Hyperbaric oxygen therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperbaric oxygen therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperbaric oxygen therapy US Medical PG Question 1: A 33-year-old woman is brought to the emergency department 30 minutes after being rescued from a fire in her apartment. She reports nausea, headache, and dizziness. Physical examination shows black discoloration of her oral mucosa. Pulse oximetry shows an oxygen saturation of 99% on room air. The substance most likely causing symptoms in this patient primarily produces toxicity by which of the following mechanisms?
- A. Inhibition of mitochondrial complex V
- B. Degradation of 2,3-bisphosphoglycerate
- C. Oxidation of Fe2+
- D. Rise in serum pH
- E. Competitive binding to heme (Correct Answer)
Hyperbaric oxygen therapy Explanation: ***Competitive binding to heme***
- The patient's symptoms (nausea, headache, dizziness, black oral mucosa) and history of being rescued from a fire strongly suggest **carbon monoxide (CO) poisoning** [1].
- **Carbon monoxide** primarily exerts its toxicity by competitively binding to the **heme iron** in hemoglobin with an affinity 200-250 times greater than oxygen, forming **carboxyhemoglobin (COHb)** and displacing oxygen [2].
*Inhibition of mitochondrial complex V*
- **Cyanide poisoning** inhibits **mitochondrial complex IV (cytochrome c oxidase)**, not complex V, leading to impaired cellular respiration.
- While both cyanide and CO poisoning can occur in fires, CO is more common due to incomplete combustion, and the specific presentation points toward CO.
*Degradation of 2,3-bisphosphoglycerate*
- **2,3-BPG** is an important regulator of oxygen affinity for hemoglobin, promoting oxygen release to tissues [2]. Its degradation would increase hemoglobin's affinity for oxygen, thus reducing oxygen unloading, but this is not the primary mechanism of toxicity for CO or common fire-related toxins.
- No common toxin directly causes widespread degradation of 2,3-BPG as its primary mechanism of acute toxicity or symptoms.
*Oxidation of Fe2+*
- The oxidation of **ferrous iron (Fe2+)** to **ferric iron (Fe3+)** in hemoglobin leads to the formation of **methemoglobin**, which cannot bind oxygen. This occurs in **methemoglobinemia** induced by certain drugs or toxins (e.g., nitrites, dapsone).
- While **methemoglobinemia** impairs oxygen transport, it does not explain the black oral mucosa or the strong association with fire smoke toxicity in the context of CO.
*Rise in serum pH*
- A rise in serum pH (alkalosis) is not a direct or primary mechanism of toxicity for common fire-related toxins like carbon monoxide or cyanide.
- Most severe forms of toxicity, including CO and cyanide poisoning, tend to cause **lactic acidosis** due to cellular hypoxia and anaerobic metabolism, leading to a
**decrease** in serum pH.
Hyperbaric oxygen therapy US Medical PG Question 2: A 25-year-old male athlete undergoes a cardiopulmonary exercise test. As exercise intensity increases from rest to moderate levels, which of the following best describes the relationship between oxygen consumption and cardiac output?
- A. Linear increase until anaerobic threshold (Correct Answer)
- B. Exponential increase throughout exercise
- C. Plateau at low exercise intensities
- D. No change until anaerobic threshold
Hyperbaric oxygen therapy Explanation: ***Linear increase until anaerobic threshold***
- During incremental exercise, both **oxygen consumption (VO2)** and **cardiac output (CO)** increase proportionally with work rate.
- This **linear relationship** continues until the body reaches the **anaerobic threshold**, beyond which other physiological responses begin to dominate.
*Exponential increase throughout exercise*
- An **exponential increase** would imply a disproportionately rapid rise in oxygen consumption and cardiac output even at low-to-moderate exercise intensities, which is not physiologically accurate.
- While both parameters do increase, the initial increase is typically linear, reflecting the immediate physiological demands.
*Plateau at low exercise intensities*
- A **plateau** would suggest that the body's demand for oxygen and the heart's pumping capacity stabilize despite an increase in exercise intensity, which contradicts the need for increased energy supply during exercise.
- The cardiovascular system actively responds to even low-intensity exercise to meet metabolic demands.
*No change until anaerobic threshold*
- **No change** would mean that the cardiovascular system is not responding to the increased metabolic demands of exercise, which is incorrect.
- Both VO2 and CO begin to rise almost immediately upon starting exercise to meet the muscles' increasing oxygen requirements.
Hyperbaric oxygen therapy US Medical PG Question 3: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Hyperbaric oxygen therapy Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
Hyperbaric oxygen therapy US Medical PG Question 4: A 23-year-old woman is brought to the emergency department 30 minutes after stepping on a piece of broken glass. Physical examination shows a 3-cm, ragged laceration on the plantar aspect of the left foot. The physician uses hydrogen peroxide to clean the wound. Which of the following is the most likely mechanism of action of this disinfectant?
- A. Formation of free radicals (Correct Answer)
- B. Intercalation of DNA
- C. Crosslinking of proteins
- D. Halogenation of nucleic acids
- E. Congealing of cytoplasm
Hyperbaric oxygen therapy Explanation: ***Formation of free radicals***
- **Hydrogen peroxide** acts as an **oxidizing agent**, generating highly reactive **oxygen-free radicals** (e.g., superoxide, hydroxyl radicals) that damage microbial cellular components.
- This **oxidative damage** disrupts proteins, lipids, and nucleic acids, leading to bacterial and viral cell death.
*Intercalation of DNA*
- This mechanism is characteristic of certain **chemotherapeutic agents** (e.g., doxorubicin, ethidium bromide) and some **antimicrobials**, which insert themselves between DNA base pairs, disrupting replication and transcription.
- Hydrogen peroxide does not typically target DNA in this manner for its disinfectant action.
*Crosslinking of proteins*
- This mechanism is characteristic of **aldehydes** like **formaldehyde** and **glutaraldehyde**, which form covalent bonds between amino groups of proteins, denaturing them and disrupting cellular function.
- While hydrogen peroxide can modify proteins, its primary disinfectant action is not through widespread protein crosslinking.
*Halogenation of nucleic acids*
- This mechanism is primarily associated with **halogens** such as **chlorine** and **iodine**, which react with nucleic acids to form halogenated compounds, thereby inactivating them.
- Hydrogen peroxide, while an oxidizer, does not lead to halogenation as its primary mode of action.
*Congealing of cytoplasm*
- This mechanism, which refers to the coagulation or solidification of cellular contents, is typical of **alcohols** (e.g., ethanol, isopropanol) and some **heavy metal salts** that denature proteins and lipids, leading to cell lysis.
- Hydrogen peroxide's action is more specific to oxidative damage rather than general cytoplasmic congealing.
Hyperbaric oxygen therapy US Medical PG Question 5: A 9-year-old boy presents for incision and drainage of a small abscess on his left thigh. No significant past medical history. No current medications. Before the procedure, the patient is allowed to inhale colorless, sweet-smelling gas. After the procedure, the patient receives 3–4 minutes of high flow oxygen through a nasal mask. The pulse oximetry shows an oxygen saturation of 94%. This patient was oxygenated at the end of the procedure to prevent which of the following complications?
- A. Malignant hyperthermia
- B. Hepatotoxicity
- C. Raised intracranial pressure
- D. Cardiac arrhythmias
- E. Diffusion hypoxia (Correct Answer)
Hyperbaric oxygen therapy Explanation: ***Diffusion hypoxia (Correct)***
- **Nitrous oxide** rapidly diffuses from the blood into the alveoli after discontinuation, displacing oxygen and carbon dioxide.
- This creates the **"Fink effect"** - a dilution of alveolar oxygen that can lead to transient **hypoxemia**.
- Administering **high-flow oxygen for 3-5 minutes** prevents this complication by maintaining adequate alveolar oxygen concentration during the N2O washout period.
*Malignant hyperthermia (Incorrect)*
- This is a pharmacogenetic disorder triggered by **volatile anesthetics** (e.g., halothane, sevoflurane) and **succinylcholine**, not nitrous oxide.
- Characterized by **muscle rigidity, hyperthermia, and hypermetabolism**.
- While oxygen is part of supportive treatment, post-procedure oxygenation doesn't prevent its onset.
- Treatment requires **dantrolene**, not just oxygen.
*Hepatotoxicity (Incorrect)*
- Not prevented by post-procedure oxygenation.
- Typically associated with **halothane** (rare with modern anesthetics), not nitrous oxide.
- Nitrous oxide is not a primary cause of hepatotoxicity.
*Raised intracranial pressure (Incorrect)*
- While nitrous oxide can increase **cerebral blood flow** and potentially raise ICP, post-procedure oxygen doesn't specifically prevent this effect.
- Management of elevated ICP involves **hyperventilation, head elevation, osmotic diuretics**, and avoiding N2O in at-risk patients.
- The oxygen administration here targets diffusion hypoxia, not ICP control.
*Cardiac arrhythmias (Incorrect)*
- While hypoxia can cause arrhythmias, the primary purpose of post-N2O oxygen is to prevent **diffusion hypoxia**.
- Preventing hypoxemia secondarily reduces arrhythmia risk, but this is not the direct indication.
- Arrhythmias from anesthetics are more commonly associated with **halogenated agents** sensitizing the myocardium to catecholamines.
Hyperbaric oxygen therapy US Medical PG Question 6: A neonate suffering from neonatal respiratory distress syndrome is given supplemental oxygen. Which of the following is a possible consequence of oxygen therapy in this patient?
- A. Anosmia
- B. Atelectasis
- C. Atopy
- D. Blindness (Correct Answer)
- E. Cardiac anomalies
Hyperbaric oxygen therapy Explanation: ***Blindness***
- High concentrations of supplemental oxygen in neonates, particularly premature infants, can lead to **retinopathy of prematurity (ROP)**.
- ROP involves abnormal growth of blood vessels in the retina, which can detach the retina and result in **permanent blindness**.
*Anosmia*
- **Anosmia** is the loss of the sense of smell, typically caused by nasal polyps, head trauma, or certain viral infections.
- It is **not a recognized complication** of oxygen therapy in neonates.
*Atelectasis*
- **Atelectasis** refers to the collapse of lung tissue, which can be caused by bronchial obstruction or hypoventilation.
- While underlying respiratory distress syndrome can predispose to atelectasis, oxygen therapy itself typically aims to improve ventilation and **does not directly cause atelectasis**.
*Atopy*
- **Atopy** is a genetic predisposition to developing allergic diseases such as asthma, eczema, and allergic rhinitis.
- It is **unrelated to oxygen therapy** and is determined by genetic factors and environmental exposures.
*Cardiac anomalies*
- **Cardiac anomalies** (congenital heart defects) are structural problems in the heart present at birth, resulting from abnormal fetal development.
- They are **not a consequence of oxygen therapy** given postpartum; oxygen therapy may be used to manage their symptoms.
Hyperbaric oxygen therapy US Medical PG Question 7: A 36-year-old male with fluctuating levels of consciousness is brought to the emergency department by ambulance due to a fire in his home. He currently opens his eyes to voice, localizes painful stimuli, responds when asked questions, but is disoriented and cannot obey commands. The patient’s temperature is 99°F (37.2°C), blood pressure is 86/52 mmHg, pulse is 88/min, and respirations are 14/min with an oxygen saturation of 97% O2 on room air. Physical exam shows evidence of soot around the patient’s nose and mouth, but no burns, airway obstruction, nor accessory muscle use. A blood lactate is 14 mmol/L. The patient is started on intravenous fluids.
What is the next best step in management?
- A. Methylene blue
- B. Hyperbaric oxygen
- C. Sodium thiosulfate and sodium nitrite
- D. Intravenous epinephrine
- E. 100% oxygen, hydroxycobalamin, and sodium thiosulfate (Correct Answer)
Hyperbaric oxygen therapy Explanation: ***100% oxygen, hydroxycobalamin, and sodium thiosulfate***
- This patient presents with signs of both **carbon monoxide poisoning** (fire exposure, disoriented, altered mental status) and **cyanide poisoning** (fire exposure, very high lactate, normal oxygen saturation despite altered mental status). This combination therapy directly addresses both.
- **100% oxygen** competes with carbon monoxide for hemoglobin binding and helps clear it, while **hydroxycobalamin** and **sodium thiosulfate** are antidotes for cyanide poisoning, converting cyanide into less toxic compounds.
*Methylene blue*
- **Methylene blue** is used to treat **methemoglobinemia**, a condition where iron in hemoglobin is oxidized, leading to impaired oxygen transport.
- The patient's symptoms (fire exposure, altered mental status, and a high lactate with normal SpO2) are not characteristic of methemoglobinemia, but rather strong indicators of carbon monoxide and cyanide poisoning.
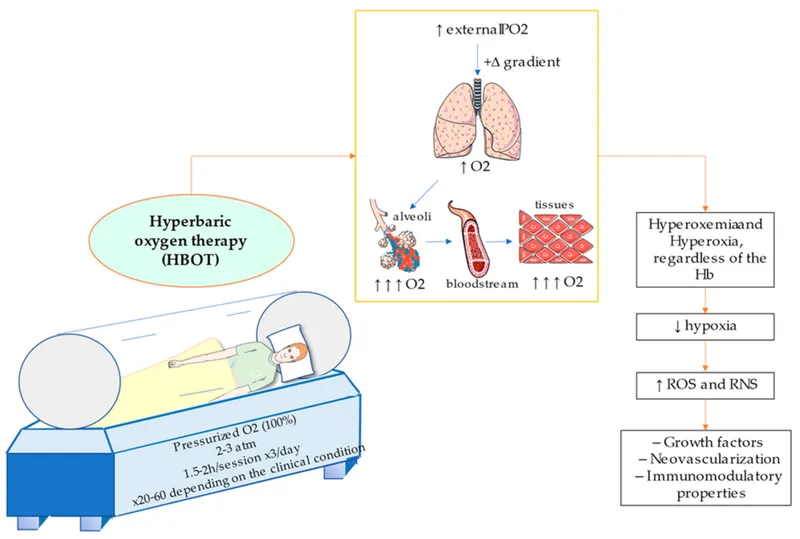
*Hyperbaric oxygen*
- **Hyperbaric oxygen** is a treatment for severe carbon monoxide poisoning, but it is not the initial or sole treatment for a patient with suspected co-existing cyanide poisoning.
- While recommended for **severe CO poisoning**, it doesn't directly address cyanide toxicity, which is suggested by the metabolic acidosis with a high lactate level despite normal oxygen saturation.
*Sodium thiosulfate and sodium nitrite*
- This combination (the **Lilly kit**) is traditionally used to treat **cyanide poisoning**, with sodium nitrite inducing methemoglobinemia to sequester cyanide, and sodium thiosulfate aiding its excretion.
- The patient also requires treatment for **carbon monoxide poisoning**, and hydroxycobalamin is generally preferred over sodium nitrite as it does not induce methemoglobinemia, which can worsen hypoxia in CO poisoning.
*Intravenous epinephrine*
- **Epinephrine** is a powerful vasoconstrictor and bronchodilator primarily used to treat **anaphylaxis** or **cardiac arrest**.
- There is no indication of anaphylaxis or cardiac arrest in this patient, and epinephrine would not be an appropriate treatment for carbon monoxide or cyanide poisoning.
Hyperbaric oxygen therapy US Medical PG Question 8: A 69-year-old man presents to the emergency department with shortness of breath that has been worsening over the past month. The patient states that he has had worsening shortness of breath that has progressed to shortness of breath with simple activities and minor exertion. When he was unable to climb the stairs to his house today, he decided to come to the emergency department. The patient has a past medical history of poorly managed diabetes mellitus, hypertension, end stage renal disease, and obesity. His current medications include insulin, metformin, lisinopril, hydrochlorothiazide, and ibuprofen. The patient is notably non-compliant with his medications. An EKG and chest radiograph are normal. The patient had dialysis two days ago and attends most of his appointments. Laboratory values are ordered and are seen below:
Serum:
Na+: 135 mEq/L
K+: 4.5 mEq/L
Cl-: 100 mEq/L
HCO3-: 19 mEq/L
Urea nitrogen: 29 mg/dL
Glucose: 75 mg/dL
Creatinine: 2.5 mg/dL
Ca2+: 9.2 mg/dL
Mg2+: 1.7 mEq/L
AST: 11 U/L
ALT: 11 U/L
Leukocyte count and differential:
Leukocyte count: 4,500/mm^3
Platelet count: 150,000/mm^3
Neutrophil: 54%
Lymphocyte: 25%
Monocyte: 3%
Eosinophil: 1%
Basophil: 1%
Hemoglobin: 8.2 g/dL
Hematocrit: 22%
Mean corpuscular volume: 82 µm^3
The patient appears comfortable at rest but demonstrates notable shortness of breath when exerting himself. His temperature is 99.5°F (37.5°C), pulse is 89/min, blood pressure is 144/85 mmHg, respirations are 10/min, and oxygen saturation is 97% on room air. Pulmonary and cardiac exam are within normal limits. Which of the following is a side-effect of the long-term therapy this patient should be started on right now?
- A. Hyperkalemia
- B. Pruritus
- C. Hypertension (Correct Answer)
- D. Hypokalemia
- E. Visual halos
Hyperbaric oxygen therapy Explanation: ***Hypertension***
- This patient is experiencing symptomatic **anemia of chronic kidney disease** (Hgb 8.2 g/dL, Hct 22%) and should be started on **erythropoiesis-stimulating agents (ESA)** such as erythropoietin or darbepoetin.
- **Hypertension is the most common side effect** of erythropoietin therapy, occurring in **20-30% of patients**. The mechanism involves increased blood viscosity from rising hematocrit, increased peripheral vascular resistance, and direct vasoconstrictive effects.
- Patients on ESA therapy require **close blood pressure monitoring** and may need adjustment of antihypertensive medications. Blood pressure should be controlled before initiating ESA therapy.
- Other important side effects include thrombotic events, headache, and flu-like symptoms.
*Visual halos*
- Visual halos are a classic symptom of **digoxin toxicity**, not a side effect of erythropoietin therapy.
- While this patient has multiple cardiac risk factors, the primary issue is **anemia requiring ESA therapy**, not heart failure requiring digoxin.
*Hyperkalemia*
- Hyperkalemia is associated with **renal failure**, **ACE inhibitors** (lisinopril), or **potassium-sparing diuretics**, but the patient's current potassium is normal (4.5 mEq/L).
- Hyperkalemia is **not a recognized side effect** of erythropoietin therapy.
*Pruritus*
- Pruritus can be a symptom of **chronic kidney disease** or **uremia** itself, but it is not a direct side effect of **erythropoietin therapy**.
- While ESRD patients commonly experience pruritus, this is not related to ESA treatment.
*Hypokalemia*
- Hypokalemia is **not a recognized side effect** of erythropoietin therapy.
- While ESA stimulates red blood cell production in bone marrow, this does not cause clinically significant potassium shifts or hypokalemia.
- The patient's current potassium level is normal at 4.5 mEq/L.
Hyperbaric oxygen therapy US Medical PG Question 9: A 14-year-old boy is brought to the emergency department by his mom after she found him complaining of headaches, nausea, lightheadedness, and muscle pain. He has had type I diabetes for 3 years with very well managed blood sugars, and he is otherwise healthy. He recently returned from a boy scout skiing trip where he drank from a mountain stream, ate unusual foods, and lived in a lodge with a wood-fired fireplace and cooking stove. On physical exam he has a diffuse redness of his skin. Which of the following changes to this patient's pulmonary system would cause oxygen to exhibit similar tissue hypoxia effects as the most likely cause of this patient's symptoms?
- A. Increasing capillary length
- B. Nitrous oxide administration
- C. Increasing capillary transit time
- D. Interstitial thinning
- E. Interstitial fibrosis (Correct Answer)
Hyperbaric oxygen therapy Explanation: ***Interstitial fibrosis***
- Carbon monoxide poisoning causes tissue hypoxia by reducing **oxygen-carrying capacity** (CO binds hemoglobin with high affinity, maintaining normal PaO2 but severely reducing oxygen content and delivery to tissues).
- Among the pulmonary changes listed, interstitial fibrosis most closely produces **tissue hypoxia** by impairing oxygen transfer across the thickened alveolar-capillary membrane, resulting in **hypoxemia and reduced tissue oxygen delivery**.
- While the mechanisms differ (CO affects carrying capacity vs. fibrosis affects diffusion), both ultimately result in inadequate oxygen delivery to meet tissue metabolic demands, manifesting as tissue hypoxia.
- Interstitial fibrosis creates a **diffusion barrier** that worsens with increased oxygen demand (exercise), similar to how CO poisoning impairs the ability to meet tissue oxygen requirements.
*Increasing capillary length*
- Increasing capillary length would **improve gas exchange** by providing more surface area and time for oxygen diffusion across the alveolar-capillary membrane.
- This adaptation enhances oxygen delivery to tissues, which is the opposite of the tissue hypoxia seen in CO poisoning.
*Nitrous oxide administration*
- Nitrous oxide is an anesthetic gas that acts primarily on the **central nervous system** and does not significantly impair oxygen transport or binding to hemoglobin.
- While it can displace oxygen at very high concentrations, its mechanism does not mimic the impaired oxygen delivery characteristic of CO poisoning.
*Increasing capillary transit time*
- Increased capillary transit time allows **more time for oxygen equilibration** between alveolar gas and capillary blood, thereby improving oxygenation.
- This would enhance tissue oxygen delivery rather than cause tissue hypoxia, opposite to the effect of CO poisoning.
*Interstitial thinning*
- Interstitial thinning **decreases the diffusion distance** for oxygen, facilitating more efficient gas exchange across the alveolar-capillary membrane.
- This would improve oxygen delivery to tissues and is the opposite of what occurs in CO poisoning.
Hyperbaric oxygen therapy US Medical PG Question 10: A 25-year-old woman is rushed to the emergency department after she was found unconscious in a house fire. She has no previous medical history available. At the hospital, the vital signs include: blood pressure 110/70 mm Hg, temperature 36.0°C (97.0°F), and heart rate 76/min with oxygen saturation 99% on room air. On physical exam she is unconscious. There are superficial burns on her hands and parts of her face. Her face and clothes are blackened with soot. What is the 1st best step while treating this patient?
- A. Sodium nitrite
- B. Administer 100% oxygen (Correct Answer)
- C. Penicillamine
- D. Pyridoxine (vitamin B6)
- E. N-acetylcysteine
Hyperbaric oxygen therapy Explanation: ***Administer 100% oxygen***
- The patient's presentation with **soot on her face and clothes**, and unconsciousness after a house fire, strongly suggests **carbon monoxide (CO) poisoning** and potential **cyanide poisoning**.
- **100% oxygen** is the first-line treatment for CO poisoning, as it rapidly displaces CO from hemoglobin and accelerates its elimination.
*Sodium nitrite*
- Sodium nitrite is used to treat **cyanide poisoning** by inducing methemoglobinemia, which then binds to cyanide.
- While cyanide poisoning is possible in house fires, **CO poisoning is more immediate and life-threatening** in terms of respiratory compromise.
*Penicillamine*
- Penicillamine is a **chelating agent** used primarily for **copper poisoning** (e.g., Wilson's disease) or severe lead poisoning.
- It has no role in the immediate treatment of smoke inhalation or carbon monoxide poisoning.
*Pyridoxine (vitamin B6)*
- Pyridoxine is the antidote for **isoniazid overdose** and can be used for **ethylene glycol poisoning**.
- It is not indicated for the management of smoke inhalation or carbon monoxide poisoning.
*N-acetylcysteine*
- N-acetylcysteine is the antidote for **acetaminophen (paracetamol) overdose** and is also used as a mucolytic.
- It is not indicated for the immediate treatment of smoke inhalation or carbon monoxide poisoning.
More Hyperbaric oxygen therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.