal prothrombin time (PT). The patient is given desmopressin and is asked to avoid aspirin. Which of the following findings is most likely directly involved in the etiology of this patient's presentation?
- A. Decreased levels or dysfunction of von Willebrand factor (Correct Answer)
- B. Decreased levels of factor IX
- C. Decreased platelet count
- D. Decreased plasma fibrinogen
- E. Decreased activity of ADAMTS13
Phases of wound healing Explanation: ***Decreased levels or dysfunction of von Willebrand factor***
- The patient's presentation with mucosal bleeding (nosebleeds), easy bruising, prolonged **bleeding time**, increased **PTT**, and abnormal **ristocetin cofactor assay** is characteristic of **von Willebrand disease (vWD)**.
- The **direct etiology** is a deficiency or dysfunction of **von Willebrand factor (vWF)**, which serves two critical functions: mediating platelet adhesion to damaged endothelium and stabilizing factor VIII in circulation.
- The abnormal **ristocetin cofactor assay** specifically tests vWF function and is diagnostic for vWD.
- Treatment with **desmopressin (DDAVP)** stimulates release of stored vWF, confirming the diagnosis.
*Decreased levels of factor VIII*
- While factor VIII levels are indeed **secondarily decreased** in vWD due to loss of vWF's stabilizing effect, this is a **consequence** rather than the direct etiologic defect.
- Factor VIII deficiency alone (hemophilia A) would cause prolonged PTT and bleeding, but would not cause prolonged bleeding time or abnormal ristocetin cofactor assay, as these specifically reflect platelet function and vWF activity.
*Decreased levels of factor IX*
- This causes **hemophilia B**, characterized by prolonged **PTT** and bleeding into joints and muscles.
- However, hemophilia B would not cause prolonged **bleeding time** or abnormal **ristocetin cofactor assay**, which indicate platelet dysfunction specific to vWD.
*Decreased platelet count*
- Thrombocytopenia causes prolonged **bleeding time** and mucocutaneous bleeding, but typically does not affect **PTT**.
- The abnormal **ristocetin cofactor assay** indicates a qualitative platelet function defect (inability to aggregate with ristocetin due to absent vWF), not simply low platelet numbers.
*Decreased activity of ADAMTS13*
- This enzyme cleaves ultra-large vWF multimers; its deficiency causes **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP presents with thrombotic microangiopathy, hemolytic anemia, thrombocytopenia, renal failure, and neurological symptoms - not the bleeding diathesis seen here.
- This patient's presentation indicates **insufficient** vWF function, not excessive vWF activity.
Phases of wound healing US Medical PG Question 8: A 45-year-old man comes to his primary care provider for a routine visit. The patient mentions that while he was cooking 5 days ago, he accidentally cut himself with a meat cleaver and lost the skin at the tip of his finger. After applying pressure and ice, the bleeding stopped and he did not seek treatment. The patient is otherwise healthy and does not take any daily medications. The patient’s temperature is 98.2°F (36.8°C), blood pressure is 114/72 mmHg, pulse is 60/min, and respirations are 12/min. On exam, the patient demonstrates a 0.5 x 0.3 cm wound on the tip of his left third finger. No bone is involved, and the wound is red, soft, and painless. There are no signs of infection. Which of the following can be expected on histopathological examination of the wounded area?
- A. Platelet aggregates
- B. Epithelial cell migration from the wound borders
- C. Neutrophil migration into the wound
- D. Deposition of type III collagen (Correct Answer)
- E. Deposition of type I collagen
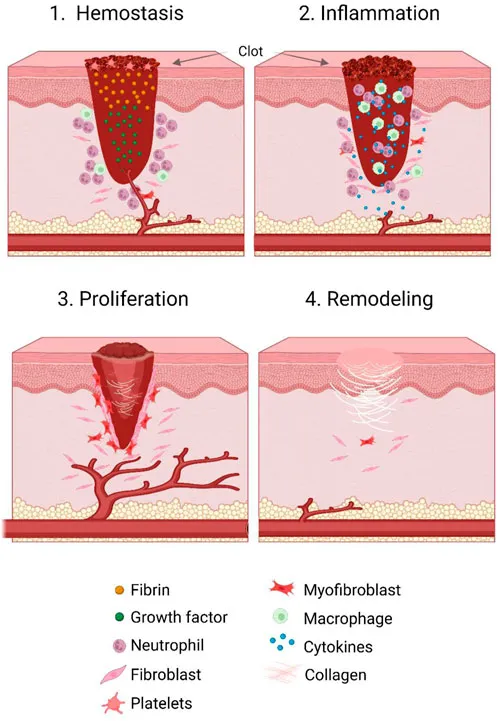
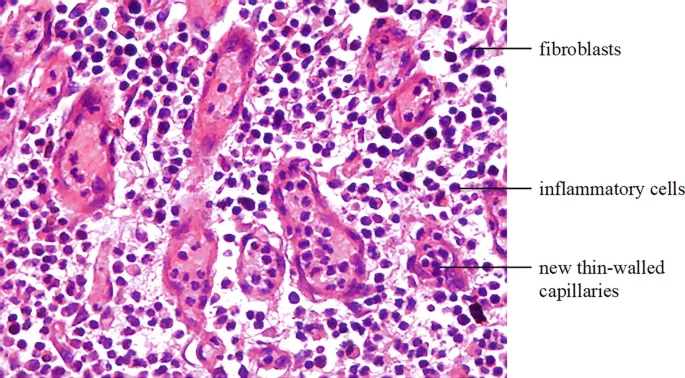
Phases of wound healing Explanation: ***Deposition of type III collagen***
- Five days post-injury, the **proliferative phase of wound healing** is active, characterized by the formation of an initial **granulation tissue** matrix primarily composed of **Type III collagen**.
- This type of collagen forms thinner, more flexible fibers that provide a temporary scaffold for tissue regeneration before being gradually replaced by stronger Type I collagen.
*Platelet aggregates*
- **Platelet aggregation** occurs immediately after injury as part of **hemostasis**, forming a plug to stop bleeding.
- By five days, this initial phase would have concluded, and the primary focus would be on tissue repair and regeneration.
*Epithelial cell migration from the wound borders*
- **Epithelial cell migration** for re-epithelialization typically occurs within the first 24-48 hours after injury, forming a new epidermal layer over the wound.
- While it continues, the dominant histological feature at day 5 in an open wound of this size would be **granulation tissue formation** in the dermis.
*Neutrophil migration into the wound*
- **Neutrophil migration** is a hallmark of the **inflammatory phase**, peaking within 24-48 hours post-injury to clear debris and microbes.
- By day 5, the inflammatory phase would be subsiding, and macrophages would be more prevalent, signaling the transition to the proliferative phase.
*Deposition of type I collagen*
- **Type I collagen** is the predominant collagen found in mature scar tissue and is deposited during the later **remodeling phase** of wound healing.
- While some Type I collagen may be present, **Type III collagen** is characteristic of the early granulation tissue prominent at day 5.
Phases of wound healing US Medical PG Question 9: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Phases of wound healing Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Phases of wound healing US Medical PG Question 10: A previously healthy 5-year-old boy is brought to the emergency department 15 minutes after sustaining an injury to his right hand. His mother says that she was cleaning the bathroom when he accidentally knocked over the drain cleaner bottle and spilled the liquid onto his hand. On arrival, he is crying and holding his right hand in a flexed position. His temperature is 37.7°C (99.8°F), pulse is 105/min, respirations are 25/min, and blood pressure is 105/65 mm Hg. Examination of the right hand shows a 4 x 4 cm area of reddened, blistered skin. The area is very tender to light touch. His ability to flex and extend the right hand are diminished. Radial pulses are palpable. Capillary refill time is less than 3 seconds. Which of the following is the most appropriate next step in management?
- A. Irrigate with water (Correct Answer)
- B. Apply split-thickness skin graft
- C. Apply silver sulfadiazine
- D. Apply mineral oil
- E. Perform escharotomy
Phases of wound healing Explanation: ***Irrigate with water***
- The immediate and most crucial step for a **chemical burn** is copious **irrigation with water** to remove the offending agent and prevent further tissue damage.
- This action minimizes the duration of contact between the **corrosive substance** and the skin, halting the chemical reaction.
*Apply split-thickness skin graft*
- A **skin graft** is a surgical procedure typically reserved for **deep burns** and is not the immediate first step for chemical exposure.
- It would be considered later in management if the burn resulted in **full-thickness tissue loss** and incomplete wound healing.
*Apply silver sulfadiazine*
- **Silver sulfadiazine** is an antimicrobial cream used to prevent infection in **thermal burns** after initial wound care.
- It is not indicated as the first line of treatment for a **chemical burn** and would not remove the chemical agent from the skin.
*Apply mineral oil*
- Applying **mineral oil** is not the appropriate initial treatment for a **chemical burn** and could potentially trap the chemical, worsening the injury.
- The priority is to dilute and remove the chemical, which mineral oil cannot do effectively.
*Perform escharotomy*
- An **escharotomy** is a surgical incision through burn eschar used to relieve pressure in **circumferential full-thickness burns** that compromise circulation.
- This procedure is not indicated as the initial management for a **chemical burn** and is only considered for severe, deep burns with vascular compromise.
More Phases of wound healing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.