Negative pressure wound therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Negative pressure wound therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Negative pressure wound therapy US Medical PG Question 1: Two hours after admission to the intensive care unit, a 56-year-old man with necrotizing pancreatitis develops profound hypotension. His blood pressure is 80/50 mm Hg and he is started on vasopressors. A central venous access line is placed. Which of the following is most likely to decrease the risk of complications from this procedure?
- A. Placement of the central venous line in the femoral vein
- B. Replacement of the central venous line every 7-10 days
- C. Initiation of anticoagulation after placement
- D. Preparation of the skin with chlorhexidine and alcohol (Correct Answer)
- E. Initiation of periprocedural systemic antibiotic prophylaxis
Negative pressure wound therapy Explanation: ***Preparation of the skin with chlorhexidine and alcohol***
- **Chlorhexidine** with alcohol is the most effective skin antiseptic for preventing **catheter-related bloodstream infections (CRBSIs)** by significantly reducing skin microbial counts.
- Proper skin preparation is a cornerstone of preventing **infectious complications** associated with central venous catheter insertion.
*Placement of the central venous line in the femoral vein*
- The femoral site is generally associated with a **higher risk of infection** and **deep venous thrombosis** compared to subclavian or internal jugular sites in adult patients.
- Femoral access is often reserved for situations where other sites are inaccessible or contraindicated, due to its **less favorable complication profile**.
*Replacement of the central venous line every 7-10 days*
- Routine replacement of central venous lines at fixed intervals, without clinical indication, has **not been shown to reduce infection rates**.
- This practice can actually **increase the risk** of mechanical complications and introduce new opportunities for infection with each procedure.
*Initiation of anticoagulation after placement*
- Routine systemic **anticoagulation** after central venous line placement is generally **not recommended** due to an increased risk of **bleeding complications**.
- Anticoagulation is typically reserved for specific indications such as documented **catheter-related thrombosis**.
*Initiation of periprocedural systemic antibiotic prophylaxis*
- Routine **systemic antibiotic prophylaxis** is **not recommended** for central venous catheter insertion as it promotes **antibiotic resistance** without significantly reducing CRBSIs.
- Strict adherence to **aseptic technique** and proper skin antisepsis are more effective for preventing infections.
Negative pressure wound therapy US Medical PG Question 2: A 60-year-old female presents to her primary care physician complaining of bloating and fatigue over the past year. On examination, she has abdominal distension and ascites. Abdominal imaging reveals a mass-like lesion affecting the left ovary. A biopsy of the lesion demonstrates serous cystadenocarcinoma. She is subsequently started on a chemotherapeutic medication known to stabilize polymerized microtubules. Which of the following complications should this patient be monitored for following initiation of this medication?
- A. Peripheral neuropathy (Correct Answer)
- B. Pulmonary fibrosis
- C. Acoustic nerve damage
- D. Hemorrhagic cystitis
- E. Cardiotoxicity
Negative pressure wound therapy Explanation: ***Peripheral neuropathy***
- The chemotherapeutic medication described, which stabilizes **polymerized microtubules**, is likely a **taxane** (e.g., paclitaxel, docetaxel), often used for ovarian cancer.
- Taxanes are well-known to cause **dose-dependent peripheral neuropathy** due to their effects on microtubule dynamics in neuronal axons.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a significant side effect associated with certain chemotherapeutic agents like **bleomycin** or **busulfan**, but not typically with taxanes.
- Monitoring for this would involve assessing breath sounds, oxygen saturation, and potentially imaging for interstitial changes.
*Acoustic nerve damage*
- **Acoustic nerve damage** and ototoxicity are characteristic side effects of **platinum-based chemotherapy agents** (e.g., cisplatin), which are also used in ovarian cancer but have a different mechanism of action than microtubule stabilizers.
- This typically manifests as **tinnitus** or **hearing loss**.
*Hemorrhagic cystitis*
- **Hemorrhagic cystitis** is a common and severe side effect of **cyclophosphamide** and **ifosfamide**, alkylating agents, due to the accumulation of their metabolite **acrolein** in the bladder.
- It is not associated with microtubule-stabilizing agents like taxanes.
*Cardiotoxicity*
- **Cardiotoxicity**, including dilated cardiomyopathy, is a serious side effect primarily associated with **anthracyclines** (e.g., doxorubicin), which generate free radicals and damage cardiac myocytes.
- While some taxanes can cause cardiovascular effects, severe cardiotoxicity like that seen with anthracyclines is not their primary or most concerning side effect.
Negative pressure wound therapy US Medical PG Question 3: A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?
- A. Fibroblasts
- B. Myofibroblasts (Correct Answer)
- C. Neutrophils
- D. Macrophages
- E. Endothelial cells
Negative pressure wound therapy Explanation: ***Myofibroblasts***
- The patient presents with a **contracture** (restricted range of motion and hyperextension of the hand due to a thick scar) after a burn, which is characteristic of the action of **myofibroblasts**.
- Myofibroblasts are specialized cells that possess features of both fibroblasts (synthesizing **collagen** and extracellular matrix) and smooth muscle cells (containing **actin microfilaments**), allowing them to exert contractile force which leads to scar contraction.
*Fibroblasts*
- While fibroblasts are crucial for **wound healing** by producing collagen and other extracellular matrix components, they primarily lay down the foundation for scar tissue.
- They lack the strong contractile capabilities that lead to significant **tissue retraction** and contracture.
*Neutrophils*
- Neutrophils are **acute inflammatory cells** that primarily function in the early stages of wound healing to phagocytose debris and pathogens.
- They do not play a direct role in the formation of **scar tissue** or **contractures**.
*Macrophages*
- Macrophages are important **immune cells** involved in clearing debris, presenting antigens, and releasing growth factors during the later stages of wound healing.
- They also influence fibroblast activity, but they do not directly cause **tissue contraction** or scar formation.
*Endothelial cells*
- Endothelial cells line **blood vessels** and are essential for **angiogenesis** (formation of new blood vessels) during wound healing.
- They are not involved in the **contractile process** that leads to scar contracture.
Negative pressure wound therapy US Medical PG Question 4: A 52-year-old farmer presents to his physician with a puncture wound on his left shin. He got this wound accidentally when he felt unwell and went out to his garden "to catch some air". He reports he had been treated for tetanus 35 years ago and has received the Tdap vaccine several times since then, but he does not remember when he last received the vaccine. His vital signs are as follows: the blood pressure is 110/80 mm Hg, heart rate is 91/min, respiratory rate is 19/min, and temperature is 37.8°C (100.0°F). On physical examination, he is mildly dyspneic and pale. Lung auscultation reveals diminished vesicular breath sounds in the lower lobes bilaterally with a few inspiratory crackles heard over the left lower lobe. There is a puncture wound 1 cm in diameter that is contaminated with soil in the middle third of the patient’s shin. You order blood tests and an X-ray, and now you are arranging his wound treatment. How should tetanus post-exposure prevention be performed in this case?
- A. The patient should be administered only the Tdap vaccine, because it is a minor wound with a small area of possible toxin absorption.
- B. The patient does not need tetanus post-exposure prevention, because he has a past medical history of tetanus.
- C. The patient should receive both tetanus toxoid-containing vaccine and human tetanus immunoglobulin. (Correct Answer)
- D. The patient does not need tetanus post-exposure prevention, because he received the Tdap vaccine several times in the past.
- E. The patient should only be administered human tetanus immunoglobulin, because he is acutely ill and febrile, which are contraindications for tetanus toxoid-containing vaccine administration.
Negative pressure wound therapy Explanation: ***The patient should receive both tetanus toxoid-containing vaccine and human tetanus immunoglobulin.***
- This patient has a **tetanus-prone wound** (puncture wound contaminated with soil) and an **uncertain vaccination history** (due to not remembering when the last Tdap was).
- For clean wounds, a Tdap booster within 5 years is sufficient, but with a dirty wound and uncertain history, **both passive immunization (tetanus immunoglobulin) and active immunization (Tdap vaccine)** are required.
*The patient should be administered only the Tdap vaccine, because it is a minor wound with a small area of possible toxin absorption.*
- A **puncture wound contaminated with soil** is considered a tetanus-prone wound, regardless of size, requiring more aggressive prophylaxis.
- Relying solely on the vaccine may not provide immediate protection, as it takes time for the body to mount an **immune response**.
*The patient does not need tetanus post-exposure prevention, because he has a past medical history of tetanus.*
- A past history of tetanus **does not confer lifelong immunity** due to the low toxin dose required to cause disease, which is insufficient to stimulate a robust immune response.
- Thus, previous tetanus infection does not negate the need for **vaccination or passive immunity** following injury.
*The patient does not need tetanus post-exposure prevention, because he received the Tdap vaccine several times in the past.*
- While he received the vaccine "several times," the **exact timing of his last dose is unknown**, which is critical for determining protection levels.
- Without a clear history of a booster within the last **5 years for dirty wounds** or 10 years for clean wounds, his immune status is considered uncertain.
*The patient should only be administered human tetanus immunoglobulin, because he is acutely ill and febrile, which are contraindications for tetanus toxoid-containing vaccine administration.*
- **Mild illness or low-grade fever** is generally not a contraindication for vaccination, and the potential benefits often outweigh the risks in post-exposure prophylaxis.
- While **tetanus immunoglobulin** provides immediate passive protection, it does not stimulate long-term active immunity, which is crucial for ongoing protection.
Negative pressure wound therapy US Medical PG Question 5: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
Negative pressure wound therapy Explanation: ***Surgical debridement***
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
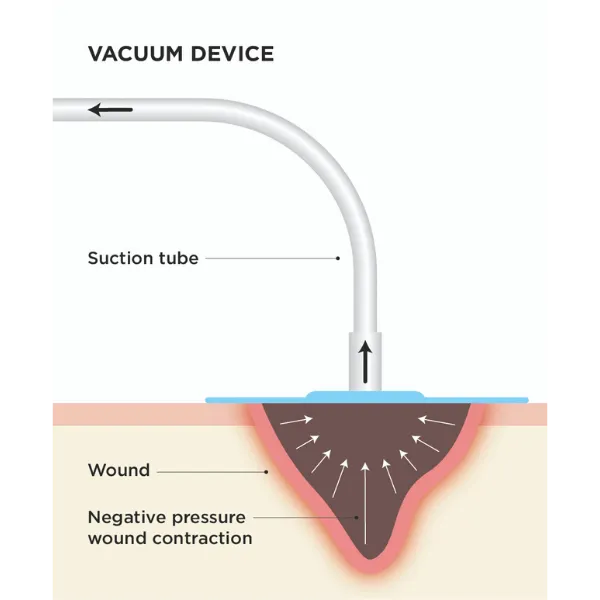
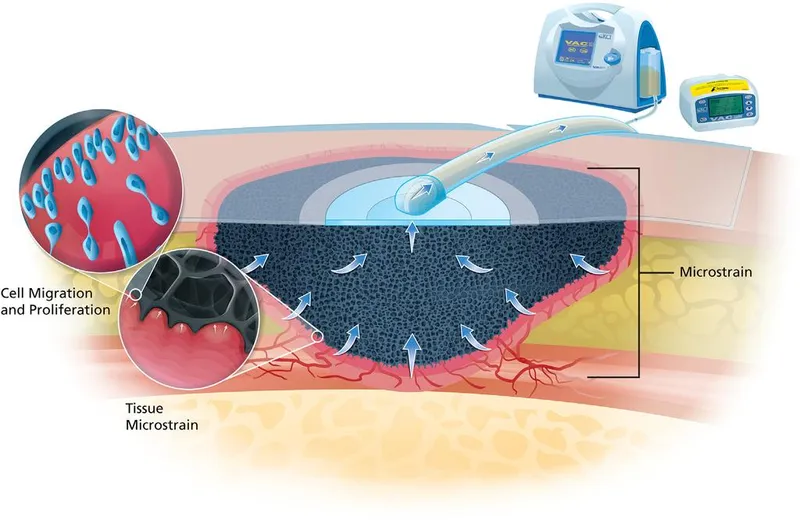
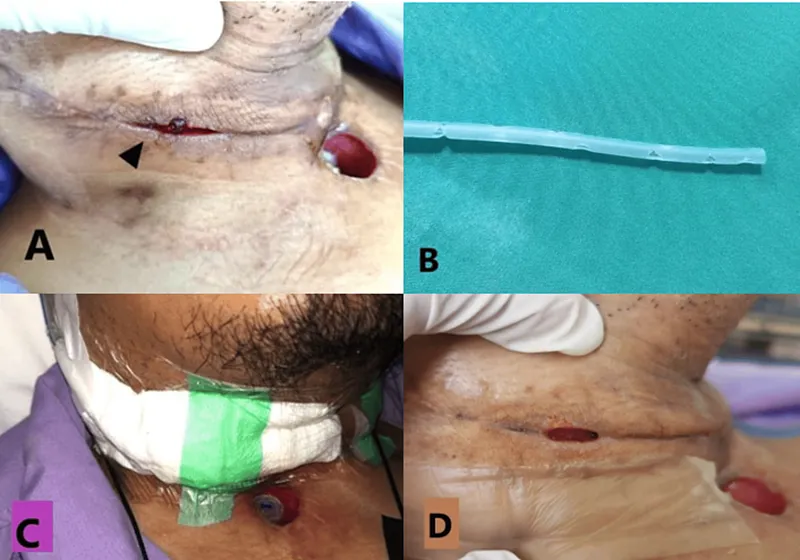
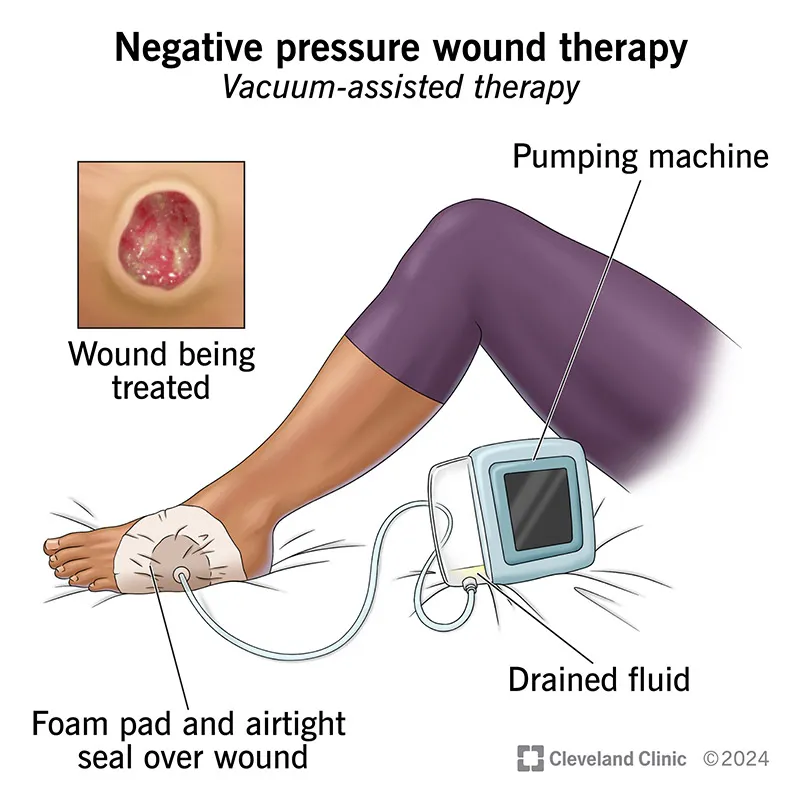
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
Negative pressure wound therapy US Medical PG Question 6: A 15-year-old boy is brought to the emergency department by ambulance after his mother found him having muscle spasms and stiffness in his room. His mother stated he scraped his foot on a rusty razor on the bathroom floor 2 days prior. On presentation, his temperature is 102.0°F (38.9°C), blood pressure is 108/73 mmHg, pulse is 122/min, and respirations are 18/min. On physical exam, he is found to have severe muscle spasms and rigid abdominal muscles. In addition, he has a dirty appearing wound on his right foot. The patient's mother does not recall any further vaccinations since age 12. Finally, he is found to have difficulty opening his mouth so he is intubated. Which of the following treatment(s) should be provided to this patient?
- A. Wound debridement and antitoxin
- B. Antitoxin
- C. Wound debridement
- D. Wound debridement and booster vaccine
- E. Wound debridement, antitoxin, and booster vaccine (Correct Answer)
Negative pressure wound therapy Explanation: ***Wound debridement, antitoxin, and booster vaccine***
- The patient presents with classic symptoms of **tetanus** (muscle spasms, stiffness, trismus, fever) following a contaminated wound, and an uncertain vaccination history.
- **Wound debridement** removes the source of toxin production, **antitoxin** (tetanus immune globulin) neutralizes circulating toxin, and a **booster vaccine** provides active immunity against future infections.
*Wound debridement and antitoxin*
- While **wound debridement** and **antitoxin** are critical for acute management, omitting the booster vaccine leaves the patient vulnerable to future tetanus infections.
- A booster dose is essential to stimulate the patient's own immune system and provide **long-term immunity**, especially with a history of unknown vaccination status.
*Antitoxin*
- Administering only **antitoxin** would neutralize circulating toxins but would not address the ongoing production of toxins from the contaminated wound.
- It also wouldn't provide **active immunization** to protect against future exposures.
*Wound debridement*
- **Wound debridement** alone removes the bacterial source but does not neutralize the already circulating **tetanus toxin**, which is responsible for the severe neurological symptoms.
- It also fails to provide immediate passive immunity with antitoxin or active immunization with a booster.
*Wound debridement and booster vaccine*
- This option correctly addresses removing the source and providing active immunity but critically misses the immediate need for **antitoxin** to neutralize existing toxins and alleviate the life-threatening symptoms.
- The **tetanus toxin** acts rapidly, and prompt neutralization is crucial to prevent further neurological damage and improve prognosis.
Negative pressure wound therapy US Medical PG Question 7: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Negative pressure wound therapy Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Negative pressure wound therapy US Medical PG Question 8: A 39-year-old man comes to the physician for a follow-up examination. He was treated for a urinary tract infection with trimethoprim-sulfamethoxazole 2 months ago. He is paraplegic as a result of a burst lumbar fracture that occurred after a fall 5 years ago. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He performs clean intermittent catheterization daily. He has smoked one pack of cigarettes daily for 19 years. His temperature is 37.1°C (98.8°F), pulse is 95/min, respirations are 14/min, and blood pressure is 120/80 mm Hg. He appears malnourished. Examination shows palpable pedal pulse. Multiple dilated tortuous veins are present over both lower extremities. There is a 2-cm wound surrounded by partial-thickness loss of skin and a pink wound bed over the right calcaneum. Neurologic examination shows paraparesis. His hemoglobin A1c is 6.5%, and fingerstick blood glucose concentration is 134 mg/dL. Which of the following is most likely to have prevented this patient's wound?
- A. Broad-spectrum antibiotic therapy
- B. Cessation of smoking
- C. Heparin therapy
- D. Topical antibiotic therapy
- E. Frequent position changes (Correct Answer)
Negative pressure wound therapy Explanation: ***Frequent position changes***
- This patient is paraplegic, which increases his risk for **pressure ulcers** due to prolonged immobility and sustained pressure on bony prominences like the calcaneum.
- **Frequent repositioning** redistributes pressure, preventing skin breakdown and promoting circulation, thereby avoiding pressure injuries.
*Broad-spectrum antibiotic therapy*
- The wound is described as a **partial-thickness loss** with a pink wound bed, suggesting it's not primarily an infected wound requiring broad-spectrum antibiotics to prevent its formation.
- Antibiotics are used to **treat existing infections**, not prevent pressure ulcers in a non-infected state.
*Cessation of smoking*
- While **smoking impairs wound healing** and overall vascular health, it is not the most direct or primary preventative measure for a pressure ulcer caused by immobility.
- Smoking cessation would improve **long-term vascular health** and *ulcer healing*, but frequent position changes addresses the immediate cause of pressure.
*Heparin therapy*
- **Heparin** is an anticoagulant used to prevent **thrombosis** (blood clots), which is not the primary mechanism behind pressure ulcer formation.
- While immobility can contribute to deep vein thrombosis, heparin would not prevent the **mechanical pressure-induced skin damage** that causes a calcaneal wound.
*Topical antibiotic therapy*
- Similar to systemic antibiotics, topical antibiotics are used for **treating localized infections** or preventing them in *open wounds*.
- This wound is a result of pressure, and preventing its formation requires addressing the pressure itself, not merely applying antibiotics to the skin surface.
Negative pressure wound therapy US Medical PG Question 9: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
Negative pressure wound therapy Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Negative pressure wound therapy US Medical PG Question 10: A 37-year-old man presents to the emergency department after he cut his hand while working on his car. The patient has a past medical history of antisocial personality disorder and has been incarcerated multiple times. His vitals are within normal limits. Physical exam is notable for a man covered in tattoos with many bruises over his face and torso. Inspection of the patient's right hand reveals 2 deep lacerations on the dorsal aspects of the second and third metacarpophalangeal (MCP) joints. The patient is given a tetanus vaccination, and the wound is irrigated. Which of the following is appropriate management for this patient?
- A. Closure of the wound with sutures
- B. Clindamycin and topical erythromycin
- C. Ciprofloxacin and topical erythromycin
- D. Surgical irrigation, debridement, and amoxicillin-clavulanic acid (Correct Answer)
- E. No further management necessary
Negative pressure wound therapy Explanation: ***Surgical irrigation, debridement, and amoxicillin-clavulanic acid***
- The presence of deep lacerations over the metacarpophalangeal joints, combined with an injury mechanism suggestive of a **fight bite** (laceration from striking another person's teeth), mandates **aggressive surgical management**.
- **Amoxicillin-clavulanic acid** is the appropriate antibiotic choice for **human bite wounds** due to its broad spectrum covering common oral flora like *Eikenella corrodens*, *Streptococci*, and anaerobes.
*Closure of the wound with sutures*
- **Primary closure** of human bite wounds, especially those on the hand, is strongly **contraindicated** due to the high risk of severe infection.
- These wounds should be left open to drain and heal by **secondary intention** following thorough debridement.
*Clindamycin and topical erythromycin*
- **Clindamycin** has good anaerobic coverage but lacks sufficient coverage for common aerobes found in human bites like *Eikenella corrodens*.
- **Topical erythromycin** is ineffective for deep soft tissue infections and does not provide systemic protection against the likely pathogens.
*Ciprofloxacin and topical erythromycin*
- **Ciprofloxacin** has limited activity against many oral anaerobes and *Eikenella corrodens*, making it a poor choice for human bite prophylaxis.
- As mentioned, **topical antibiotics** are insufficient for preventing serious infections in deep bite wounds.
*No further management necessary*
- This patient has sustained a **deep, contaminated wound** with a high risk of serious infection, potentially involving joints or tendons.
- Failing to provide further management, including surgical exploration and appropriate antibiotics, would likely lead to severe complications such as **osteomyelitis** or **septic arthritis**.
More Negative pressure wound therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.