Wound healing

On this page
🔬 The Cellular Orchestra: Wound Healing's Molecular Symphony
Wound healing transforms a breach in tissue integrity into restored function through a precisely choreographed cascade of inflammation, proliferation, and remodeling-yet clinical outcomes span from seamless repair to chronic non-healing ulcers. You'll master the molecular signals and cellular players driving each phase, develop pattern recognition skills to distinguish normal from pathologic healing, and apply evidence-based algorithms that optimize outcomes across diverse patient contexts. This journey builds from microscopic mechanisms to bedside decision-making, equipping you to predict complications, intervene strategically, and integrate wound management into comprehensive care.
The healing cascade begins within seconds of injury, activating multiple cellular pathways that must coordinate perfectly for optimal outcomes. 85% of surgical complications relate to impaired healing processes, making this knowledge essential for clinical excellence.
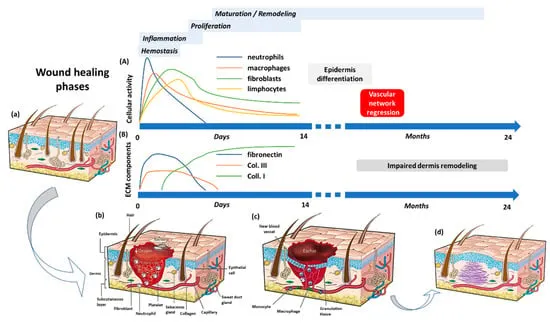
📌 Remember: HIPR - Hemostasis (0-30 minutes), Inflammation (1-5 days), Proliferation (4-21 days), Remodeling (21 days-2 years). Each phase overlaps with precise timing that determines healing success rates.
-
Hemostasis Phase (0-30 minutes)
- Platelet aggregation within 15 seconds of injury
- Fibrin clot formation peaks at 3-5 minutes
- Thrombin converts fibrinogen at >90% efficiency
- Clot strength reaches 80% maximum by 10 minutes
- Vasoconstriction reduces bleeding by 60-70%
-
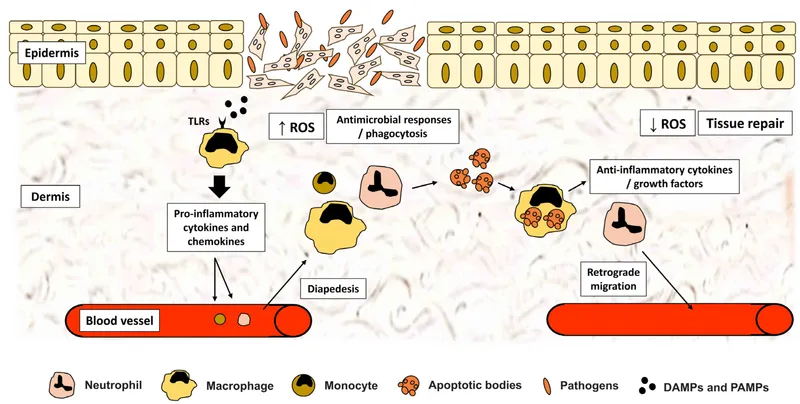
Inflammatory Phase (1-5 days)
- Neutrophil infiltration peaks at 24-48 hours
- Macrophage activation occurs by 72 hours
- M1 macrophages dominate days 1-3 (pro-inflammatory)
- M2 macrophages emerge day 3+ (tissue repair)
- Cytokine release follows TNF-α → IL-1β → IL-6 sequence
| Phase | Duration | Key Cells | Primary Function | Success Markers | Failure Signs |
|---|---|---|---|---|---|
| Hemostasis | 0-30 min | Platelets, RBCs | Bleeding control | Clot formation <5 min | Continued bleeding >30 min |
| Inflammation | 1-5 days | Neutrophils, Macrophages | Debris clearance | Controlled swelling | Excessive inflammation >7 days |
| Proliferation | 4-21 days | Fibroblasts, Endothelial | Tissue building | Granulation tissue | Poor tissue quality |
| Remodeling | 21 days-2 years | Fibroblasts | Strength restoration | Tensile strength >80% | Weak scar formation |
💡 Master This: The 3-day rule - healthy wounds show decreased erythema, reduced exudate, and early granulation tissue by day 3. Absence of these markers predicts 85% of healing complications.
Understanding cellular coordination patterns enables prediction of healing outcomes and guides intervention timing. Connect these foundational phases through proliferation mechanisms to master tissue regeneration principles.
🔬 The Cellular Orchestra: Wound Healing's Molecular Symphony
⚙️ The Regeneration Engine: Cellular Mechanisms Driving Repair
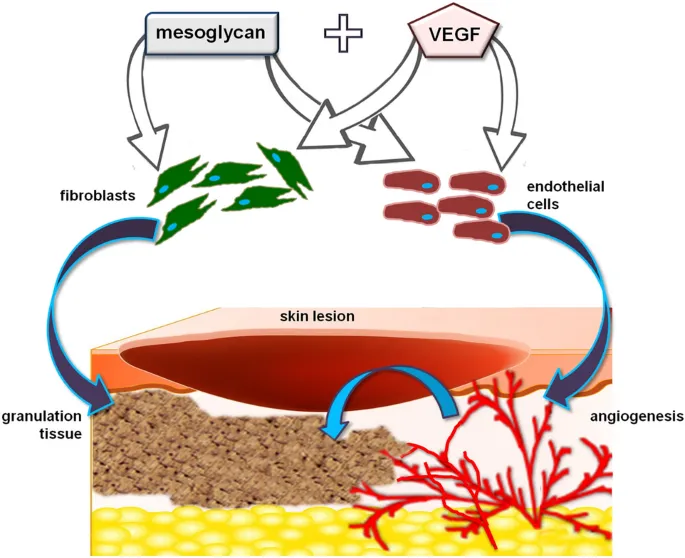
Growth factor cascades initiate within minutes of injury, with PDGF concentrations increasing 10-fold by 1 hour. VEGF levels peak at 3-7 days, driving angiogenesis that restores >95% of tissue perfusion in successful healing.
-
Growth Factor Hierarchy
- PDGF (Platelet-Derived Growth Factor)
- Released within 5 minutes of platelet activation
- Stimulates fibroblast chemotaxis at ng/mL concentrations
- Peak activity: 24-72 hours post-injury
- VEGF (Vascular Endothelial Growth Factor)
- Hypoxia-induced expression increases >100-fold
- Drives endothelial proliferation at 50-200% normal rates
- Critical window: days 3-14 for optimal angiogenesis
- PDGF (Platelet-Derived Growth Factor)
-
Cellular Response Mechanisms
- Fibroblast Activation
- Migration velocity: 20-50 μm/hour toward injury site
- Collagen production increases 300-500% above baseline
- Type III collagen dominates first 2 weeks (60-80% of total)
- Angiogenesis Process
- Capillary sprouting begins day 3-4 post-injury
- New vessel density peaks at 150-200% normal by day 7
- Perfusion restoration: 80% by week 2, 95% by week 4
- Fibroblast Activation
📌 Remember: VEGF-PDGF-TGF sequence - Vascular growth (days 3-7), Proliferation signals (days 1-14), Tissue remodeling (weeks 3-52). Disruption of any factor reduces healing success by >50%.
| Growth Factor | Peak Activity | Primary Target | Concentration Change | Clinical Significance |
|---|---|---|---|---|
| PDGF | 24-72 hours | Fibroblasts | 10-fold increase | Drives granulation tissue |
| VEGF | 3-7 days | Endothelial cells | 100-fold increase | Essential for angiogenesis |
| TGF-β | 7-21 days | Multiple cell types | 5-fold increase | Controls scar formation |
| EGF | 1-3 days | Epithelial cells | 3-fold increase | Promotes re-epithelialization |
| FGF | 2-14 days | Multiple cell types | 8-fold increase | Supports proliferation |
💡 Master This: The growth factor window - optimal healing requires PDGF within 24 hours, VEGF by day 3, and TGF-β regulation by week 1. Missing any window increases chronic wound risk by 40-60%.
Cellular mechanisms create the foundation for tissue regeneration, but clinical success depends on recognizing normal versus pathological healing patterns. Connect these molecular insights through pattern recognition frameworks to master healing assessment.
⚙️ The Regeneration Engine: Cellular Mechanisms Driving Repair
🎯 The Healing Detective: Pattern Recognition for Clinical Success
-
Healthy Healing Patterns
- Color Progression: Red → Pink → White over 2-6 weeks
- Bright red granulation tissue by day 3-5
- Pink epithelialization edges by day 5-7
- Pale pink mature tissue by week 2-4
- Size Reduction: 10-15% weekly area decrease
- Linear wounds: 1-2mm daily edge approximation
- Circular wounds: 5-10% diameter reduction weekly
- Depth healing: 0.5-1mm daily granulation tissue growth
- Color Progression: Red → Pink → White over 2-6 weeks
-
Warning Pattern Recognition
- Infection Indicators
- Temperature elevation >38.5°C with wound correlation
- Purulent drainage with >10⁵ CFU/mL bacterial count
- Expanding erythema >2cm beyond wound margins
- Pain increase >3 points on 10-point scale
- Healing Failure Patterns
- No size reduction after 2 weeks of optimal care
- Pale or gray granulation tissue indicating poor perfusion
- Rolled wound edges suggesting chronic inflammation
- Friable tissue that bleeds with minimal manipulation
- Infection Indicators
📌 Remember: NERDS for superficial infection - Non-healing, Exudative, Red/bleeding tissue, Debris, Smell. STONEES for deep infection - Size increase, Temperature, Os (probes to bone), New breakdown, Erythema, Edema, Smell.
| Assessment Parameter | Normal Range | Warning Signs | Intervention Threshold | Clinical Action |
|---|---|---|---|---|
| Granulation Quality | Bright red, firm | Pale, friable | Gray/black tissue | Debridement required |
| Exudate Volume | Minimal to moderate | Excessive (>5mL/day) | Purulent drainage | Culture and antibiotics |
| Wound Size | 10-15% weekly reduction | <5% reduction | No change in 2 weeks | Reassess treatment plan |
| Pain Level | Decreasing trend | Increasing pain | >3 point increase | Evaluate for infection |
| Edge Appearance | Pink, approximating | Rolled, undermined | Callused edges | Surgical revision |
- Healing Velocity Calculations
- Linear Healing Rate: (Initial length - Current length) / Days elapsed
- Normal rate: 1-2mm/day for surgical incisions
- Concerning rate: <0.5mm/day indicates healing impairment
- Area Reduction Rate: (Initial area - Current area) / Initial area × 100 / Weeks
- Target rate: 10-15% weekly area reduction
- Chronic wound threshold: <5% reduction over 2 weeks
- Linear Healing Rate: (Initial length - Current length) / Days elapsed
💡 Master This: Pattern prediction - wounds with bright red granulation, minimal exudate, and 10%+ weekly size reduction heal in predicted timeframes 85% of the time. Deviations from this pattern require immediate intervention reassessment.
Pattern recognition enables early intervention, but systematic comparison of healing types reveals optimal treatment selection strategies. Connect these assessment skills through differential frameworks to master healing optimization.
🎯 The Healing Detective: Pattern Recognition for Clinical Success
⚖️ The Healing Spectrum: Systematic Discrimination for Optimal Outcomes
-
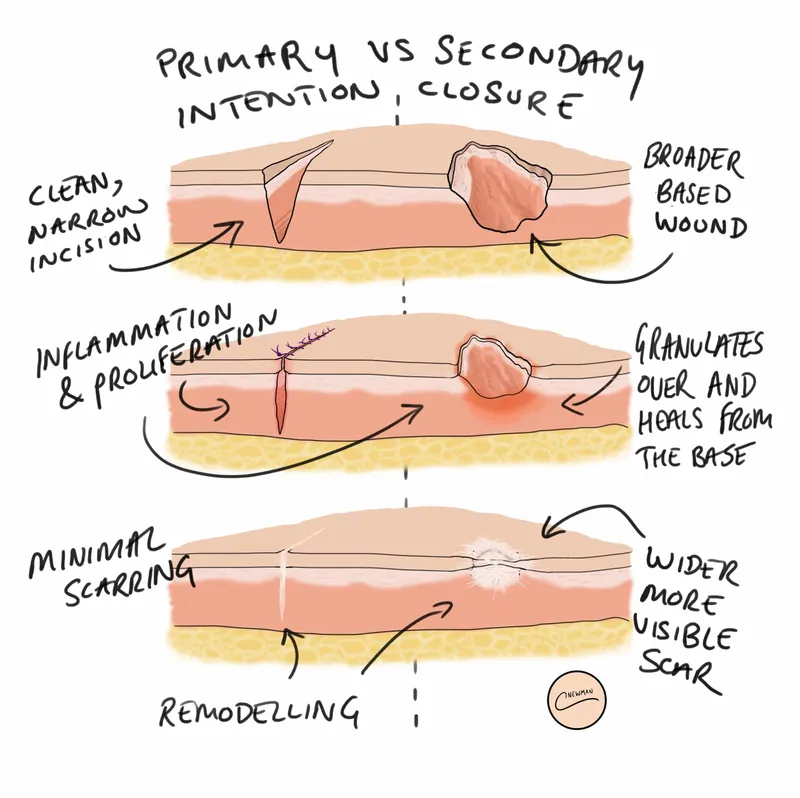
Primary Intention Healing
- Mechanism: Direct tissue approximation with minimal gap (<2mm)
- Epithelialization completes within 24-48 hours
- Tensile strength reaches 80% normal by 8 weeks
- Inflammatory phase limited to 2-3 days
- Success Criteria
- Infection rate: <2% with proper technique
- Healing time: 7-14 days for most surgical wounds
- Cosmetic outcome: Excellent in >90% of cases
- Functional restoration: 95-100% of original strength
- Mechanism: Direct tissue approximation with minimal gap (<2mm)
-
Secondary Intention Healing
- Mechanism: Granulation tissue formation with contraction and epithelialization
- Granulation phase: 5-21 days depending on wound size
- Contraction: 0.6-0.75mm/day wound edge movement
- Epithelialization: 1-2mm/day from wound margins
- Timeline Expectations
- Small wounds (<2cm): 2-4 weeks complete healing
- Medium wounds (2-5cm): 4-8 weeks healing time
- Large wounds (>5cm): 8-16 weeks or longer
- Mechanism: Granulation tissue formation with contraction and epithelialization
📌 Remember: PACE for healing intention selection - Primary (clean, approximated), Augmented (delayed primary), Contraction (secondary), Engineered (tertiary with grafts). Each method has specific indications and success rates.
| Healing Type | Tissue Loss | Closure Method | Healing Time | Infection Risk | Cosmetic Outcome |
|---|---|---|---|---|---|
| Primary | Minimal (<2mm) | Direct suture/staples | 7-14 days | <2% | Excellent (>90%) |
| Secondary | Moderate (2-20mm) | Natural granulation | 4-12 weeks | 5-15% | Good (60-80%) |
| Tertiary | Extensive (>20mm) | Delayed closure/grafts | 6-16 weeks | 10-25% | Variable (40-90%) |
| Augmented | Variable | Tissue substitutes | 2-8 weeks | 3-8% | Good to excellent |
- Primary Intention Candidates
- Clean wounds with <6-hour contamination time
- Adequate tissue for tension-free closure
- Good perfusion (capillary refill <3 seconds)
- Patient factors: healthy, non-diabetic, non-smoker
- Secondary Intention Indications
- Contaminated wounds requiring debridement
- Tissue loss preventing primary closure
- Infected wounds needing drainage
- Uncertain viability requiring observation
⭐ Clinical Pearl: Delayed primary closure (tertiary intention) combines benefits of both methods - allows contamination clearance for 3-5 days, then achieves primary intention healing rates in 80-85% of cases.
💡 Master This: The 6-hour rule for primary closure applies to clean wounds only. Contaminated wounds can be closed primarily up to 12-24 hours if thoroughly irrigated and debrided, achieving success rates >85%.
Systematic healing discrimination guides treatment selection, but evidence-based intervention algorithms optimize clinical outcomes. Connect these classification principles through treatment protocols to master healing optimization strategies.
⚖️ The Healing Spectrum: Systematic Discrimination for Optimal Outcomes
🔧 The Healing Optimizer: Evidence-Based Treatment Algorithms
-
Acute Wound Protocol
- Initial Management (First 24 hours)
- Hemostasis: Direct pressure for 10-15 minutes
- Irrigation: >100mL saline per cm of wound length
- Debridement: Remove >95% of foreign material
- Assessment: Document size, depth, contamination level
- Closure Decision Matrix
- Clean wounds <6 hours: Primary closure success rate 95%
- Contaminated wounds: Delayed closure after 3-5 days observation
- Tissue loss >20%: Consider reconstructive options
- Initial Management (First 24 hours)
-
Chronic Wound Algorithm
- Phase 1: Preparation (Weeks 1-2)
- Debridement: Remove 100% of necrotic tissue
- Infection control: Achieve <10⁵ CFU/mL bacterial load
- Moisture balance: Maintain optimal hydration without maceration
- Perfusion optimization: Ensure adequate blood flow
- Phase 2: Stimulation (Weeks 3-6)
- Advanced dressings: Growth factor-enhanced products
- Negative pressure: -125mmHg continuous therapy
- Biological agents: Platelet-rich plasma, stem cells
- Hyperbaric oxygen: 2.4 ATA for 90 minutes daily
- Phase 1: Preparation (Weeks 1-2)
| Treatment Phase | Duration | Success Metrics | Intervention Escalation | Expected Outcomes |
|---|---|---|---|---|
| Preparation | 1-2 weeks | >90% viable tissue | Add antimicrobials | Clean wound bed |
| Stimulation | 3-6 weeks | 15% weekly size reduction | Advanced therapies | Active granulation |
| Maturation | 6-12 weeks | Continued closure | Surgical options | Complete healing |
| Maintenance | Ongoing | No recurrence | Preventive measures | Functional restoration |
- Treatment Escalation Criteria
- Level 1: Standard care (weeks 1-2)
- Moist wound healing with appropriate dressings
- Infection prevention with antimicrobial barriers
- Pressure relief and positioning optimization
- Level 2: Advanced therapies (weeks 3-4)
- NPWT for wounds >2cm² with adequate perfusion
- Biological agents for stalled healing after 2 weeks
- Growth factors for diabetic ulcers with poor granulation
- Level 3: Surgical intervention (weeks 4-6)
- Debridement for >20% necrotic tissue persistence
- Flap coverage for exposed bone/tendon
- Amputation for non-salvageable tissue
- Level 1: Standard care (weeks 1-2)
⭐ Clinical Pearl: NPWT improves healing rates by 40-60% in appropriate wounds but requires adequate perfusion (ABI >0.8) and <20% necrotic tissue for optimal results.
💡 Master This: The 2-week rule - wounds showing <15% size reduction after 2 weeks of optimal care require treatment escalation. Early intervention prevents chronic wound development in 75% of cases.
Evidence-based algorithms optimize individual wound outcomes, but multi-system integration reveals the broader healing context. Connect these treatment protocols through systems integration to master comprehensive healing management.
🔧 The Healing Optimizer: Evidence-Based Treatment Algorithms
🌐 The Healing Ecosystem: Multi-System Integration and Advanced Insights
-
Metabolic-Healing Integration
- Glucose Control Impact
- HbA1c >8%: Healing time increases 2-3 fold
- Optimal range: 6.5-7.5% for fastest healing rates
- Hyperglycemia >180mg/dL: Impairs neutrophil function by 50%
- Protein Synthesis Requirements
- Increased needs: 1.2-1.5g/kg/day during active healing
- Collagen synthesis: Requires vitamin C >90mg/day
- Amino acid profile: Arginine and glutamine supplementation improves outcomes 25-30%
- Glucose Control Impact
-
Vascular-Perfusion Networks
- Microcirculation Optimization
- Capillary density: Must increase 150-200% for optimal healing
- Oxygen delivery: TcPO₂ >30mmHg required for granulation tissue
- Perfusion pressure: >30mmHg ankle pressure for healing potential
- Angiogenesis Regulation
- VEGF expression: Peaks at day 3-7, requires hypoxic stimulus
- Endothelial proliferation: 50-200% increase during active healing
- Vessel maturation: 2-4 weeks for functional perfusion
- Microcirculation Optimization
📌 Remember: MOVE for healing optimization - Metabolic control (glucose <180mg/dL), Oxygenation (TcPO₂ >30mmHg), Vascular perfusion (ABI >0.8), Endocrine balance (thyroid, cortisol normal). All systems must function optimally for maximum healing rates.
| System | Normal Function | Healing Impact | Optimization Target | Clinical Intervention |
|---|---|---|---|---|
| Metabolic | Glucose 70-140mg/dL | HbA1c <7.5% | Glycemic control | Insulin optimization |
| Vascular | ABI 0.9-1.3 | TcPO₂ >30mmHg | Perfusion enhancement | Revascularization |
| Immune | WBC 4-11K/μL | Balanced inflammation | Immune modulation | Anti-inflammatory agents |
| Nutritional | Albumin >3.5g/dL | Protein 1.2-1.5g/kg | Nutritional support | Supplementation |
| Endocrine | TSH 0.5-5.0mIU/L | Hormone optimization | Endocrine balance | Hormone replacement |
- Epigenetic Healing Factors
- DNA methylation patterns affect collagen gene expression
- Histone modifications influence growth factor sensitivity
- MicroRNA regulation controls angiogenesis timing
- Environmental factors (smoking, stress) alter epigenetic markers
- Microbiome-Healing Interactions
- Beneficial bacteria produce short-chain fatty acids promoting healing
- Dysbiosis increases inflammatory cytokines by 40-60%
- Probiotic supplementation improves healing rates in 65% of patients
- Antibiotic disruption delays healing by 20-30% through microbiome effects
⭐ Clinical Pearl: Circadian rhythm disruption (shift work, sleep disorders) impairs healing by 30-40% through growth hormone and cortisol dysregulation. Sleep optimization accelerates healing in 70% of patients.
💡 Master This: Systems thinking - optimal healing requires simultaneous optimization of all systems. Single-factor approaches achieve 60-70% success rates, while integrated approaches achieve 85-95% success rates.
Multi-system integration provides the foundation for advanced healing management, but practical mastery tools enable immediate clinical application. Connect these integration principles through rapid reference frameworks to achieve clinical excellence.
🌐 The Healing Ecosystem: Multi-System Integration and Advanced Insights
🎯 The Healing Mastery Toolkit: Rapid Clinical Reference Framework
-
Essential Clinical Arsenal
- Critical Numbers for Immediate Reference
- Healing velocity: 10-15% weekly area reduction (normal)
- Infection threshold: >10⁵ CFU/mL bacterial load
- Perfusion minimum: TcPO₂ >30mmHg for granulation
- Glucose target: <180mg/dL for optimal healing
- Protein needs: 1.2-1.5g/kg/day during active healing
- Pressure relief: <32mmHg interface pressure maximum
- Critical Numbers for Immediate Reference
-
Rapid Assessment Framework
- 30-Second Wound Evaluation
- Size measurement: Length × width × depth in cm
- Tissue quality: Red (healthy), Yellow (slough), Black (necrotic)
- Exudate assessment: Minimal, moderate, heavy (>5mL/day)
- Pain evaluation: 0-10 scale with trend assessment
- 60-Second Treatment Decision
- Primary closure: Clean wounds <6 hours, minimal tissue loss
- Secondary healing: Contaminated wounds, significant tissue loss
- Advanced therapy: <15% healing progress after 2 weeks
- 30-Second Wound Evaluation
📌 Remember: FAST-HEAL assessment - Factors (systemic), Area measurement, Stage/depth, Tissue quality, Healthy edges, Exudate character, Associated pain, Location/perfusion. Complete assessment in <2 minutes.
| Assessment Component | Normal Finding | Warning Sign | Action Required | Success Metric |
|---|---|---|---|---|
| Size Reduction | 10-15% weekly | <5% in 2 weeks | Reassess treatment | Return to normal rate |
| Tissue Quality | Bright red granulation | Pale/gray tissue | Improve perfusion | Pink, healthy tissue |
| Exudate | Minimal, serous | Purulent, excessive | Culture, antibiotics | Clear, minimal drainage |
| Pain Level | Decreasing trend | Increasing pain | Evaluate infection | Pain resolution |
| Edge Appearance | Pink, approximating | Rolled, undermined | Debride edges | Healthy edge migration |
- Standard Care Indications (Success Rate 80-90%)
- Acute wounds with good perfusion
- Clean surgical incisions
- Superficial abrasions and minor lacerations
- Advanced Therapy Triggers (Success Rate 85-95%)
- Stalled healing after 2 weeks optimal care
- Chronic wounds with >20% necrotic tissue
- Diabetic ulcers with poor granulation
- Surgical Intervention Criteria (Success Rate 90-95%)
- Exposed bone/tendon requiring coverage
- Large tissue defects >5cm diameter
- Failed conservative management after 4-6 weeks
⭐ Clinical Pearl: The "Rule of 15s" - 15% weekly size reduction, 15 days maximum for inflammation phase, 15 minutes hemostasis time, 15mg/dL protein increase needed for healing. Deviations predict 85% of complications.
💡 Master This: Healing prediction accuracy - wounds meeting all normal criteria heal in predicted timeframes 90% of the time. Single criterion deviation reduces success to 70%, multiple deviations to <50%.
This mastery toolkit transforms complex wound healing knowledge into immediately actionable clinical expertise, enabling rapid assessment, accurate diagnosis, and optimal treatment selection for superior patient outcomes.
🎯 The Healing Mastery Toolkit: Rapid Clinical Reference Framework
Practice Questions: Wound healing
Test your understanding with these related questions
A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?













