Factors affecting wound healing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Factors affecting wound healing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Factors affecting wound healing US Medical PG Question 1: A 62-year-old woman is hospitalized for an open reduction of a fracture of her right femur following a motor vehicle accident 2 hours prior. She has had rheumatoid arthritis for 12 years. She was hospitalized 1 month ago for an exacerbation of rheumatoid arthritis. Since then, she has been taking a higher dose of prednisone to control the flare. Her other medications include calcium supplements, methotrexate, and etanercept. She has had appropriate nutrition over the years with regular follow-ups with her healthcare providers. Her vital signs are within normal limits. Cardiovascular examination shows no abnormalities. In order to reduce the risk of post-operative wound failure, which of the following is the most appropriate modification in this patient’s drug regimen?
- A. Replacing prednisone with hydrocortisone
- B. Applying topical vitamin C
- C. Adding zinc supplementation (Correct Answer)
- D. Discontinuing steroids before surgery
- E. Increasing prednisone dose initially and tapering rapidly after 3 days
Factors affecting wound healing Explanation: ***Adding zinc supplementation***
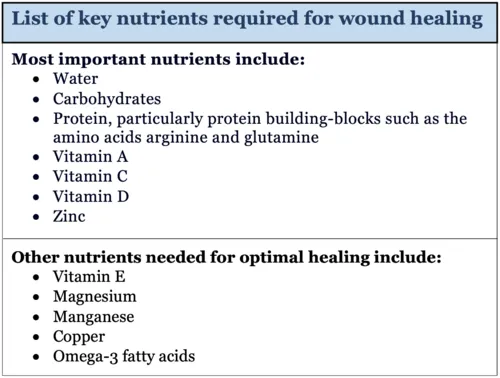
- **Zinc** plays a crucial role in **collagen synthesis**, immune function, and **wound healing**, making supplementation beneficial for reducing post-operative wound failure, especially in patients with chronic inflammatory conditions or those on corticosteroids.
- Chronic inflammation from **rheumatoid arthritis** and long-term **corticosteroid use** can impair zinc absorption and lead to deficiency, which exacerbates wound healing issues.
*Replacing prednisone with hydrocortisone*
- Both **prednisone** and **hydrocortisone** are corticosteroids, and switching between them does not inherently reduce the risk of wound failure.
- While prednisone is converted to prednisolone in the liver, hydrocortisone is directly active; both have similar immunosuppressive and anti-inflammatory effects that can impair wound healing.
*Applying topical vitamin C*
- **Topical vitamin C** is primarily used for its antioxidant properties and role in collagen synthesis in the skin, but its systemic effect on deep surgical wound healing is limited.
- **Systemic vitamin C deficiency** can impair wound healing, but the patient's history of appropriate nutrition suggests this is less likely to be the primary issue.
*Discontinuing steroids before surgery*
- Abruptly discontinuing **prednisone**, especially in a patient on a higher dose for an **RA flare**, carries a high risk of causing an **adrenal crisis**, which is life-threatening.
- Steroids are typically continued at a stress-dose equivalent during surgery to prevent **adrenal insufficiency**, not discontinued.
*Increasing prednisone dose initially and tapering rapidly after 3 days*
- Increasing the **prednisone dose** pre-operatively could further suppress the immune system and impair wound healing, increasing the risk of infection and dehiscence.
- While a **stress-dose steroid** regimen is appropriate, the goal is to provide physiological replacement, not to significantly increase the dose beyond what is necessary to prevent adrenal crisis.
Factors affecting wound healing US Medical PG Question 2: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Factors affecting wound healing Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Factors affecting wound healing US Medical PG Question 3: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Factors affecting wound healing Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Factors affecting wound healing US Medical PG Question 4: A 45-year-old man presents with lethargy, muscle aches, and dry skin. He is underweight and has very particular eating habits. Physical examination reveals swollen bleeding gums, cracked lips, petechiae, perifollicular hemorrhage, and corkscrew hairs. Laboratory tests reveal a nutritional deficiency. Which of the following is the key function of the most likely deficient nutrient?
- A. Hydroxylation of lysine and proline residues in collagen synthesis (Correct Answer)
- B. Precursor of serotonin
- C. Component of the visual pigment rhodopsin
- D. Gamma-carboxylation of glutamate residues in clotting factors
- E. Cofactor in carboxylase reactions
Factors affecting wound healing Explanation: ***Hydroxylation of lysine and proline residues in collagen synthesis***
- The patient's symptoms of **swollen, bleeding gums**, **petechiae**, **perifollicular hemorrhage**, and **corkscrew hairs** are classic signs of **scurvy**, caused by a severe deficiency of **vitamin C**.
- **Vitamin C** (ascorbic acid) is a crucial **cofactor** for **prolyl hydroxylase** and **lysyl hydroxylase**, enzymes essential for the hydroxylation of **proline** and **lysine** residues in **collagen** synthesis, which stabilizes the collagen triple helix.
*Precursor of serotonin*
- **Serotonin** is synthesized from the amino acid **tryptophan**, not vitamin C.
- Deficiency of serotonin precursors is not associated with the bleeding and connective tissue problems observed in this patient.
*Component of the visual pigment rhodopsin*
- **Rhodopsin** is a visual pigment found in the retina, and its formation requires **vitamin A** (retinol).
- Deficiency of vitamin A leads to **night blindness** and xerophthalmia, not the symptoms described.
*Gamma-carboxylation of glutamate residues in clotting factors*
- This process is essential for the activation of several **blood clotting factors** (II, VII, IX, X) and is dependent on **vitamin K**.
- Vitamin K deficiency can lead to bleeding diathesis, but the specific mucocutaneous and follicular signs point away from this.
*Cofactor in carboxylase reactions*
- **Biotin** (vitamin B7) acts as a cofactor for **carboxylase enzymes**, which are involved in fatty acid synthesis, gluconeogenesis, and amino acid metabolism.
- While biotin deficiency can cause skin and hair problems, it does not typically present with the specific bleeding and perifollicular hemorrhages seen with scurvy.
Factors affecting wound healing US Medical PG Question 5: A 56-year-old woman undergoes open reduction and internal fixation of the distal tibia 1 day after a fall. She has had rheumatoid arthritis for 12 years and diabetes mellitus for 2 years. Her medications over the past year have included metformin, prednisone, calcium supplements, and methotrexate. Prior to surgery, insulin was added to her medications, and the dose of prednisone was increased. She has had appropriate nutrition over the years with regular follow-ups with her healthcare professional. Which of the following is the most appropriate supplement to prevent wound failure in this patient?
- A. Glutamine
- B. Zinc
- C. Vitamin A
- D. Arginine
- E. Vitamin C (Correct Answer)
Factors affecting wound healing Explanation: ***Vitamin C***
- This patient is at high risk for **wound healing complications** due to her comorbidities (diabetes, rheumatoid arthritis) and medications (prednisone, methotrexate). **Vitamin C** (ascorbic acid) is essential for **collagen synthesis** and cross-linking, which is crucial for wound strength and tissue repair.
- While other options play a role in wound healing, Vitamin C is particularly important in patients with **impaired healing** due to chronic inflammation, corticosteroid use, and metabolic disorders, as it counteracts their negative effects on collagen formation.
*Glutamine*
- **Glutamine** is an important fuel for rapidly dividing cells, including immune cells and fibroblasts, and can be beneficial in catabolic states.
- However, its role in directly counteracting the specific challenges of this patient's wound healing (corticosteroid use, diabetes, rheumatoid arthritis) is **less direct** compared to Vitamin C's role in collagen synthesis.
*Zinc*
- **Zinc** is a cofactor for numerous enzymes involved in cell proliferation, immune function, and collagen synthesis.
- While important, zinc deficiency is not explicitly indicated, and its role as a primary intervention to prevent wound failure in a patient with **prednisone-induced healing impairment** is secondary to vitamin C.
*Vitamin A*
- **Vitamin A** can help reverse the negative effects of **corticosteroids** on wound healing by promoting epithelialization and collagen synthesis.
- While relevant due to prednisone use, its overall importance in **collagen formation** and direct wound strength is not as profound or broad as Vitamin C.
*Arginine*
- **Arginine** is a precursor for nitric oxide, which improves blood flow to wounds, and is involved in collagen formation and immune function.
- Although beneficial for wound healing, particularly in critically ill patients, it is **not the most appropriate single supplement** for addressing the specific collagen synthesis impairment seen in this patient's context of corticosteroid use and chronic disease.
Factors affecting wound healing US Medical PG Question 6: A 39-year-old man comes to the physician for a follow-up examination. He was treated for a urinary tract infection with trimethoprim-sulfamethoxazole 2 months ago. He is paraplegic as a result of a burst lumbar fracture that occurred after a fall 5 years ago. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He performs clean intermittent catheterization daily. He has smoked one pack of cigarettes daily for 19 years. His temperature is 37.1°C (98.8°F), pulse is 95/min, respirations are 14/min, and blood pressure is 120/80 mm Hg. He appears malnourished. Examination shows palpable pedal pulse. Multiple dilated tortuous veins are present over both lower extremities. There is a 2-cm wound surrounded by partial-thickness loss of skin and a pink wound bed over the right calcaneum. Neurologic examination shows paraparesis. His hemoglobin A1c is 6.5%, and fingerstick blood glucose concentration is 134 mg/dL. Which of the following is most likely to have prevented this patient's wound?
- A. Broad-spectrum antibiotic therapy
- B. Cessation of smoking
- C. Heparin therapy
- D. Topical antibiotic therapy
- E. Frequent position changes (Correct Answer)
Factors affecting wound healing Explanation: ***Frequent position changes***
- This patient is paraplegic, which increases his risk for **pressure ulcers** due to prolonged immobility and sustained pressure on bony prominences like the calcaneum.
- **Frequent repositioning** redistributes pressure, preventing skin breakdown and promoting circulation, thereby avoiding pressure injuries.
*Broad-spectrum antibiotic therapy*
- The wound is described as a **partial-thickness loss** with a pink wound bed, suggesting it's not primarily an infected wound requiring broad-spectrum antibiotics to prevent its formation.
- Antibiotics are used to **treat existing infections**, not prevent pressure ulcers in a non-infected state.
*Cessation of smoking*
- While **smoking impairs wound healing** and overall vascular health, it is not the most direct or primary preventative measure for a pressure ulcer caused by immobility.
- Smoking cessation would improve **long-term vascular health** and *ulcer healing*, but frequent position changes addresses the immediate cause of pressure.
*Heparin therapy*
- **Heparin** is an anticoagulant used to prevent **thrombosis** (blood clots), which is not the primary mechanism behind pressure ulcer formation.
- While immobility can contribute to deep vein thrombosis, heparin would not prevent the **mechanical pressure-induced skin damage** that causes a calcaneal wound.
*Topical antibiotic therapy*
- Similar to systemic antibiotics, topical antibiotics are used for **treating localized infections** or preventing them in *open wounds*.
- This wound is a result of pressure, and preventing its formation requires addressing the pressure itself, not merely applying antibiotics to the skin surface.
Factors affecting wound healing US Medical PG Question 7: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Factors affecting wound healing Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Factors affecting wound healing US Medical PG Question 8: A previously healthy 5-year-old boy is brought to the emergency department 15 minutes after sustaining an injury to his right hand. His mother says that she was cleaning the bathroom when he accidentally knocked over the drain cleaner bottle and spilled the liquid onto his hand. On arrival, he is crying and holding his right hand in a flexed position. His temperature is 37.7°C (99.8°F), pulse is 105/min, respirations are 25/min, and blood pressure is 105/65 mm Hg. Examination of the right hand shows a 4 x 4 cm area of reddened, blistered skin. The area is very tender to light touch. His ability to flex and extend the right hand are diminished. Radial pulses are palpable. Capillary refill time is less than 3 seconds. Which of the following is the most appropriate next step in management?
- A. Irrigate with water (Correct Answer)
- B. Apply split-thickness skin graft
- C. Apply silver sulfadiazine
- D. Apply mineral oil
- E. Perform escharotomy
Factors affecting wound healing Explanation: ***Irrigate with water***
- The immediate and most crucial step for a **chemical burn** is copious **irrigation with water** to remove the offending agent and prevent further tissue damage.
- This action minimizes the duration of contact between the **corrosive substance** and the skin, halting the chemical reaction.
*Apply split-thickness skin graft*
- A **skin graft** is a surgical procedure typically reserved for **deep burns** and is not the immediate first step for chemical exposure.
- It would be considered later in management if the burn resulted in **full-thickness tissue loss** and incomplete wound healing.
*Apply silver sulfadiazine*
- **Silver sulfadiazine** is an antimicrobial cream used to prevent infection in **thermal burns** after initial wound care.
- It is not indicated as the first line of treatment for a **chemical burn** and would not remove the chemical agent from the skin.
*Apply mineral oil*
- Applying **mineral oil** is not the appropriate initial treatment for a **chemical burn** and could potentially trap the chemical, worsening the injury.
- The priority is to dilute and remove the chemical, which mineral oil cannot do effectively.
*Perform escharotomy*
- An **escharotomy** is a surgical incision through burn eschar used to relieve pressure in **circumferential full-thickness burns** that compromise circulation.
- This procedure is not indicated as the initial management for a **chemical burn** and is only considered for severe, deep burns with vascular compromise.
Factors affecting wound healing US Medical PG Question 9: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Factors affecting wound healing Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
Factors affecting wound healing US Medical PG Question 10: A 42-year-old man sustains a deep laceration requiring surgical debridement. The wound care team debates between primary closure versus healing by secondary intention. The wound is 6 cm long, 2 cm wide, located on the lower leg with mild contamination from soil exposure, and the patient is a heavy smoker with peripheral vascular disease. Evaluate which approach best synthesizes the risk-benefit analysis for optimal outcome?
- A. Skin grafting after granulation tissue formation
- B. Immediate primary closure with prophylactic antibiotics
- C. Delayed primary closure after 3-5 days of wound observation (Correct Answer)
- D. Healing by secondary intention with negative pressure therapy
- E. Primary closure with tension-relieving retention sutures
Factors affecting wound healing Explanation: ***Delayed primary closure after 3-5 days of wound observation***
- This approach, also known as **tertiary intention**, is ideal for **contaminated wounds** as it allows time for the inflammatory phase to reduce bacterial load before final closure.
- It balances the risk of infection from **soil exposure** and **peripheral vascular disease** with the benefit of better functional and cosmetic outcomes compared to secondary intention.
*Skin grafting after granulation tissue formation*
- This technique is typically reserved for **extensive skin loss** or large defects where edges cannot be approximated, which is not indicated for a 6 cm linear laceration.
- It involves a more complex surgical procedure and carries a high risk of failure in patients with **peripheral vascular disease** and **smoking-related** poor microcirculation.
*Immediate primary closure with prophylactic antibiotics*
- Primary closure of a **contaminated wound** significantly increases the risk of **wound dehiscence** and abscess formation, especially in a low-perfusion area like the lower leg.
- The patient’s history of **smoking** and **vascular disease** further impairs oxygen delivery and immune response, making immediate closure premature.
*Healing by secondary intention with negative pressure therapy*
- While this reduces infection risk, it leads to a prolonged healing period and significant **scar contracture**, which can impair movement on the lower leg.
- It is less efficient than delayed primary closure for a cleanable laceration and is usually reserved for **chronically infected** or non-approximable wounds.
*Primary closure with tension-relieving retention sutures*
- Placing sutures under tension in a patient with **peripheral vascular disease** further compromises **capillary perfusion**, leading to skin flap necrosis.
- Retention sutures do not address the primary concern of **bacterial contamination** from the soil, which remains trapped within the closed wound space.
More Factors affecting wound healing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.