Vascular trauma management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vascular trauma management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vascular trauma management US Medical PG Question 1: A 50-year-old man presents to the emergency department with pain and swelling of his right leg for the past 2 days. Three days ago he collapsed on his leg after tripping on a rug. It was a hard fall and left him with bruising of his leg. Since then the pain and swelling of his leg have been gradually increasing. Past medical history is noncontributory. He lives a rather sedentary life and smokes two packs of cigarettes per day. The vital signs include heart rate 98/min, respiratory rate 15/min, temperature 37.8°C (100.1°F), and blood pressure 100/60 mm Hg. On physical examination, his right leg is visibly swollen up to the mid-calf with pitting edema and moderate erythema. Peripheral pulses in the right leg are weak and the leg is tender. Manipulation of the right leg is negative for Homan’s sign. What is the next best step in the management of this patient?
- A. Send the patient to surgery for an emergency fasciotomy
- B. Start intravenous heparin therapy immediately
- C. Make a diagnosis of deep vein thrombosis based on history and physical
- D. Perform a venous ultrasound (Correct Answer)
- E. Perform intravenous venography within 24 hours
Vascular trauma management Explanation: ***Perform a venous ultrasound***
- The patient's presentation with acute unilateral leg swelling, pain, erythema, and weak peripheral pulses following trauma, along with **risk factors for venous thromboembolism (sedentary lifestyle, smoking)**, strongly suggests the possibility of a **deep vein thrombosis (DVT)**.
- **Venous ultrasound** is the **most appropriate and preferred initial diagnostic test** for suspected DVT due to its **non-invasiveness, accessibility, and high sensitivity and specificity**.
*Send the patient to surgery for an emergency fasciotomy*
- **Fasciotomy** is indicated for **acute compartment syndrome**, which typically presents with severe pain out of proportion to injury, pain on passive stretch, paresthesia, and tense compartments.
- While the patient has swelling and tenderness, the weak pulses are concerning, but the overall picture does not definitively point to compartment syndrome needing immediate fasciotomy without further diagnostic workup.
*Start intravenous heparin therapy immediately*
- Though DVT is suspected, **heparin therapy should not be initiated empirically without definitive diagnostic confirmation** due to the risk of bleeding complications.
- A **venous ultrasound is crucial to confirm the diagnosis** before starting anticoagulation.
*Make a diagnosis of deep vein thrombosis based on history and physical*
- While the clinical picture is highly suggestive of DVT, **clinical diagnosis alone is not sufficiently accurate** to initiate potentially risky treatments like anticoagulation.
- **Objective diagnostic testing (like ultrasound)** is essential to confirm the presence of a DVT.
*Perform intravenous venography within 24 hours*
- **Intravenous venography** is considered the **gold standard** for diagnosing DVT, but it is an **invasive procedure** with risks (e.g., contrast nephropathy, allergic reactions, radiation exposure).
- It is **rarely used as a first-line diagnostic test** and is usually reserved for cases where ultrasound results are inconclusive or discordant with clinical suspicion.
Vascular trauma management US Medical PG Question 2: A 74-year-old male is brought to the emergency department 1 hour after he fell from the top of the staircase at home. He reports pain in his neck as well as weakness of his upper extremities. He is alert and immobilized in a cervical collar. He has hypertension treated with hydrochlorothiazide. His pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/70 mmHg. Examination shows bruising and midline cervical tenderness. Neurologic examination shows diminished strength and sensation to pain and temperature in the upper extremities, particularly in the hands. Upper extremity deep tendon reflexes are absent. Strength, sensation, and reflexes in the lower extremities are intact. Anal sensation and tone are present. Babinski's sign is absent bilaterally. Which of the following is most likely to confirm the cause of this patient's neurologic examination findings?
- A. CT angiography of the neck
- B. MRI of the cervical spine without contrast (Correct Answer)
- C. X-ray of the cervical spine
- D. CT of the cervical spine with contrast
- E. Cervical myelography
Vascular trauma management Explanation: ***MRI of the cervical spine without contrast***
- This patient presents with symptoms consistent with **central cord syndrome**, characterized by greater weakness in the upper extremities than the lower extremities, often following a hyperextension injury in older adults with pre-existing cervical spondylosis. **MRI is the gold standard for visualizing soft tissue injuries**, including spinal cord compression, edema, or hemorrhage, which are typical causes of central cord syndrome.
- Given the primary concern for spinal cord injury and the detailed neurological deficits indicating specific cord involvement, **MRI** offers the best resolution for evaluating the extent of cord damage, disc herniation, ligamentous injury, and pre-existing degenerative changes.
*CT angiography of the neck*
- **CT angiography** primarily evaluates the **vascular structures** of the neck (e.g., carotid and vertebral arteries) for dissection, stenosis, or occlusion.
- While vascular injury could occur in trauma, the patient's neurological findings (disproportionate upper extremity weakness, pain and temperature sensation loss) point more directly to **spinal cord pathology** rather than isolated vascular compromise as the primary cause.
*X-ray of the cervical spine*
- **X-rays** are useful for initial screening of **bony fractures** and significant dislocations but offer limited information about soft tissues, such as the spinal cord, ligaments, or intervertebral discs.
- They cannot adequately visualize the spinal cord damage responsible for the patient's specific neurological deficits, making it insufficient for confirming the cause of central cord syndrome.
*CT of the cervical spine with contrast*
- **CT scans** excel at visualizing **bony structures** and acute fractures, but even with contrast, they provide less detail of the **spinal cord parenchyma** and soft tissue ligaments compared to MRI.
- **Contrast** is typically used to highlight vascular structures, inflammatory processes, or tumors, which are not the primary diagnostic concerns suggested by this patient's acute post-traumatic presentation of central cord syndrome.
*Cervical myelography*
- **Myelography** involves injecting contrast into the subarachnoid space, followed by X-ray or CT imaging, to outline the spinal cord and nerve roots.
- While it can identify **spinal cord compression**, it is an **invasive procedure** with risks (e.g., headache, seizures) and has largely been replaced by the non-invasive and superior soft tissue imaging capabilities of MRI, especially in acute trauma.
Vascular trauma management US Medical PG Question 3: A 29-year-old man is brought to the emergency department 20 minutes after being stabbed in the left thigh. His pulse is 110/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Examination shows a 2-cm wound overlying a pulsatile mass on the left anterior thigh, 4 cm below the inguinal crease. A thrill is palpated, and a bruit is heard over this area. Peripheral pulses are normal bilaterally. The patient is at greatest risk for which of the following?
- A. Erectile dysfunction
- B. High-output cardiac failure (Correct Answer)
- C. Pudendal nerve compression
- D. Femoral head necrosis
- E. Iliac artery aneurysm
Vascular trauma management Explanation: **High-output cardiac failure**
- The pulsatile mass, thrill, and bruit over the stab wound indicate an **arteriovenous (AV) fistula**, where arterial blood shunts directly into a vein.
- A large AV fistula significantly reduces systemic vascular resistance, increasing venous return and cardiac output, which can lead to **high-output cardiac failure** over time.
*Erectile dysfunction*
- While a vascular injury could, in rare cases, affect **penile blood supply**, the described injury in the anterior thigh (likely involving the femoral artery/vein) is not typically associated with erectile dysfunction as a primary or immediate complication.
- Erectile dysfunction is often related to injuries to the **internal pudendal arteries** or nerve damage (e.g., sacral plexus), which are not directly implicated by a femoral AV fistula.
*Pudendal nerve compression*
- A stab wound in the **anterior thigh** is anatomically distant from the pudendal nerve, which is located more medially and posteriorly in the pelvis and perineum.
- Pudendal nerve compression typically causes **perineal pain** or numbness, not symptoms related to a femoral AV fistula.
*Femoral head necrosis*
- **Avascular necrosis of the femoral head** is usually caused by disruption of the blood supply via the medial femoral circumflex artery, often due to trauma like hip dislocation or chronic corticosteroid use.
- The described injury is to the **superficial femoral vessels** and is not directly upstream of the typical blood supply to the femoral head sufficient to cause necrosis.
*Iliac artery aneurysm*
- An aneurysm is a **localized dilation** of an artery, usually due to weakening of the vessel wall, and it's distinct from an AV fistula which involves a direct connection between an artery and a vein.
- While the iliac artery feeds into the femoral artery, the pulsatile mass and bruit directly at the wound site are characteristic of a **traumatic AV fistula**, not an iliac artery aneurysm.
Vascular trauma management US Medical PG Question 4: A 20-year-old woman is brought to the emergency department because of severe muscle soreness, nausea, and darkened urine for 2 days. The patient is on the college track team and has been training intensively for an upcoming event. One month ago, she had a urinary tract infection and was treated with nitrofurantoin. She appears healthy. Her temperature is 37°C (98.6°F), pulse is 64/min, and blood pressure is 110/70 mm Hg. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and non-tender. There is diffuse muscle tenderness over the arms, legs, and back. Laboratory studies show:
Hemoglobin 12.8 g/dL
Leukocyte count 7,000/mm3
Platelet count 265,000/mm3
Serum
Creatine kinase 22,000 U/L
Lactate dehydrogenase 380 U/L
Urine
Blood 3+
Protein 1+
RBC negative
WBC 1–2/hpf
This patient is at increased risk for which of the following complications?
- A. Myocarditis
- B. Metabolic alkalosis
- C. Compartment syndrome
- D. Acute kidney injury (Correct Answer)
- E. Hemolytic anemia
Vascular trauma management Explanation: ***Acute kidney injury***
- The patient's elevated **creatine kinase (CK)** of 22,000 U/L, muscle soreness, and dark urine (positive for blood but negative for red blood cells) are all indicative of **rhabdomyolysis**.
- **Rhabdomyolysis** releases large amounts of myoglobin, which is nephrotoxic and can precipitate in the renal tubules, leading to **acute tubular necrosis** and subsequent acute kidney injury.
*Myocarditis*
- While CK elevations can be seen in myocarditis, this patient's presentation is dominated by **skeletal muscle symptoms** and a history of intense exercise.
- There are no specific cardiac symptoms or signs (e.g., chest pain, arrhythmias) to suggest myocardial involvement.
*Metabolic alkalosis*
- Rhabdomyolysis typically causes **metabolic acidosis** due to the release of cellular contents, including phosphate and sulfate.
- There is no clinical or lab evidence (e.g., vomiting, diuretic use) to suggest metabolic alkalosis.
*Compartment syndrome*
- **Compartment syndrome** involves increased pressure within a muscle compartment, leading to pain, pallor, paresthesia, pulselessness, and paralysis.
- While rhabdomyolysis can occasionally lead to severe swelling that causes compartment syndrome, the diffuse muscle tenderness and absence of focal limb findings make it less likely as the primary direct complication.
*Hemolytic anemia*
- Though the urine is positive for blood and negative for RBCs, this is characteristic of **myoglobinuria**, not hemoglobinuria, which would indicate hemolytic anemia.
- The patient's **hemoglobin** is normal (12.8 g/dL), and there are no other signs of hemolysis (e.g., jaundice, reticulocytosis).
Vascular trauma management US Medical PG Question 5: A 38-year-old man is brought to the emergency department 35 minutes after he sustained a gunshot wound to the right thigh. He has type 1 diabetes mellitus. On arrival, his pulse is 112/min, respirations are 20/min, and blood pressure is 115/69 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. There is an entrance wound on the anteromedial surface of the right thigh 2 cm below the inguinal ligament. There is no bruit or thrill. There is no exit wound. The pedal pulse is diminished on the right side compared to the left. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hematocrit 46%
Serum
Urea nitrogen 24 mg/dL
Glucose 160 mg/dL
Creatinine 3.1 mg/dL
Which of the following is the most appropriate next step in management?
- A. Digital subtraction angiography
- B. Wound cleaning and tetanus toxoid
- C. CT angiography
- D. Duplex ultrasonography (Correct Answer)
- E. Fasciotomy
Vascular trauma management Explanation: ***Duplex ultrasonography***
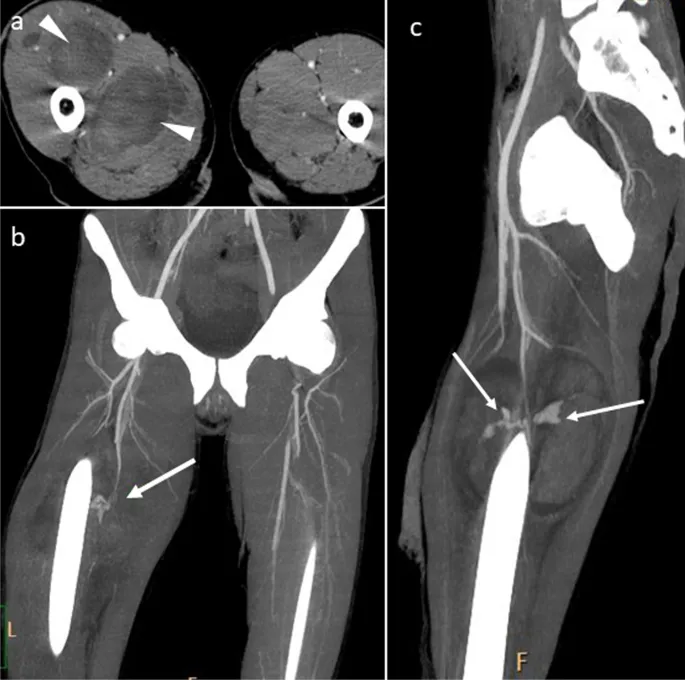
- The patient has suffered a **gunshot wound** to the thigh with a **diminished pedal pulse**, indicating potential **vascular injury** (a "soft sign" requiring imaging).
- Given his **significantly elevated creatinine (3.1 mg/dL)** and **type 1 diabetes mellitus**, imaging studies requiring **IV iodinated contrast** carry substantial risk for **contrast-induced nephropathy** and further renal deterioration.
- **Duplex ultrasonography** is a **non-invasive, contrast-free method** to assess vascular flow and identify injuries like **arterial dissection**, **thrombosis**, or **pseudoaneurysm**. While operator-dependent, it is the most appropriate initial diagnostic step in this hemodynamically stable patient with significant renal impairment.
- This allows vascular assessment while **minimizing nephrotoxic risk** in a patient with pre-existing renal dysfunction.
*CT angiography*
- **CT angiography** is the **gold standard** for evaluating penetrating extremity trauma with soft signs of vascular injury in most cases, offering rapid and highly accurate vascular imaging.
- However, it requires administration of **intravenous iodinated contrast**, which poses significant risk for **contrast-induced nephropathy** in this patient with **baseline creatinine of 3.1 mg/dL** and **diabetes mellitus**.
- While CTA would typically be preferred in trauma settings, the severe renal impairment makes duplex ultrasonography the safer initial choice in this stable patient.
*Digital subtraction angiography*
- This is an **invasive angiographic technique** that uses **iodinated contrast** and carries even higher contrast load than CTA, posing substantial risk for **contrast-induced nephropathy** given the patient's **elevated creatinine**.
- While it offers high resolution and therapeutic capability, the risks associated with contrast and invasive arterial access outweigh its benefits for initial assessment in this scenario.
- Reserved for cases where intervention is anticipated or non-invasive imaging is inconclusive.
*Wound cleaning and tetanus toxoid*
- These are essential components of wound care for any penetrating injury but do not address the immediate concern of **potential vascular injury** causing the diminished pedal pulse.
- Prioritizing definitive diagnosis of vascular compromise is critical before focusing solely on local wound management, as a missed arterial injury could lead to limb loss.
*Fasciotomy*
- **Fasciotomy** is a surgical procedure to relieve **compartment syndrome**, which can develop secondary to vascular injury, reperfusion, or significant soft tissue trauma.
- While compartment syndrome is a risk with this injury, there is no immediate clinical evidence of it (no severe pain out of proportion to exam, no tense compartments documented).
- Diagnosis of the vascular injury should be established first, as fasciotomy may be needed later if ischemia is prolonged or after revascularization.
Vascular trauma management US Medical PG Question 6: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
Vascular trauma management Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
Vascular trauma management US Medical PG Question 7: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
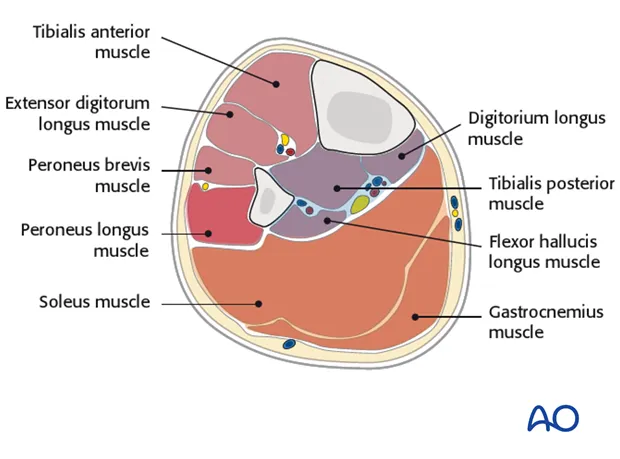
Vascular trauma management Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Vascular trauma management US Medical PG Question 8: A 22-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was the unrestrained driver. After extrication, he had severe neck pain and was unable to move his arms and legs. On arrival, he is lethargic and cannot provide a history. Hospital records show that eight months ago, he underwent an open reduction and internal fixation of the right humerus. His neck is immobilized in a cervical collar. Intravenous fluids are being administered. His pulse is 64/min, respirations are 8/min and irregular, and blood pressure is 104/64 mm Hg. Examination shows multiple bruises over the chest, abdomen, and extremities. There is flaccid paralysis and absent reflexes in all extremities. Sensory examination shows decreased sensation below the shoulders. Cardiopulmonary examination shows no abnormalities. The abdomen is soft. There is swelling of the right ankle and right knee. Squeezing of the glans penis does not produce anal sphincter contraction. A focused assessment with sonography for trauma shows no abnormalities. He is intubated and mechanically ventilated. Which of the following is the most appropriate next step in management?
- A. Cervical x-ray
- B. CT of the head
- C. Intravenous dexamethasone therapy
- D. MRI of the spine (Correct Answer)
- E. Placement of Foley catheter
Vascular trauma management Explanation: **MRI of the spine**
- The patient presents with clear signs of a **spinal cord injury** (flaccid paralysis, absent reflexes, decreased sensation below the shoulders, severe neck pain after trauma). **MRI** is the most sensitive and specific imaging modality to visualize soft tissue injuries, including the spinal cord, ligaments, and disc herniations, which are crucial for diagnosing and guiding treatment for a spinal cord injury.
- Given the patient's **hemodynamic stability** after initial resuscitation and intubation, and the suspicion of spinal cord injury, a thorough evaluation with MRI is the next appropriate step to delineate the extent and location of the injury.
*Cervical x-ray*
- While cervical X-rays are often performed in trauma cases, they have **limited sensitivity** for detecting all spinal injuries, especially soft tissue damage, ligamentous injuries, or non-displaced fractures.
- In a patient with clear neurological deficits suggesting spinal cord involvement, X-rays alone are **insufficient** for a definitive diagnosis and treatment planning.
*CT of the head*
- A CT scan of the head would be appropriate if there were signs of a **head injury**, such as focal neurological deficits suggestive of intracranial pathology, or a change in mental status not fully explained by other injuries.
- In this case, the predominant neurological signs point to a **spinal cord injury** rather than a primary head injury, making head CT a lower priority at this stage.
*Intravenous dexamethasone therapy*
- The use of high-dose corticosteroids like dexamethasone for acute spinal cord injury is **controversial** and its routine use is **not recommended** by current guidelines due to a lack of clear benefit and potential for harm.
- Imaging to characterize the injury is a more urgent and appropriate step before considering any pharmacological interventions for spinal cord protection.
*Placement of Foley catheter*
- While a **Foley catheter** will likely be needed for this patient to manage neurogenic bladder dysfunction that often accompanies spinal cord injury, it is a supportive measure.
- It does not address the immediate diagnostic need to characterize the spinal cord injury, which is paramount for guiding surgical or medical management and preventing further damage.
Vascular trauma management US Medical PG Question 9: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Vascular trauma management Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Vascular trauma management US Medical PG Question 10: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Vascular trauma management Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
More Vascular trauma management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.