Venous insufficiency and varicose vein treatment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Venous insufficiency and varicose vein treatment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Venous insufficiency and varicose vein treatment US Medical PG Question 1: A 52-year-old man presents to the emergency department because of pain and swelling in his left leg over the past few hours. He traveled from Sydney to Los Angeles 2 days ago. He has had type 2 diabetes mellitus for 10 years and takes metformin for it. He has smoked a pack of cigarettes daily for 25 years. His temperature is 36.9°C (98.4°F), the blood pressure is 140/90 mm Hg, and the pulse is 90/min. On examination, the left calf is 5 cm greater in circumference than the right. The left leg appears more erythematous than the right with dilated superficial veins. Venous duplex ultrasound shows non-compressibility. Which of the following best represents the mechanism of this patient’s illness?
- A. Impaired venous blood flow (Correct Answer)
- B. Subcutaneous soft-tissue infection that may extend to the deep fascia
- C. Infection of the dermis and subcutaneous tissues
- D. Impaired arterial blood flow
- E. Impaired lymphatic flow
Venous insufficiency and varicose vein treatment Explanation: ***Impaired venous blood flow***
- The patient's symptoms (unilateral leg pain and swelling, erythema, dilated superficial veins, recent long-haul travel) and the **venous duplex ultrasound** finding of **non-compressibility** are highly indicative of **deep vein thrombosis (DVT)**, which results from impaired venous outflow.
- Risk factors such as **long-haul travel** (venous stasis), **smoking** (endothelial damage), and potentially **diabetes** contribute to a hypercoagulable state.
*Impaired lymphatic flow*
- This typically presents as **lymphedema**, characterized by chronic, often pitting edema, and skin changes like thickening (peau d'orange), but usually without acute erythema or dilated superficial veins in this context.
- **Venous duplex ultrasound** would not show non-compressibility in cases of impaired lymphatic flow, as veins themselves would be clear.
*Subcutaneous soft-tissue infection that may extend to the deep fascia*
- This describes **necrotizing fasciitis**, a severe infection often characterized by rapid progression, severe pain disproportionate to examination findings, blistering, and systemic toxicity, which are not clearly evident here.
- While there is erythema, the key diagnostic finding is the **non-compressible vein**, not signs of crepitus or rapidly spreading infection.
*Infection of the dermis and subcutaneous tissues*
- This describes **cellulitis**, which presents with localized redness, warmth, swelling, and tenderness, often with an entry point.
- While some symptoms overlap (erythema, swelling), the **venous duplex ultrasound finding of non-compressibility** definitively points away from a simple skin infection and towards a vascular obstruction.
*Impaired arterial blood flow*
- This presents as **acute limb ischemia**, characterized by the "6 Ps": pain, pallor, pulselessness, paresthesias, poikilothermia (coldness), and paralysis.
- The patient's leg is swollen and erythematous, not pale and cold, and the ultrasound directly implicates venous rather than arterial occlusion.
Venous insufficiency and varicose vein treatment US Medical PG Question 2: A 50-year-old man presents to the emergency department with pain and swelling of his right leg for the past 2 days. Three days ago he collapsed on his leg after tripping on a rug. It was a hard fall and left him with bruising of his leg. Since then the pain and swelling of his leg have been gradually increasing. Past medical history is noncontributory. He lives a rather sedentary life and smokes two packs of cigarettes per day. The vital signs include heart rate 98/min, respiratory rate 15/min, temperature 37.8°C (100.1°F), and blood pressure 100/60 mm Hg. On physical examination, his right leg is visibly swollen up to the mid-calf with pitting edema and moderate erythema. Peripheral pulses in the right leg are weak and the leg is tender. Manipulation of the right leg is negative for Homan’s sign. What is the next best step in the management of this patient?
- A. Send the patient to surgery for an emergency fasciotomy
- B. Start intravenous heparin therapy immediately
- C. Make a diagnosis of deep vein thrombosis based on history and physical
- D. Perform a venous ultrasound (Correct Answer)
- E. Perform intravenous venography within 24 hours
Venous insufficiency and varicose vein treatment Explanation: ***Perform a venous ultrasound***
- The patient's presentation with acute unilateral leg swelling, pain, erythema, and weak peripheral pulses following trauma, along with **risk factors for venous thromboembolism (sedentary lifestyle, smoking)**, strongly suggests the possibility of a **deep vein thrombosis (DVT)**.
- **Venous ultrasound** is the **most appropriate and preferred initial diagnostic test** for suspected DVT due to its **non-invasiveness, accessibility, and high sensitivity and specificity**.
*Send the patient to surgery for an emergency fasciotomy*
- **Fasciotomy** is indicated for **acute compartment syndrome**, which typically presents with severe pain out of proportion to injury, pain on passive stretch, paresthesia, and tense compartments.
- While the patient has swelling and tenderness, the weak pulses are concerning, but the overall picture does not definitively point to compartment syndrome needing immediate fasciotomy without further diagnostic workup.
*Start intravenous heparin therapy immediately*
- Though DVT is suspected, **heparin therapy should not be initiated empirically without definitive diagnostic confirmation** due to the risk of bleeding complications.
- A **venous ultrasound is crucial to confirm the diagnosis** before starting anticoagulation.
*Make a diagnosis of deep vein thrombosis based on history and physical*
- While the clinical picture is highly suggestive of DVT, **clinical diagnosis alone is not sufficiently accurate** to initiate potentially risky treatments like anticoagulation.
- **Objective diagnostic testing (like ultrasound)** is essential to confirm the presence of a DVT.
*Perform intravenous venography within 24 hours*
- **Intravenous venography** is considered the **gold standard** for diagnosing DVT, but it is an **invasive procedure** with risks (e.g., contrast nephropathy, allergic reactions, radiation exposure).
- It is **rarely used as a first-line diagnostic test** and is usually reserved for cases where ultrasound results are inconclusive or discordant with clinical suspicion.
Venous insufficiency and varicose vein treatment US Medical PG Question 3: A 52-year-old woman comes to the physician because of swelling of her legs for 2 months. She has noticed that her legs gradually swell up throughout the day. Two years ago, she underwent a coronary angioplasty. She has hypertension and coronary artery disease. She works as a waitress at a local diner. Her father died of liver cancer at the age of 61 years. She has smoked one pack of cigarettes daily for 31 years. She drinks one to two glasses of wine daily and occasionally more on weekends. Current medications include aspirin, metoprolol, and rosuvastatin. Vital signs are within normal limits. Examination shows 2+ pitting edema in the lower extremities. There are several dilated, tortuous veins over both calves. Multiple excoriation marks are noted over both ankles. Peripheral pulses are palpated bilaterally. The lungs are clear to auscultation. Cardiac examination shows no murmurs, gallops, or rubs. The abdomen is soft and nontender; there is no organomegaly. Which of the following is the most appropriate next step in management?
- A. Sclerotherapy
- B. CT scan of abdomen and pelvis
- C. Compression stockings (Correct Answer)
- D. Abdominal ultrasound
- E. Adjust antihypertensive medication
Venous insufficiency and varicose vein treatment Explanation: ***Compression stockings***
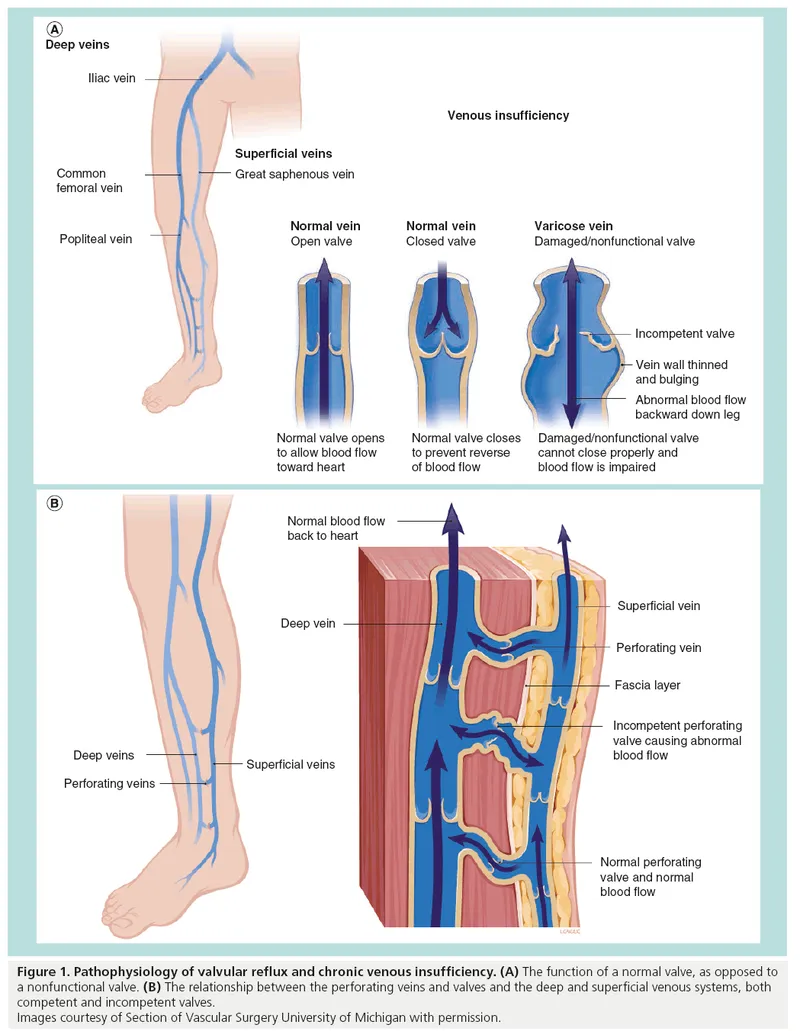
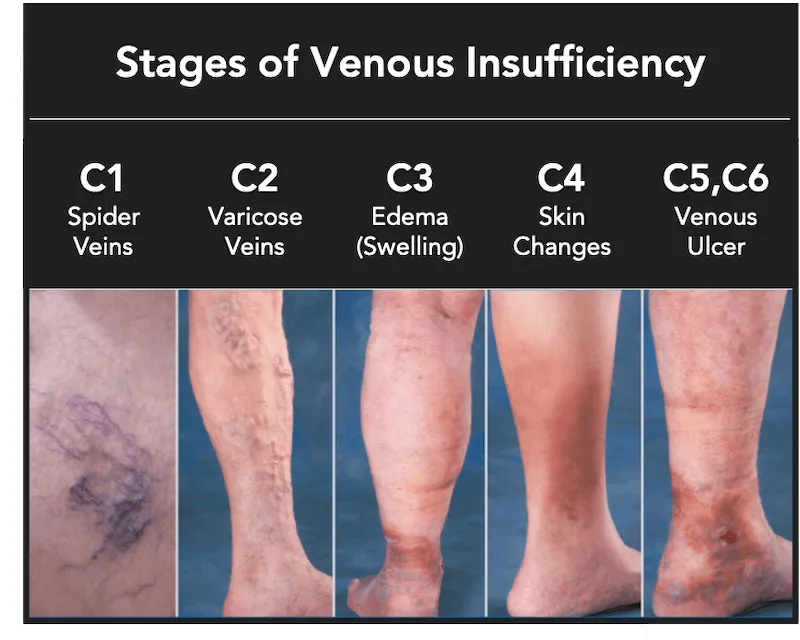
- The patient presents with **bilateral pitting edema**, **dilated, tortuous veins** (varicose veins), and symptoms that worsen throughout the day, which are classic signs of **chronic venous insufficiency (CVI)**.
- Her occupation as a waitress (prolonged standing) is a significant risk factor for CVI.
- **Compression stockings** are the first-line conservative treatment for CVI, helping to reduce edema and improve venous return.
*Sclerotherapy*
- **Sclerotherapy** is a procedure used to treat varicose veins by injecting a solution to close them.
- While it can be an option for varicose veins, it is typically considered after conservative measures like compression stockings have been tried and found to be insufficient, or for cosmetic reasons.
*CT scan of abdomen and pelvis*
- A **CT scan of the abdomen and pelvis** would be used to investigate more serious causes of edema, such as malignancy with IVC compression or lymphatic obstruction.
- Given the classic presentation of CVI with visible varicose veins, a CT scan is not the appropriate initial step.
*Adjust antihypertensive medication*
- The patient's vital signs are within normal limits, and her current medications (aspirin, metoprolol, rosuvastatin) are appropriate for her cardiac history.
- Metoprolol (a beta-blocker) does not typically cause peripheral edema; dihydropyridine calcium channel blockers would be more likely to cause peripheral edema, but she is not on these medications.
*Abdominal ultrasound*
- An **abdominal ultrasound** could be used to evaluate for liver disease or ascites, but the patient has no signs of hepatic dysfunction (no jaundice, ascites, or hepatomegaly).
- The prominent varicose veins and bilateral pitting edema that worsens with prolonged standing strongly point toward chronic venous insufficiency, making conservative management the appropriate first step.
Venous insufficiency and varicose vein treatment US Medical PG Question 4: A 68-year-old woman comes to the physician because of a 3-month history of an oozing, red area above the left ankle. She does not recall any trauma to the lower extremity. She has type 2 diabetes mellitus, hypertension, atrial fibrillation, and ulcerative colitis. She had a myocardial infarction 2 years ago and a stroke 7 years ago. She has smoked 2 packs of cigarettes daily for 48 years and drinks 2 alcoholic beverages daily. Current medications include warfarin, metformin, aspirin, atorvastatin, carvedilol, and mesalamine. She is 165 cm (5 ft 4 in) tall and weighs 67 kg (148 lb); BMI is 24.6 kg/m2. Her temperature is 36.7°C (98°F), pulse is 90/min, respirations are 12/min, and blood pressure is 135/90 mm Hg. Examination shows yellow-brown spots and dilated tortuous veins over the lower extremities. The feet and the left calf are edematous. Femoral, popliteal, and pedal pulses are palpable bilaterally. There is a 3-cm (1.2-in) painless, shallow, exudative ulcer surrounded by granulation tissue above the medial left ankle. There is slight drooping of the right side of the face. Which of the following is the most likely cause of this patient's ulcer?
- A. Peripheral neuropathy
- B. Drug-induced microvascular occlusion
- C. Chronic pressure
- D. Decreased arterial blood flow
- E. Venous insufficiency (Correct Answer)
Venous insufficiency and varicose vein treatment Explanation: ***Venous insufficiency***
- The presence of **edema**, **dilated tortuous veins**, and **yellow-brown spots** (hemosiderin deposition) on the lower extremities, along with a **painless, shallow, exudative ulcer** above the medial ankle, are classic signs of chronic venous insufficiency.
- The ulcer's location (medial malleolus) and its characteristics (granulation tissue, oozing) further support a venous etiology, as good arterial pulses indicate adequate inflow.
*Peripheral neuropathy*
- Ulcers due to peripheral neuropathy (e.g., in diabetes) are typically **painless** but often occur on the **plantar surface of the foot** or pressure points and can be deep.
- While the patient has diabetes, the clinical presentation with prominent venous stasis signs and edema points away from a primary neuropathic ulcer in this location.
*Drug-induced microvascular occlusion*
- Drug-induced microvascular occlusion (e.g., from **warfarin necrosis**) typically presents as painful, irregular, purpuric lesions that can progress to necrosis and ulceration, often occurring within days of starting the medication or with high doses.
- The 3-month history, painless nature, and specific signs of venous stasis do not align with drug-induced microvascular occlusion.
*Chronic pressure*
- Pressure ulcers develop over **bony prominences** due to prolonged pressure, leading to tissue ischemia and breakdown.
- This patient's ulcer is above the medial ankle, which is not a common site for pressure ulcers, and the presentation includes clear signs of venous hypertension, not just external compression.
*Decreased arterial blood flow*
- Ulcers due to decreased arterial blood flow (arterial ulcers) are typically **painful**, often located on the **toes, heels, or dorsum of the foot**, and have a "punched-out" appearance with **pale bases** and minimal granulation tissue.
- The presence of palpable pedal pulses and the painless nature of the ulcer rule out significant arterial insufficiency as the primary cause.
Venous insufficiency and varicose vein treatment US Medical PG Question 5: A 54-year-old woman comes to the physician because of a 6-month history of dull, persistent pain and swelling of her right leg. The pain is worse at the end of the day and is relieved by walking or elevating her feet. Two years ago, she developed acute deep vein thrombosis in her right calf after a long flight, which was treated with anticoagulants for 6 months. Physical examination shows 2+ pitting edema of her right leg. The skin around the right ankle shows a reddish-brown discoloration and multiple telangiectasias. She has dilated varicose veins in the right leg. Which of the following is most likely to establish the diagnosis?
- A. D-dimer assay
- B. Ankle-brachial pressure index
- C. Computerized tomography scan with contrast
- D. Duplex ultrasonography (Correct Answer)
- E. Nerve conduction studies
Venous insufficiency and varicose vein treatment Explanation: ***Duplex ultrasonography***
- **Duplex ultrasonography** is the gold standard for evaluating **venous insufficiency**, which is strongly suggested by the patient's history of **deep vein thrombosis (DVT)**, **chronic leg pain**, **pitting edema**, **stasis dermatitis** (reddish-brown discoloration), and **varicose veins**.
- This non-invasive imaging technique allows visualization of vein structure, blood flow, and valve function, helping to identify **venous reflux** or **obstruction**.
*D-dimer assay*
- A **D-dimer assay** is primarily used to **rule out acute DVT** or pulmonary embolism.
- While D-dimer levels may be elevated in chronic venous disease, it is **not specific** enough to establish a diagnosis of chronic venous insufficiency or its cause.
*Ankle-brachial pressure index*
- The **ankle-brachial pressure index (ABPI)** is used to diagnose **peripheral artery disease (PAD)** by comparing blood pressure in the ankle to the arm.
- This patient's symptoms are more consistent with **venous disease** rather than arterial insufficiency.
*Computerized tomography scan with contrast*
- A **CT scan with contrast** can visualize vascular structures but is **less sensitive and specific** for diagnosing venous insufficiency compared to duplex ultrasonography.
- It also involves **radiation exposure** and **contrast dye risks**, making it a less suitable initial diagnostic tool for this condition.
*Nerve conduction studies*
- **Nerve conduction studies** are used to diagnose **neuropathies** and conditions affecting the peripheral nerves and are not relevant for evaluating vascular issues.
- The patient's symptoms clearly point to a **vascular problem**, not a neurological one.
Venous insufficiency and varicose vein treatment US Medical PG Question 6: A 59-year-old man presents to his primary care provider complaining of bilateral calf cramping with walking for the past 7 months. His pain goes away when he stops walking; however, his condition affects his work as a mail carrier. His medical history is remarkable for type 2 diabetes mellitus, hyperlipidemia, and 25-pack-year smoking history. His ankle-brachial index (ABI) is found to be 0.70. The patient is diagnosed with mild to moderate peripheral artery disease. A supervised exercise program for 3 months, aspirin, and cilostazol are started. Which of the following is the best next step if the patient has no improvement?
- A. Revascularization (Correct Answer)
- B. Heparin
- C. Surgical decompression
- D. Pentoxifylline
- E. Amputation
Venous insufficiency and varicose vein treatment Explanation: ***Revascularization***
- For patients with **peripheral artery disease (PAD)** who fail to improve with conservative management (**supervised exercise, aspirin, and cilostazol**), **revascularization** is the next appropriate step to improve blood flow.
- This can be achieved through **endovascular procedures** (e.g., angioplasty with stenting) or **surgical bypass**, depending on the location and severity of the arterial blockage.
*Heparin*
- **Heparin** is an **anticoagulant** primarily used for acute thrombotic events or deep vein thrombosis (DVT), not for chronic management of stable claudication in PAD.
- It would not address the underlying **chronic arterial stenosis** causing the claudication symptoms.
*Surgical decompression*
- **Surgical decompression** is a treatment for conditions like **spinal stenosis** or **compartment syndrome**, not for peripheral arterial disease.
- The patient's symptoms (calf cramping with walking, resolving at rest) and **ABI of 0.70** are classic for **vascular claudication**, not nerve or muscle compression.
*Pentoxifylline*
- **Pentoxifylline** is an alternative medication used in PAD to improve blood flow by reducing blood viscosity.
- However, it is generally **less effective** than cilostazol and is typically considered when cilostazol is contraindicated or not tolerated, rather than as a next step after initial medical therapy failure with cilostazol.
*Amputation*
- **Amputation** is a last resort, usually reserved for **critical limb ischemia** with non-healing ulcers, gangrene, or intractable rest pain, where revascularization is not feasible or has failed.
- The patient's current symptoms are **intermittent claudication**, which is not immediately limb-threatening.
Venous insufficiency and varicose vein treatment US Medical PG Question 7: A 54-year-old man comes to the emergency department because of a 3-week history of intermittent swelling of his left arm and feeling of fullness in his head that is exacerbated by lying down and bending over to tie his shoes. Physical examination shows left-sided facial edema and distention of superficial veins in the neck and left chest wall. Which of the following is the most likely cause of this patient's symptoms?
- A. Cervical rib
- B. Mediastinal lymphoma
- C. Subclavian steal syndrome
- D. Apical lung tumor (Correct Answer)
- E. Right heart failure
Venous insufficiency and varicose vein treatment Explanation: ***Apical lung tumor***
- The symptoms of **facial edema**, **neck vein distention**, and **swelling of the left arm**, particularly when exacerbated by positional changes such as lying down or bending over, are classic signs of **superior vena cava (SVC) syndrome**.
- An **apical lung tumor (Pancoast tumor)** is a common cause of SVC syndrome due to its proximity to the SVC and surrounding structures, leading to compression.
- The **left-sided predominance** (left arm swelling, left facial edema, left chest wall venous distention) specifically points to a left apical mass compressing the left brachiocephalic vein and/or SVC.
*Cervical rib*
- A cervical rib can cause **thoracic outlet syndrome**, leading to neurovascular compression, but it typically presents with neurological symptoms (pain, numbness, weakness in the arm/hand) or arterial insufficiency rather than widespread facial and neck edema.
- While it can cause *venous compression*, resulting in arm swelling, the **facial edema and neck vein distention** suggest a more central venous obstruction like SVC syndrome rather than peripheral thoracic outlet compression.
*Mediastinal lymphoma*
- Malignancies in the mediastinum, such as lymphoma, can indeed cause SVC syndrome by compressing the SVC.
- However, mediastinal lymphomas typically cause **bilateral** symptoms due to their central location, whereas this patient has **predominant left-sided findings** (left arm swelling, left facial edema, left chest wall veins), which more specifically suggests a left apical lung mass.
- Additionally, lymphoma commonly presents with systemic "B symptoms" (fever, night sweats, weight loss) and generalized lymphadenopathy, which are not mentioned here.
*Subclavian steal syndrome*
- This syndrome results from **subclavian artery stenosis** proximal to the vertebral artery origin, causing **retrograde blood flow** in the vertebral artery to supply the arm.
- It presents with **arm claudication**, dizziness, and syncope, especially with arm exercise, rather than venous congestion and swelling of the face, neck, and arm.
- This is an **arterial** syndrome, not a **venous** syndrome.
*Right heart failure*
- **Right heart failure** causes systemic venous congestion, leading to symptoms like **peripheral edema** (especially in the lower extremities), **jugular venous distention**, and **hepatomegaly**.
- While it can cause jugular venous distension, it typically presents with **bilateral lower extremity edema** and *rarely* causes unilateral arm swelling or predominant facial edema, as seen here.
- The **positional exacerbation** and **unilateral left-sided findings** are not characteristic of right heart failure.
Venous insufficiency and varicose vein treatment US Medical PG Question 8: A 34-year-old woman, gravida 4, para 3, comes to the physician because of left ankle swelling for 2 months. She notes that the swelling is present throughout the day and decreases when she goes to sleep. One year ago, she has had an episode of deep venous thrombosis after the delivery of her third child. Her prepregnancy BMI was 34 kg/m2. Examination shows distended, tortuous veins in the legs bilaterally and pitting edema of the left ankle. There are erythematous scaling patches on the medial side of the left ankle. Duplex ultrasonography is performed. Which of the following directions of blood flow would most likely confirm the diagnosis?
- A. Femoral vein to external iliac vein
- B. Anterior tibial vein to popliteal vein
- C. Femoral vein to great saphenous vein (Correct Answer)
- D. Popliteal vein to small saphenous vein
- E. Dorsal venous arch to great saphenous vein
Venous insufficiency and varicose vein treatment Explanation: ***Femoral vein to great saphenous vein***
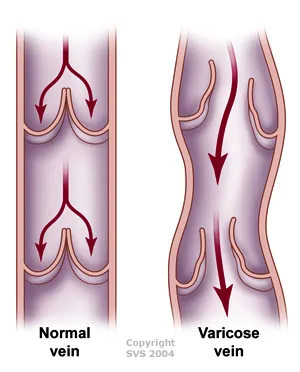
- This represents **reflux at the saphenofemoral junction (SFJ)**, the most common cause of **chronic venous insufficiency (CVI)**.
- Incompetent valves allow retrograde blood flow from the deep venous system (femoral vein) into the superficial system (great saphenous vein), causing increased venous pressure.
- This leads to the patient's presenting features: **varicose veins** (distended, tortuous veins), **pitting edema**, and **venous stasis dermatitis** (erythematous scaling patches).
- **Duplex ultrasonography** demonstrating this reversed flow pattern confirms the diagnosis of CVI due to SFJ incompetence.
- Risk factors include obesity (BMI 34), previous DVT, and multiple pregnancies—all present in this patient.
*Dorsal venous arch to great saphenous vein*
- This describes **normal antegrade flow** from the superficial dorsal venous arch upward into the great saphenous vein.
- This is the physiological direction of blood flow, not reflux or pathological flow.
- Would not be diagnostic of venous insufficiency.
*Anterior tibial vein to popliteal vein*
- This represents **normal antegrade flow** from the anterior tibial vein (deep vein of the leg) proximally to the popliteal vein.
- This is the normal physiological direction for venous return from the lower leg.
- Not indicative of valvular incompetence or venous insufficiency.
*Femoral vein to external iliac vein*
- This describes **normal antegrade flow** from the femoral vein proximally to the external iliac vein.
- This is the correct physiological direction of venous return from the lower extremity toward the heart.
- Not reflux and would not confirm venous insufficiency.
*Popliteal vein to small saphenous vein*
- This represents reflux at the **saphenopopliteal junction (SPJ)**, a less common site of venous insufficiency.
- While this can cause varicosities in the small saphenous distribution (posterior calf), it is less common than SFJ incompetence.
- The medial ankle location of skin changes and the distribution of findings are more consistent with great saphenous vein involvement than small saphenous vein.
Venous insufficiency and varicose vein treatment US Medical PG Question 9: A 35-year-old woman presents to her primary care physician for recurrent deep venous thrombosis (DVT) of her left lower extremity. She is a vegetarian and often struggles to maintain an adequate intake of non-animal based protein. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and currently denies any illicit drug use, although she endorses a history of heroin use (injection). Her past medical history is significant for 4 prior admissions for lower extremity swelling and pain that resulted in diagnoses of deep venous thrombosis. Her vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 16/min. On physical examination, her pulses are bounding, the patient's complexion is pale, breath sounds are clear, and heart sounds are normal. The spleen is mildly enlarged. She is admitted for DVT treatment and a full hypercoagulability workup. Which of the following is the best initial management for this patient?
- A. Begin heparin
- B. Begin warfarin, target INR 2.5–3.5
- C. Consult IR for IVC filter placement
- D. Begin heparin and warfarin (Correct Answer)
- E. Begin warfarin, target INR 2.0–3.0
Venous insufficiency and varicose vein treatment Explanation: ***Begin heparin and warfarin***
- For **acute DVT**, immediate anticoagulation with **heparin** (or another direct thrombin inhibitor/factor Xa inhibitor) is crucial to prevent clot propagation and pulmonary embolism.
- **Warfarin** is started concurrently, as it has a slower onset of action; heparin provides protection until warfarin reaches a therapeutic INR.
*Begin heparin*
- While **heparin** is the correct initial therapy for acute DVT, it is insufficient on its own for long-term management due to its short half-life and need for continuous infusion (unfractionated) or daily injections (low molecular weight).
- A long-term oral anticoagulant like warfarin or a direct oral anticoagulant (DOAC) is necessary for extended prophylaxis, especially in a patient with recurrent DVT.
*Begin warfarin, target INR 2.5–3.5*
- **Warfarin** is appropriate for long-term anticoagulation, but it has a delayed onset of action and requires several days to reach therapeutic levels, during which time the patient would be unprotected from clot extension or embolization.
- The initial target INR for most VTE is 2.0-3.0, though for recurrent events or certain conditions, a higher range might be considered later, but 2.5-3.5 is not the standard initial target.
*Consult IR for IVC filter placement*
- **IVC filters** are typically reserved for patients with an acute DVT who have a **contraindication to anticoagulation** or who experience recurrent PE despite adequate anticoagulation.
- There is no mention of contraindications to anticoagulation in this patient, and filters are not a primary treatment for acute DVT but rather a preventative measure against pulmonary embolism in specific high-risk scenarios.
*Begin warfarin, target INR 2.0–3.0*
- While **warfarin** at an INR target of 2.0-3.0 is a standard long-term therapy for DVT, beginning it alone is inappropriate for acute DVT due to its **delayed therapeutic effect**.
- Without concurrent rapid-acting anticoagulation (like heparin), the patient remains at high risk for complications while awaiting warfarin's full effect.
Venous insufficiency and varicose vein treatment US Medical PG Question 10: A 63-year-old man presents to the clinic complaining of burning bilateral leg pain which has been increasing gradually over the past several months. It worsens when he walks but improves with rest. His past medical and surgical history are significant for hypertension, hyperlipidemia, diabetes, and a 40-pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 167/108 mm Hg, pulse is 88/min, respirations are 13/min, and oxygen saturation is 95% on room air. Physical exam of the lower extremities reveals palpable but weak posterior tibial and dorsalis pedis pulses bilaterally. Which of the following is the best initial treatment for this patient's symptoms?
- A. Exercise and smoking cessation (Correct Answer)
- B. Lovenox and atorvastatin
- C. Lisinopril and atorvastatin
- D. Balloon angioplasty with stenting
- E. Femoral-popliteal bypass
Venous insufficiency and varicose vein treatment Explanation: ***Exercise and smoking cessation***
- This patient presents with symptoms highly suggestive of **peripheral artery disease (PAD)**, characterized by **intermittent claudication** (leg pain worsening with activity and improving with rest), and risk factors like diabetes, hypertension, hyperlipidemia, and smoking.
- **Smoking cessation** is the single most important modifiable risk factor, and a supervised **exercise program** (walking to the point of claudication) is the most effective initial treatment to improve walking distance and quality of life for PAD patients.
*Lovenox and atorvastatin*
- **Atorvastatin** is appropriate for dyslipidemia and cardiovascular risk reduction in PAD patients, but **Lovenox (low molecular weight heparin)** is an anticoagulant typically used for acute thrombotic events or VTE prophylaxis, not initial management of chronic stable claudication.
- While statins are important for secondary prevention, Lovenox does not directly address the primary management of claudication symptoms or underlying atherosclerotic progression in this stable setting.
*Lisinopril and atorvastatin*
- **Lisinopril** is an ACE inhibitor suitable for hypertension, which is important for overall cardiovascular health but not the primary initial treatment for claudication symptoms.
- While both medications address risk factors, they do not directly target the improvement of walking function and symptom relief as effectively as exercise and smoking cessation in the initial phase.
*Balloon angioplasty with stenting*
- Invasive revascularization procedures like **balloon angioplasty with stenting** are typically reserved for patients with more severe symptoms (e.g., rest pain, non-healing ulcers, critical limb ischemia) or those who have failed conservative management like exercise therapy.
- This is not the **best initial treatment** for a patient with stable claudication.
*Femoral-popliteal bypass*
- **Femoral-popliteal bypass** is a surgical revascularization procedure indicated for more severe PAD, particularly in cases of critical limb ischemia or long-segment occlusions that are not amenable to endovascular repair.
- Like angioplasty, it is a more aggressive intervention and not the **initial treatment of choice** for intermittent claudication.
More Venous insufficiency and varicose vein treatment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.