Peripheral arterial disease diagnosis and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peripheral arterial disease diagnosis and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peripheral arterial disease diagnosis and management US Medical PG Question 1: A 67-year-old man comes to the office due to pain in the lower part of his calves on his afternoon walk to get the mail. The pain is relieved by rest. It started slowly about 6 months ago and has become more painful over time. He has a history of hypertension, hyperlipidemia, diabetes mellitus, and a 20-pack-year smoking history. Medications include hydrochlorothiazide, atorvastatin, metformin, and a multivitamin that he takes daily. The patient quit smoking 2 years ago and only drinks socially. Today, his blood pressure is 145/90 mm Hg, pulse is 75/min, respiratory rate is 17/min, and temperature is 37.6°C (99.6°F). On physical exam, he appears mildly obese and healthy. His heart has a regular rate and rhythm, and his lungs are clear to auscultation bilaterally. Examination of the legs shows atrophic changes and diminished pedal pulses. A measure of his ankle brachial index (ABI) is 0.89. Which of the following is the most appropriate initial treatment?
- A. A recommendation to walk more
- B. Metoprolol
- C. A recommendation to perform pedal pumping exercises
- D. A referral to a supervised exercise program (Correct Answer)
- E. Enoxaparin
Peripheral arterial disease diagnosis and management Explanation: ***A referral to a supervised exercise program***
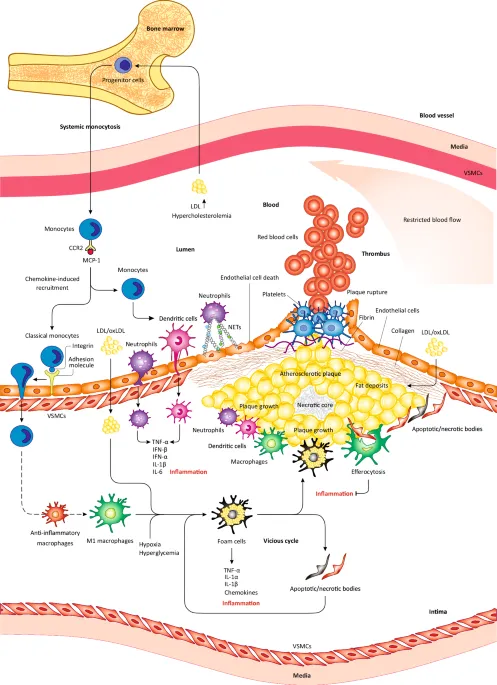
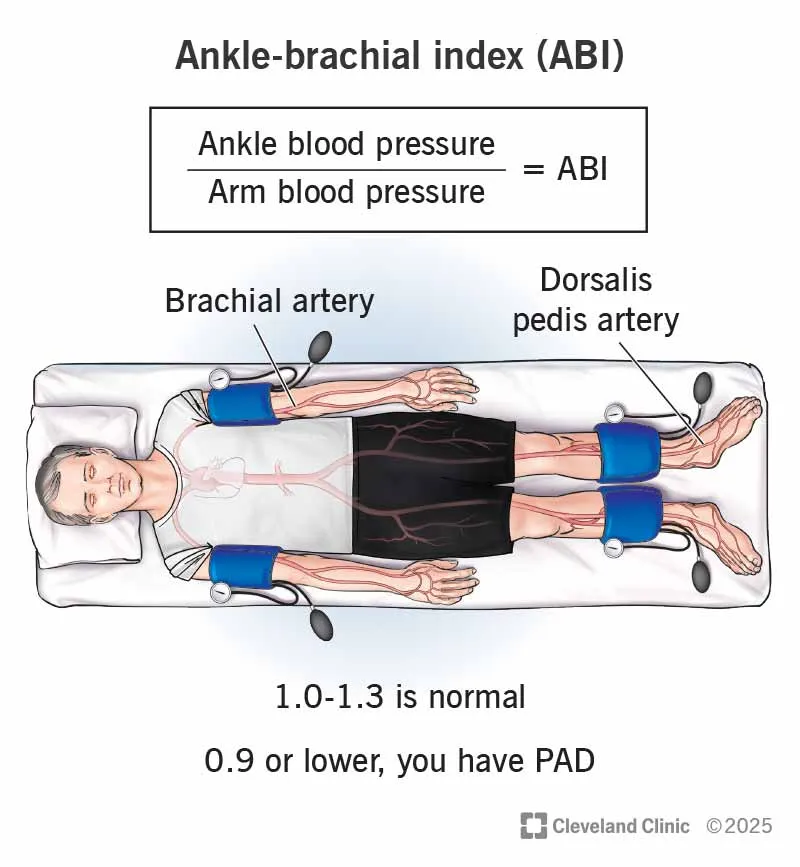
- The patient's symptoms (claudication, relief with rest), risk factors (**hypertension, hyperlipidemia, diabetes, smoking history**), physical exam findings (**atrophic changes, diminished pedal pulses**), and **ABI of 0.89** (indicating mild peripheral artery disease) all point to **peripheral arterial disease (PAD)**.
- A **supervised exercise program**, particularly walking, is the most effective initial non-pharmacological treatment for improving walking distance and quality of life in patients with claudication due to PAD.
*A recommendation to walk more*
- While walking is beneficial, simply recommending "walking more" without specific guidance or supervision is less effective than a structured program.
- An unsupervised general walking recommendation may not optimize the **duration**, **intensity**, or **frequency** needed for therapeutic benefit in PAD.
*Metoprolol*
- **Beta-blockers** like metoprolol can worsen claudication symptoms by decreasing blood flow to the extremities, especially in patients with PAD.
- They are generally **contraindicated** or used with caution in PAD patients experiencing claudication.
*A recommendation to perform pedal pumping exercises*
- **Pedal pumping exercises** are primarily used to prevent **venous stasis** and **deep vein thrombosis**, typically post-surgery or during prolonged immobility.
- They do not address the underlying arterial insufficiency causing claudication and are not an effective treatment for PAD.
*Enoxaparin*
- **Enoxaparin** is a low molecular weight heparin, an **anticoagulant** used for conditions like deep vein thrombosis or acute coronary syndromes.
- It is not indicated for the chronic management of stable claudication in peripheral artery disease, where antiplatelet therapy is generally preferred if medication is needed.
Peripheral arterial disease diagnosis and management US Medical PG Question 2: A 75-year-old Caucasian man presents to the emergency department with abdominal pain. The patient states he was at home eating dinner when he began to experience severe abdominal pain. The patient has a past medical history of diabetes, hypertension, and atherosclerosis. He lives at home alone, smokes cigarettes, and drinks 1 to 2 alcoholic drinks per day. The patient is given IV morphine and an ultrasound is obtained demonstrating a dilated abdominal aorta. The patient states that his father died of a similar finding and is concerned about his prognosis. Which of the following is the greatest risk factor for this patient's presentation?
- A. Male gender and age
- B. Caucasian race
- C. Cigarette smoking (Correct Answer)
- D. Family history
- E. Atherosclerosis
Peripheral arterial disease diagnosis and management Explanation: ***Cigarette smoking***
- **Cigarette smoking** is the most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)**, directly contributing to vascular inflammation and degradation.
- The patient's history of smoking suggests a strong causal link to his current presentation of a dilated aorta, which is highly indicative of an AAA.
*Male gender and age*
- While **male gender** and **advanced age (over 65)** are significant demographic risk factors for AAA, they are considered non-modifiable and less impactful than smoking in terms of risk magnitude.
- These factors increase predisposition but do not exert the same direct, damaging effect on the arterial wall as chronic smoking.
*Caucasian race*
- **Caucasian race** is a known demographic risk factor for AAA, with higher prevalence rates compared to other ethnic groups.
- However, this is a non-modifiable genetic predisposition and contributes less to the overall risk than modifiable lifestyle factors like smoking.
*Family history*
- A **family history** of AAA, as suggested by the patient's father having a similar condition, increases an individual's susceptibility.
- This is a significant non-modifiable risk factor, indicating genetic predisposition, but its overall impact on aneurysm formation and progression is typically less than that of active smoking.
*Atherosclerosis*
- **Atherosclerosis** is a strong associated condition with AAA, as both share common risk factors and pathology related to arterial wall degeneration.
- While atherosclerosis contributes to the overall vascular compromise, smoking specifically has a more direct and potent effect on promoting aneurysm formation and rupture independently.
Peripheral arterial disease diagnosis and management US Medical PG Question 3: A 53-year-old Asian woman comes to the physician because of a 2-month history of severe pain in her right leg while walking. She used to be able to walk a half-mile (800-m) to the grocery store but has been unable to walk 200 meters without stopping because of the pain over the past month. She can continue to walk after a break of around 5 minutes. She has hypertension, atrial fibrillation, and type 2 diabetes mellitus. She has smoked one pack of cigarettes daily for the past 32 years. Current medications include metformin, enalapril, aspirin, and warfarin. Vital signs are within normal limits. Examination shows an irregularly irregular pulse. The right lower extremity is cooler than the left lower extremity. The skin over the right leg appears shiny and dry. Femoral pulses are palpated bilaterally; pedal pulses are diminished on the right side. Which of the following is the most appropriate next step in management?
- A. MRI spine screening
- B. Duplex ultrasonography
- C. Ankle-brachial index (Correct Answer)
- D. Nerve conduction studies
- E. Biopsy of tibial artery
Peripheral arterial disease diagnosis and management Explanation: ***Ankle-brachial index***
- The patient's symptoms of **intermittent claudication** (leg pain with exertion relieved by rest) and risk factors (smoking, diabetes, atrial fibrillation, hypertension) are highly suggestive of **peripheral artery disease (PAD)**. The **ankle-brachial index (ABI)** is the most appropriate initial diagnostic step as it is a quick, non-invasive, and reliable test to screen for PAD by comparing blood pressure in the ankles to blood pressure in the arms.
- A **diminished pedal pulse** on the right side and **cooler, shiny, dry skin** further support the suspicion of PAD, making ABI crucial for confirming the diagnosis and assessing its severity.
*MRI spine screening*
- While spinal pathology can cause leg pain, symptoms like **neurogenic claudication** typically improve with leaning forward or sitting and are not consistently relieved by standing still. The patient's pain relief with rest after walking points away from spinal stenosis.
- The patient's specific peripheral signs like a **cooler leg**, **diminished pedal pulses**, and **trophic changes** are not typical findings for spinal compression.
*Duplex ultrasonography*
- **Duplex ultrasonography** is a more advanced imaging technique used to visualize the blood vessels and assess blood flow, typically performed *after* an abnormal ABI confirms the presence of PAD.
- It helps in **localizing stenoses** and assessing their severity, but it is not the primary diagnostic screening tool in the initial evaluation of suspected PAD.
*Nerve conduction studies*
- **Nerve conduction studies (NCS)** are used to diagnose neuropathies. While diabetes is a risk factor for neuropathy, the patient's symptoms are classic for **vascular claudication** (pain with exertion, relieved by rest), rather than neuropathic pain, which is often described as burning, tingling, or numbing and does not typically resolve promptly with rest.
- The physical exam findings of a **cool leg** and **diminished pulses** are not consistent with a primary neurological problem.
*Biopsy of tibial artery*
- A **biopsy of the tibial artery** is an invasive procedure generally reserved for specific types of vasculitis (e.g., giant cell arteritis, polyarteritis nodosa) when other less invasive diagnostics have been inconclusive or raised suspicion for these conditions.
- It is not indicated for the initial workup of suspected **atherosclerotic peripheral artery disease**, which is the most likely diagnosis given the patient's risk factors and symptoms.
Peripheral arterial disease diagnosis and management US Medical PG Question 4: A 73-year-old man comes to the physician because of worsening bilateral lower extremity pain for the past 8 months. The pain begins after walking one to two blocks and radiates bilaterally down the buttocks with cramping and tingling. He reports that the pain is worse while walking downhill and is relieved by sitting and leaning forward. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. He had a myocardial infarction at the age of 55 years and an abdominal aortic aneurysm repair at the age of 60 years. He has smoked one pack of cigarettes daily for the past 30 years. He does not drink alcohol or use illicit drugs. His current medications include sitagliptin, metformin, atorvastatin, metoprolol succinate, amlodipine, and hydrochlorothiazide. His temperature is 37.5°C (99.5°F), pulse is 82/min, respirations are 17/min, and blood pressure is 150/87 mm Hg. Examination shows full muscle strength. Sensation is reduced bilaterally in the feet and toes. Straight leg raise is negative. X-ray of the spine shows degenerative changes. Which of the following is the most appropriate next step in diagnosis?
- A. MRI scan of the spine (Correct Answer)
- B. Measurement of the ankle brachial index
- C. Measurement of serum creatine kinase
- D. Polysomnography
- E. Measurement of HLA-B27 antigen
Peripheral arterial disease diagnosis and management Explanation: ***MRI scan of the spine***
- The patient's symptoms of **neurogenic claudication** (pain worse with walking downhill, relieved by sitting and leaning forward) are highly suggestive of **spinal stenosis**.
- An MRI provides detailed imaging of the spinal canal, nerve roots, and surrounding soft tissues, which is essential for confirming **spinal stenosis** and identifying the precise location and extent of nerve compression.
*Measurement of the ankle brachial index*
- An ABI measures peripheral arterial disease (PAD), which can cause **vascular claudication** (pain worse with uphill walking, relieved by standing still).
- The patient's symptoms (pain worse downhill, relieved by leaning forward) are not typical for **vascular claudication** despite his vascular risk factors.
*Measurement of serum creatine kinase*
- Creatine kinase is an enzyme released from damaged muscle, used to diagnose **myopathies** or significant muscle injury.
- The clinical presentation is more consistent with a **neurological compression** than a primary muscle disorder, and the patient has full muscle strength.
*Polysomnography*
- Polysomnography is a sleep study used to diagnose sleep disorders such as **sleep apnea** or **narcolepsy**.
- It is unrelated to lower extremity pain and claudication symptoms.
*Measurement of HLA-B27 antigen*
- HLA-B27 is a genetic marker associated with **spondyloarthropathies** like ankylosing spondylitis, reactive arthritis, and psoriatic arthritis.
- The patient's age of onset and specific symptoms of neurogenic claudication are not characteristic of inflammatory rheumatologic conditions.
Peripheral arterial disease diagnosis and management US Medical PG Question 5: A 65-year-old man comes to his primary care physician with a 6-month history of bilateral calf pain. The pain usually occurs after walking his dog a few blocks and is more severe on the right side. He has coronary artery disease, essential hypertension, and type 2 diabetes mellitus. He has smoked two packs of cigarettes daily for 43 years and drinks two alcoholic beverages a day. Current medications include metformin, lisinopril, and aspirin. He is 183 cm (5 ft 11 in) tall and weighs 113 kg (250 lb); BMI is 34.9 kg/m2. His temperature is 37°C (98.6°F), pulse is 84/min, and blood pressure is 129/72 mm Hg. Cardiac examination shows a gallop without murmurs. The legs have shiny skin with reduced hair below the knee. Femoral and popliteal pulses are palpable bilaterally. Dorsal pedal pulses are 1+ on the left and absent on the right. Ankle-brachial index (ABI) is performed in the office. ABI is 0.5 in the right leg, and 0.6 in the left leg. Which of the following is the most appropriate initial step in management?
- A. Propranolol therapy
- B. Graded exercise therapy (Correct Answer)
- C. Vascular bypass surgery
- D. Spinal cord stimulation
- E. Percutaneous transluminal angioplasty with stenting
Peripheral arterial disease diagnosis and management Explanation: ***Graded exercise therapy***
- **Graded exercise therapy** is the recommended initial treatment for patients with **intermittent claudication** due to peripheral artery disease (PAD). It improves walking distance and reduces symptoms by promoting collateral circulation and endothelial function.
- This patient's symptoms (bilateral calf pain with exertion, shiny skin, reduced hair, absent dorsal pedal pulse on the right, and low ABI scores) are classic for **PAD with claudication**.
*Propranolol therapy*
- **Propranolol** is a non-selective beta-blocker that can worsen claudication symptoms by inhibiting beta-2 mediated vasodilation in peripheral arteries.
- While beta-blockers may be indicated for some cardiac conditions, they are generally avoided or used cautiously in PAD due to their potential to exacerbate peripheral vasoconstriction.
*Vascular bypass surgery*
- **Vascular bypass surgery** is typically reserved for patients with **severe, limb-threatening ischemia** (critical limb ischemia) or those with claudication that is refractory to conservative management.
- This patient's symptoms, while significant, are consistent with intermittent claudication, which is usually managed initially with lifestyle modifications and exercise.
*Spinal cord stimulation*
- **Spinal cord stimulation** is a treatment option primarily for **refractory chronic neuropathic pain** or **critical limb ischemia** not amenable to revascularization, aiming to reduce pain and potentially improve wound healing.
- It is not an initial treatment for intermittent claudication and doesn't address the underlying vascular obstruction causing claudication.
*Percutaneous transluminal angioplasty with stenting*
- **Percutaneous transluminal angioplasty with stenting** is a revascularization procedure considered when conservative therapies fail to improve claudication or for critical limb ischemia.
- It is not the initial step in management for intermittent claudication. **Lifestyle modifications** and supervised exercise are the first-line treatments.
Peripheral arterial disease diagnosis and management US Medical PG Question 6: Two days after undergoing emergency cardiac catherization for myocardial infarction, a 68-year-old woman has pain in her toes. During the intervention, she was found to have an occluded left anterior descending artery and 3 stents were placed. She has hypertension, hypercholesterolemia, and coronary artery disease. Prior to admission, her medications were metoprolol, enalapril, atorvastatin, and aspirin. Her temperature is 37.3°C (99.1°F), pulse is 93/min, and blood pressure is 115/78 mm Hg. Examination shows discoloration of the toes of both feet. A photograph of the right foot is shown. The lesions are cool and tender to palpation. The rest of the skin on the feet is warm; femoral and pedal pulses are palpable bilaterally. This patient is at increased risk for which of the following conditions?
- A. Acute kidney injury (Correct Answer)
- B. Migratory thrombophlebitis
- C. Basophilia
- D. Permanent flexion contracture
- E. Lipodermatosclerosis
Peripheral arterial disease diagnosis and management Explanation: ***Acute kidney injury***
- This patient's presentation of painful, discolored, cool toes with palpable pulses (suggesting microembolism rather than large vessel occlusion) following cardiac catheterization is highly suggestive of **cholesterol atheroembolism**. This condition commonly leads to **acute kidney injury** as cholesterol crystals dislodge from atheromatous plaques and embolize to renal arteries.
- The risk of acute kidney injury is significant in cholesterol atheroembolism due to widespread microvascular occlusion in the kidneys, leading to **ischemic damage** and **renal dysfunction**.
*Migratory thrombophlebitis*
- **Migratory thrombophlebitis** (Trousseau's sign) is characterized by recurrent, migratory episodes of superficial venous thrombosis, often associated with underlying malignancy.
- It would present with **palpable, tender, cord-like veins** typically in the extremities, rather than multifocal discoloration of the toes.
*Basophilia*
- While **eosinophilia** is often associated with cholesterol atheroembolism due to the inflammatory response to cholesterol crystals, **basophilia** (an increase in basophils) is not a typical finding or complication.
- Basophilia can be seen in myeloproliferative disorders or allergic reactions, which are not suggested by this clinical picture.
*Permanent flexion contracture*
- A permanent flexion contracture is a **fixed deformation** of a joint, preventing full extension. It is typically caused by chronic inflammation, muscle imbalances, or prolonged immobilization.
- This is a long-term orthopedic complication that would not develop acutely **2 days after a cardiac catheterization** or be directly related to microembolism.
*Lipodermatosclerosis*
- **Lipodermatosclerosis** is a localized chronic inflammation and thickening of the skin and subcutaneous tissue, typically in the lower legs, associated with **chronic venous insufficiency**.
- It presents with **brawny edema**, hyperpigmentation, and inverted champagne bottle appearance of the leg, which is distinctly different from the acute painful toe discoloration seen here.
Peripheral arterial disease diagnosis and management US Medical PG Question 7: A 58-year-old man comes to the physician because of a 3-month history of intermittent pain in his right calf that occurs after walking up more than 2 flights of stairs. He reports that the pain is associated with a tingling sensation and lasts for about 10 minutes. He is otherwise healthy. He has smoked 2 packs of cigarettes daily for 30 years and drinks 1 alcoholic beverage daily. He currently takes no medications. His pulse is 78/min, and blood pressure is 180/110 mm Hg. Physical examination shows yellow plaques below the lower eyelids bilaterally, loss of hair on the distal third of the right leg, and brittle toenails on the right foot. Femoral pulses are palpable bilaterally; right popliteal and pedal pulses are absent. Which of the following is the most appropriate management to prevent future morbidity and mortality of this patient's condition?
- A. Clopidogrel therapy (Correct Answer)
- B. Percutaneous transluminal angioplasty
- C. Cilostazol therapy
- D. Graded exercise therapy
- E. Pentoxifylline therapy
Peripheral arterial disease diagnosis and management Explanation: ***Clopidogrel therapy***
- **Antiplatelet therapy** with clopidogrel (or aspirin) is crucial for **preventing future morbidity and mortality** in PAD patients by reducing the risk of **myocardial infarction**, stroke, and cardiovascular death.
- PAD is a manifestation of systemic atherosclerosis, and these patients have significantly elevated cardiovascular risk. Antiplatelet therapy addresses this systemic risk and is a cornerstone of medical management.
- Current guidelines (ACC/AHA) strongly recommend antiplatelet therapy for all patients with symptomatic PAD to reduce adverse cardiovascular events.
*Graded exercise therapy*
- **Graded exercise therapy** is highly effective for improving walking distance and reducing claudication symptoms by promoting collateral circulation and improving endothelial function.
- While exercise is essential for symptom management and quality of life, it is **not the primary intervention for preventing mortality** in PAD patients, which is what this question specifically asks about.
- Exercise should be recommended alongside antiplatelet therapy and risk factor modification.
*Pentoxifylline therapy*
- **Pentoxifylline** may improve red blood cell flexibility and microcirculation, but it has shown limited efficacy for symptom relief and **no proven benefit for reducing cardiovascular mortality**.
- Its use is generally reserved for patients who cannot tolerate other treatments.
*Percutaneous transluminal angioplasty*
- **Revascularization** (PTA or surgical bypass) is typically reserved for patients with severe, lifestyle-limiting claudication unresponsive to medical therapy, or for critical limb ischemia.
- This patient has intermittent claudication with moderate symptoms, making conservative medical management more appropriate initially.
- Revascularization improves symptoms but does not reduce mortality compared to medical therapy alone.
*Cilostazol therapy*
- **Cilostazol** is a phosphodiesterase-3 inhibitor that improves walking distance and claudication symptoms through vasodilation and antiplatelet effects.
- While effective for symptomatic relief, it does **not reduce cardiovascular mortality** and has a contraindication in heart failure patients.
- It is used as an adjunct for symptom management, not as primary prevention of morbidity and mortality.
Peripheral arterial disease diagnosis and management US Medical PG Question 8: A 67-year-old man presents with pain in both legs. He says the pain is intermittent in nature and has been present for approximately 6 months. The pain increases with walking, especially downhill, and prolonged standing. It is relieved by lying down and leaning forward. Past medical history is significant for type 2 diabetes mellitus, hypercholesterolemia, and osteoarthritis. The patient reports a 56-pack-year history but denies any alcohol or recreational drug use. His vital signs include: blood pressure 142/88 mm Hg, pulse 88/min, respiratory rate 14/min, temperature 37°C (98.6°F). On physical examination, the patient is alert and oriented. Muscle strength is 5/5 in his upper and lower extremities bilaterally. Babinski and Romberg tests are negative. Pulses measure 2+ in upper and lower extremities bilaterally. Which of the following is the next best step in the management of this patient?
- A. MRI of the spine (Correct Answer)
- B. CT angiography of the lower extremities
- C. Ankle-brachial index
- D. Cilostazol
- E. Epidural corticosteroid injection
Peripheral arterial disease diagnosis and management Explanation: ***MRI of the spine***
- The patient's symptoms of **intermittent leg pain worsened by walking (especially downhill) and prolonged standing**, and **relieved by lying down and leaning forward**, are highly classic for **neurogenic claudication** due to **lumbar spinal stenosis**.
- An **MRI of the spine** is the *gold standard* for diagnosing spinal stenosis, clearly visualizing nerve root compression and the degree of canal narrowing.
*CT angiography of the lower extremities*
- This imaging is used to assess **peripheral artery disease** (PAD) but the patient's symptoms are inconsistent with vascular claudication.
- **Vascular claudication** typically improves with rest, not with specific postures like leaning forward.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is a non-invasive test to screen for **peripheral artery disease (PAD)**.
- While the patient has risk factors for PAD (diabetes, hypercholesterolemia, smoking), his symptoms are classic for neurogenic claudication, and his **2+ pulses** in the lower extremities make PAD less likely.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to treat symptoms of **intermittent claudication** caused by **peripheral artery disease (PAD)**.
- Since the patient's symptoms are more consistent with neurogenic claudication rather than vascular claudication, cilostazol would not be the appropriate initial step.
*Epidural corticosteroid injection*
- An **epidural corticosteroid injection** is a treatment option for symptomatic spinal stenosis but is not the *initial diagnostic step*.
- Diagnosis with an **MRI** is necessary before considering targeted therapeutic interventions like injections.
Peripheral arterial disease diagnosis and management US Medical PG Question 9: A 63-year-old man presents to the clinic complaining of burning bilateral leg pain which has been increasing gradually over the past several months. It worsens when he walks but improves with rest. His past medical and surgical history are significant for hypertension, hyperlipidemia, diabetes, and a 40-pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 167/108 mm Hg, pulse is 88/min, respirations are 13/min, and oxygen saturation is 95% on room air. Physical exam of the lower extremities reveals palpable but weak posterior tibial and dorsalis pedis pulses bilaterally. Which of the following is the best initial treatment for this patient's symptoms?
- A. Exercise and smoking cessation (Correct Answer)
- B. Lovenox and atorvastatin
- C. Lisinopril and atorvastatin
- D. Balloon angioplasty with stenting
- E. Femoral-popliteal bypass
Peripheral arterial disease diagnosis and management Explanation: ***Exercise and smoking cessation***
- This patient presents with symptoms highly suggestive of **peripheral artery disease (PAD)**, characterized by **intermittent claudication** (leg pain worsening with activity and improving with rest), and risk factors like diabetes, hypertension, hyperlipidemia, and smoking.
- **Smoking cessation** is the single most important modifiable risk factor, and a supervised **exercise program** (walking to the point of claudication) is the most effective initial treatment to improve walking distance and quality of life for PAD patients.
*Lovenox and atorvastatin*
- **Atorvastatin** is appropriate for dyslipidemia and cardiovascular risk reduction in PAD patients, but **Lovenox (low molecular weight heparin)** is an anticoagulant typically used for acute thrombotic events or VTE prophylaxis, not initial management of chronic stable claudication.
- While statins are important for secondary prevention, Lovenox does not directly address the primary management of claudication symptoms or underlying atherosclerotic progression in this stable setting.
*Lisinopril and atorvastatin*
- **Lisinopril** is an ACE inhibitor suitable for hypertension, which is important for overall cardiovascular health but not the primary initial treatment for claudication symptoms.
- While both medications address risk factors, they do not directly target the improvement of walking function and symptom relief as effectively as exercise and smoking cessation in the initial phase.
*Balloon angioplasty with stenting*
- Invasive revascularization procedures like **balloon angioplasty with stenting** are typically reserved for patients with more severe symptoms (e.g., rest pain, non-healing ulcers, critical limb ischemia) or those who have failed conservative management like exercise therapy.
- This is not the **best initial treatment** for a patient with stable claudication.
*Femoral-popliteal bypass*
- **Femoral-popliteal bypass** is a surgical revascularization procedure indicated for more severe PAD, particularly in cases of critical limb ischemia or long-segment occlusions that are not amenable to endovascular repair.
- Like angioplasty, it is a more aggressive intervention and not the **initial treatment of choice** for intermittent claudication.
Peripheral arterial disease diagnosis and management US Medical PG Question 10: A 54-year-old man comes to the physician because of a painful mass in his left thigh for 3 days. He underwent a left lower limb angiography for femoral artery stenosis and had a stent placed 2 weeks ago. He has peripheral artery disease, coronary artery disease, hypercholesterolemia and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 34 years. Current medications include enalapril, aspirin, simvastatin, metformin, and sitagliptin. His temperature is 36.7°C (98°F), pulse is 88/min, and blood pressure is 116/72 mm Hg. Examination shows a 3-cm (1.2-in) tender, pulsatile mass in the left groin. The skin over the area of the mass shows no erythema and is cool to the touch. A loud bruit is heard on auscultation over this area. The remainder of the examination shows no abnormalities. Results of a complete blood count and serum electrolyte concentrations show no abnormalities. Duplex ultrasonography shows an echolucent sac connected to the common femoral artery, with pulsatile and turbulent blood flow between the artery and the sac. Which of the following is the most appropriate next best step in management?
- A. Ultrasound-guided thrombin injection (Correct Answer)
- B. Covered stent implantation
- C. Ultrasound-guided compression
- D. Coil embolization
- E. Schedule surgical repair
Peripheral arterial disease diagnosis and management Explanation: ***Ultrasound-guided thrombin injection***
- The patient presents with a **post-catheterization pseudoaneurysm** as indicated by the pulsatile, tender mass with a bruit after recent femoral angiography, and confirmed by duplex ultrasonography showing an echolucent sac connected to the common femoral artery with pulsatile flow.
- **Ultrasound-guided thrombin injection** is the preferred treatment for pseudoaneurysms that are larger than 2-3 cm or have been present for more than 1 week, as it effectively closes the pseudoaneurysm sac with a high success rate and minimal invasiveness.
*Covered stent implantation*
- This is a treatment for arterial injury or aneurysm, but it is generally reserved for **larger or more complex pseudoaneurysms**, or those that have failed less invasive treatments, due to its greater invasiveness and potential complications.
- It involves placing a stent graft to exclude the pseudoaneurysm from the circulation.
*Ultrasound-guided compression*
- This technique involves applying sustained pressure to the pseudoaneurysm neck, which can lead to thrombosis. However, it has a **lower success rate** compared to thrombin injection, especially for larger pseudoaneurysms, and is often painful and time-consuming.
- It is often considered a first-line therapy for smaller pseudoaneurysms (<2-3 cm) before thrombin injection, but in this case, the pseudoaneurysm is 3 cm.
*Coil embolization*
- This procedure is typically used to treat **arteriovenous malformations** or high-flow bleeding rather than pseudoaneurysms.
- It involves placing coils into the vessel to induce thrombosis, but carries risks of distal embolization and might be overly aggressive for a femoral pseudoaneurysm.
*Schedule surgical repair*
- **Surgical repair** is indicated for pseudoaneurysms that are rapidly expanding, symptomatic with critical limb ischemia, infected, or those that have failed less invasive treatments.
- In this case, given the patient's stable condition and the availability of less invasive options, surgical repair is not the initial best step.
More Peripheral arterial disease diagnosis and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.