Endovascular procedures overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endovascular procedures overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endovascular procedures overview US Medical PG Question 1: A 72-year-old woman comes to the physician for follow-up care. One year ago, she was diagnosed with a 3.8-cm infrarenal aortic aneurysm found incidentally on abdominal ultrasound. She has no complaints. She has hypertension, type 2 diabetes mellitus, and COPD. Current medications include hydrochlorothiazide, lisinopril, glyburide, and an albuterol inhaler. She has smoked a pack of cigarettes daily for 45 years. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 12/min, and blood pressure is 145/85 mm Hg. Examination shows a faint abdominal bruit on auscultation. Ultrasonography of the abdomen shows a 4.9-cm saccular dilation of the infrarenal aorta. Which of the following is the most appropriate next step in management?
- A. Elective endovascular aneurysm repair (Correct Answer)
- B. Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months
- C. Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months
- D. Elective open aneurysm repair
- E. Adjustment of cardiovascular risk factors and follow-up CT in 6 months
Endovascular procedures overview Explanation: ***Elective endovascular aneurysm repair***
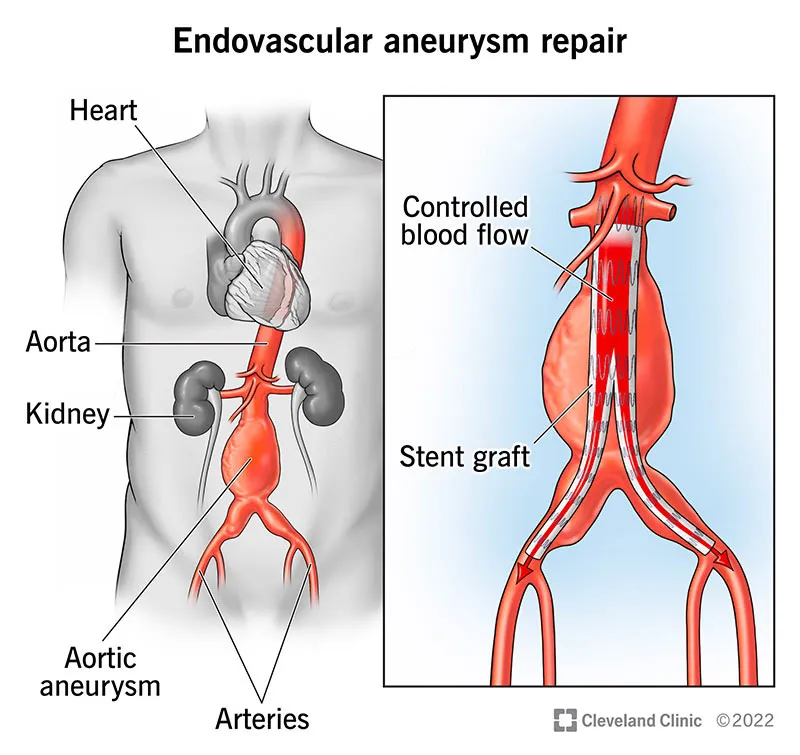
- The patient's **infrarenal aortic aneurysm** has grown from 3.8 cm to 4.9 cm in one year, approaching the **5.0 cm threshold for intervention in women** (compared to 5.5 cm for men). The **rapid growth rate of 1.1 cm/year** (normal is <0.5 cm/year) significantly increases rupture risk and is an indication for intervention even before reaching the absolute size threshold.
- Given her multiple comorbidities (hypertension, diabetes, COPD, 45 pack-year smoking history), **endovascular aneurysm repair (EVAR)** is preferred over open repair due to lower perioperative morbidity and mortality in high-risk surgical candidates.
- The combination of near-threshold size and rapid growth makes elective repair appropriate now rather than continued surveillance.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months*
- While **risk factor modification** (smoking cessation, blood pressure control) is essential, it is insufficient as the primary management given the aneurysm's significant growth and imminent rupture risk.
- A 12-month follow-up interval is too long for a rapidly growing aneurysm (grew 1.1 cm in the past year), as this increases the risk of rupture without intervention.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months*
- **Risk factor management** is important but does not address the immediate need for intervention due to the aneurysm's size approaching the threshold and concerning growth rate.
- While 6-month surveillance might be considered for smaller aneurysms with slower growth, this aneurysm's rapid expansion rate suggests it will exceed 5.0 cm well before the next surveillance interval, increasing rupture risk unnecessarily.
*Elective open aneurysm repair*
- **Open aneurysm repair** is an effective treatment but carries significantly higher perioperative risks (30-day mortality 3-5% vs 1-2% for EVAR) compared to endovascular repair, especially in patients with multiple comorbidities.
- Given this patient's COPD, smoking history, and cardiovascular risk factors, EVAR is the preferred approach to minimize surgical stress and improve perioperative outcomes.
*Adjustment of cardiovascular risk factors and follow-up CT in 6 months*
- **Risk factor modification** alone is insufficient given the aneurysm's proximity to intervention threshold and rapid growth rate.
- While CT provides more detailed anatomic imaging for surgical planning, continued surveillance is inappropriate when the patient already meets criteria for intervention. Additionally, CT involves radiation exposure and is typically reserved for pre-operative planning rather than routine surveillance.
Endovascular procedures overview US Medical PG Question 2: A 16-year-old boy comes to the physician for a routine health maintenance examination. He feels well. He has no history of serious illness. He is at the 60th percentile for height and weight. Vital signs are within normal limits. The lungs are clear to auscultation. A grade 3/6 ejection systolic murmur is heard along the lower left sternal border. The murmur decreases in intensity on rapid squatting and increases in intensity when he performs the Valsalva maneuver. This patient is at increased risk for which of the following complications?
- A. Sudden cardiac death (Correct Answer)
- B. Pulmonary apoplexy
- C. Infective endocarditis
- D. Cerebral aneurysm
- E. Angiodysplasia
Endovascular procedures overview Explanation: ***Sudden cardiac death***
- The murmur characteristics (decreases with squatting, increases with Valsalva) are classic for **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a leading cause of **sudden cardiac death** in young athletes.
- HOCM causes **left ventricular outflow tract obstruction** due to asymmetric septal hypertrophy and systolic anterior motion of the mitral valve, predisposing to fatal arrhythmias.
*Pulmonary apoplexy*
- This refers to severe **pulmonary hemorrhage**, which is not associated with the cardiac murmur described.
- It is typically seen in conditions like **Goodpasture's syndrome** or severe vasculitis.
*Infective endocarditis*
- While structural heart disease can increase the risk, the primary concern with HOCM is **sudden cardiac death** due to arrhythmia, not infective endocarditis, which generally requires specific predisposing factors like prosthetic valves or prolonged IV access.
- The murmur itself is due to obstruction, not typically indicative of an infection risk without other signs.
*Cerebral aneurysm*
- There is no direct association between the murmur characteristics described and an increased risk of **cerebral aneurysms**.
- Cerebral aneurysms are often linked to conditions like **polycystic kidney disease** or specific connective tissue disorders.
*Angiodysplasia*
- **Angiodysplasia** involves vascular malformations in the GI tract leading to bleeding, which is unrelated to the cardiovascular findings in this patient.
- It is often seen in older individuals or those with **aortic stenosis**, but not typically HOCM.
Endovascular procedures overview US Medical PG Question 3: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
Endovascular procedures overview Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Endovascular procedures overview US Medical PG Question 4: One and a half hours after undergoing an elective cardiac catheterization, a 53-year-old woman has right flank and back pain. She has hypertension, hypercholesterolemia, and type 2 diabetes mellitus. She had an 80% stenosis in the left anterior descending artery and 2 stents were placed. Intravenous unfractionated heparin was used prior to the procedure. Prior to admission, her medications were enalapril, simvastatin, and metformin. Her temperature is 37.3°C (99.1°F), pulse is 102/min, and blood pressure is 109/75 mm Hg. Examination shows a tender lower abdomen; there is no guarding or rigidity. There is right suprainguinal fullness and tenderness. There is no bleeding or discharge from the femoral access site. Cardiac examination shows no murmurs, rubs, or gallops. Femoral and pedal pulses are palpable bilaterally. 0.9% saline infusion is begun. A complete blood count shows a hematocrit of 36%, leukocyte count of 8,400/mm3, and a platelet count of 230,000/mm3. Which of the following is the most appropriate next step in management?
- A. X-ray of the abdomen
- B. Obtain an ECG
- C. CT scan of the abdomen and pelvis (Correct Answer)
- D. Administer protamine sulfate
- E. Administer intravenous atropine
Endovascular procedures overview Explanation: ***CT scan of the abdomen and pelvis***
- The patient's symptoms of **right flank and back pain**, along with **right suprainguinal fullness and tenderness** following cardiac catheterization with **anticoagulation**, are highly suggestive of a **retroperitoneal hemorrhage**.
- A **CT scan of the abdomen and pelvis** is the most appropriate diagnostic tool to confirm the presence, size, and location of the retroperitoneal bleed.
*X-ray of the abdomen*
- An **X-ray of the abdomen** is generally not useful for diagnosing soft tissue conditions like retroperitoneal hemorrhage.
- It would be primarily used for detecting **ureteral stones** or **bowel obstruction**, which are not the primary concerns with this presentation.
*Obtain an ECG*
- While an **ECG** is important in cardiac patients, the current symptoms of flank pain, back pain, and suprainguinal fullness are not typical signs of an acute cardiac event.
- The patient just underwent a successful cardiac catheterization and stent placement, making **ischemia** less likely to be the immediate cause of these specific symptoms.
*Administer protamine sulfate*
- **Protamine sulfate** is used to reverse the effects of **unfractionated heparin**, which was used prior to the procedure.
- While a retroperitoneal hemorrhage is suspected, reversal of heparin without definitive diagnosis and assessment of the bleeding severity could be premature and might increase the risk of **thrombosis** in a patient with recent stent placement.
*Administer intravenous atropine*
- **Intravenous atropine** is used to treat **bradycardia**.
- The patient's pulse is 102/min, indicating **tachycardia**, not bradycardia, making atropine an inappropriate treatment.
Endovascular procedures overview US Medical PG Question 5: A 17-year-old teenager is brought to the emergency department with severe bleeding from his right hand. He was involved in a gang fight about 30 minutes ago where he received a penetrating stab wound by a sharp knife in the region of the ‘anatomical snuffbox’. A vascular surgeon is called in for consultation. Damage to which artery is most likely responsible for his excessive bleeding?
- A. Ulnar artery
- B. Palmar carpal arch
- C. Radial artery (Correct Answer)
- D. Princeps pollicis artery
- E. Brachial artery
Endovascular procedures overview Explanation: ***Radial artery***
- The **anatomical snuffbox** is formed by the tendons of the **extensor pollicis longus**, **extensor pollicis brevis**, and **abductor pollicis longus**. The floor of this region is primarily formed by the **scaphoid** and **trapezial bones**.
- The **radial artery** passes directly through the anatomical snuffbox to contribute to the deep palmar arch. A penetrating injury in this area would most likely damage the radial artery, leading to significant bleeding.
*Ulnar artery*
- The **ulnar artery** runs along the medial side of the forearm and enters the hand superficial to the **flexor retinaculum**, lateral to the ulnar nerve.
- It does not pass through the **anatomical snuffbox**.
*Palmar carpal arch*
- The **palmar carpal arches** are anastomoses between the radial and ulnar arteries on the palmar aspect of the wrist.
- While they are in the vicinity, a direct stab in the **anatomical snuffbox** specifically targets the radial artery as it traverses this area.
*Princeps pollicis artery*
- The **princeps pollicis artery** is a branch of the **radial artery** that supplies the thumb.
- While it originates from the radial artery, the primary vessel at risk within the **anatomical snuffbox** itself, causing systemic excessive bleeding, is the main trunk of the radial artery before it gives off this specific branch.
*Brachial artery*
- The **brachial artery** is located in the arm and terminates in the cubital fossa, dividing into the radial and ulnar arteries.
- It is too proximal to be injured by a stab wound to the **anatomical snuffbox** in the hand.
Endovascular procedures overview US Medical PG Question 6: A 55-year-old man comes to the emergency department because of left-sided chest pain and difficulty breathing for the past 30 minutes. His pulse is 88/min. He is pale and anxious. Serum studies show increased cardiac enzymes. An ECG shows ST-elevations in leads I, aVL, and V5-V6. A percutaneous coronary intervention is performed. In order to localize the site of the lesion, the catheter must pass through which of the following structures?
- A. Left coronary artery → left circumflex artery (Correct Answer)
- B. Right coronary artery → posterior descending artery
- C. Left coronary artery → left anterior descending artery
- D. Right coronary artery → right marginal artery
- E. Left coronary artery → posterior descending artery
Endovascular procedures overview Explanation: ***Left coronary artery → left circumflex artery***
- **ST-elevations** in leads I, aVL, and V5-V6 are indicative of a **lateral myocardial infarction**.
- The **left circumflex artery** primarily supplies the lateral wall of the left ventricle.
*Right coronary artery → posterior descending artery*
- The **posterior descending artery** (PDA) typically supplies the inferior wall and posterior interventricular septum.
- An occlusion here would cause **ST-elevations** in leads II, III, and aVF, which is not seen in this case.
*Left coronary artery → left anterior descending artery*
- The **left anterior descending** (LAD) artery supplies the anterior wall and apex of the left ventricle.
- Occlusion of the LAD would typically cause **ST-elevations** in leads V1-V4, indicating an anterior MI.
*Right coronary artery → right marginal artery*
- The **right marginal artery** is a branch of the right coronary artery and supplies part of the right ventricle.
- Occlusion here would primarily affect the **right ventricle**, and is not typically associated with the given ECG changes.
*Left coronary artery → posterior descending artery*
- While the **posterior descending artery** can sometimes originate from the left circumflex artery (**left dominant circulation**), it primarily supplies the inferior wall.
- The observed ECG changes in leads I, aVL, and V5-V6 are characteristic of a **lateral wall infarct**, which is supplied by the left circumflex artery.
Endovascular procedures overview US Medical PG Question 7: A 33-year-old woman comes to the emergency department because of severe right flank pain for 2 hours. The pain is colicky in nature and she describes it as 9 out of 10 in intensity. She has had 2 episodes of vomiting. She has no history of similar episodes in the past. She is 160 cm (5 ft 3 in) tall and weighs 104 kg (229 lb); BMI is 41 kg/m2. Her temperature is 37.3°C (99.1°F), pulse is 96/min, respirations are 16/min and blood pressure is 116/76 mm Hg. The abdomen is soft and there is mild tenderness to palpation in the right lower quadrant. Bowel sounds are reduced. The remainder of the examination shows no abnormalities. Her leukocyte count is 7,400/mm3. A low-dose CT scan of the abdomen and pelvis shows a round 12-mm stone in the distal right ureter. Urine dipstick is mildly positive for blood. Microscopic examination of the urine shows RBCs and no WBCs. 0.9% saline infusion is begun and intravenous ketorolac is administered. Which of the following is the most appropriate next step in management?
- A. Ureteral stenting
- B. Ureteroscopy (Correct Answer)
- C. Observation
- D. Extracorporeal shock wave lithotripsy
- E. Thiazide diuretic therapy
Endovascular procedures overview Explanation: ***Ureteroscopy***
- **Ureteroscopy** is the most appropriate next step for a 12-mm symptomatic distal ureteral stone, especially given its size.
- It allows for direct visualization of the stone and immediate fragmentation or extraction, providing rapid relief of symptoms and addressing the obstruction.
*Ureteral stenting*
- **Ureteral stenting** is primarily used to relieve obstruction and pain, or to bypass the stone, but it does not remove the stone.
- It is often considered a temporary measure to decompress the kidney, particularly in cases of infection or severe obstruction, but definitive treatment for the stone would still be needed.
*Observation*
- **Observation** is generally reserved for smaller ureteral stones (typically <5 mm) that are likely to pass spontaneously.
- A 12-mm stone has a very low chance of spontaneous passage and would likely lead to prolonged pain, obstruction, and potential complications.
*Extracorporeal shock wave lithotripsy*
- **Extracorporeal shock wave lithotripsy (ESWL)** is less effective for larger stones (>10 mm) and stones located in the distal ureter, as successful fragmentation and passage are reduced.
- It is generally more effective for smaller, proximal ureteral or renal stones.
*Thiazide diuretic therapy*
- **Thiazide diuretics** are used as a preventative measure to reduce calcium excretion and thus decrease the risk of new calcium stone formation, but they are not a treatment for an acutely obstructing stone.
- This therapy would not alleviate the current acute pain or obstruction caused by the 12-mm stone.
Endovascular procedures overview US Medical PG Question 8: A 36-year-old man comes to the emergency department 4 hours after a bike accident for severe pain and swelling in his right leg. He has not had a headache, nausea, vomiting, abdominal pain, or blood in his urine. He has a history of gastroesophageal reflux disease and allergic rhinitis. He has smoked one pack of cigarettes daily for 17 years and drinks an average of one alcoholic beverage daily. His medications include levocetirizine and pantoprazole. He is in moderate distress. His temperature is 37°C (98.6°F), pulse is 112/min, and blood pressure is 140/80 mm Hg. Examination shows multiple bruises over both lower extremities and the face. There is swelling surrounding a 2 cm laceration 13 cm below the right knee. The lower two-thirds of the tibia is tender to palpation and the skin is pale and cool to the touch. The anterior tibial, posterior tibial, and dorsalis pedis pulses are weak. Capillary refill time of the right big toe is 4 seconds. Dorsiflexion of his right foot causes severe pain in his calf. Cardiopulmonary examination is normal. An x-ray is ordered, which is shown below. Which of the following is the most appropriate next step in management?
- A. Above knee cast
- B. IVC filter placement
- C. Fasciotomy (Correct Answer)
- D. Low molecular weight heparin
- E. Open reduction and internal fixation
Endovascular procedures overview Explanation: ***Fasciotomy***
- The patient's symptoms (severe pain, swelling, pain with passive dorsiflexion, weak pulses, pale/cool skin, and prolonged capillary refill) after a traumatic injury are highly suggestive of **acute compartment syndrome**.
- **Fasciotomy** is the definitive treatment for acute compartment syndrome to relieve pressure and prevent irreversible tissue damage.
*Above knee cast*
- While a cast is used for immobilization of fractures, it would worsen **compartment syndrome** by externally compressing an already swollen limb.
- This patient has signs of compartment syndrome which requires urgent surgical decompression, not just immobilization.
*IVC filter placement*
- **IVC filter placement** is indicated for preventing pulmonary embolism in patients with deep vein thrombosis (DVT) who have contraindications to anticoagulation.
- There is no clinical evidence to suggest DVT in this patient, and the primary concern is acute compartment syndrome.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is an anticoagulant used for DVT prophylaxis or treatment.
- It is not indicated for the immediate management of acute compartment syndrome and could increase the risk of bleeding in a patient who likely needs urgent surgery.
*Open reduction and internal fixation*
- **Open reduction and internal fixation (ORIF)** is a surgical procedure to stabilize complex fractures, which may be needed later for a tibial fracture if present.
- However, the immediate priority is to address the limb-threatening acute compartment syndrome before performing definitive fracture repair.
Endovascular procedures overview US Medical PG Question 9: A 59-year-old patient comes to the emergency department accompanied by his wife because of severe right leg pain and numbness. His condition suddenly started an hour ago. His wife says that he has a heart rhythm problem for which he takes a blood thinner, but he is not compliant with his medications. He has smoked 10–15 cigarettes daily for the past 15 years. His temperature is 36.9°C (98.42°F), blood pressure is 140/90 mm Hg, and pulse is 85/min and irregular. On physical examination, the patient is anxious and his right leg is cool and pale. Palpation of the popliteal fossa shows a weaker popliteal pulse on the right side compared to the left side. Which of the following is the best initial step in the management of this patient's condition?
- A. Urgent assessment for amputation or revascularization (Correct Answer)
- B. Decompressive laminectomy
- C. Oral acetaminophen and topical capsaicin
- D. Arthroscopic synovectomy
- E. Cilostazol
Endovascular procedures overview Explanation: ***Urgent assessment for amputation or revascularization***
- The patient presents with classic signs of **acute limb ischemia** (severe pain, numbness, coolness, pallor, and diminished pulse) in the setting of chronic atrial fibrillation and medication non-compliance, indicating an **embolic event**.
- **Immediate surgical consultation** for revascularization and limb salvage is critical to prevent irreversible tissue damage and potential amputation.
*Decompressive laminectomy*
- This procedure is indicated for conditions like **spinal stenosis** or **herniated disc** causing nerve root compression, typically presenting with radicular pain, weakness, or sensory deficits.
- The patient's acute onset of symptoms, limb ischemia signs, and irregular pulse are not consistent with a spinal compressive neuropathy.
*Oral acetaminophen and topical capsaicin*
- These are **palliative treatments** for pain that is typically chronic and less severe, such as osteoarthritis or neuropathic pain.
- They are entirely inadequate for the management of **acute limb ischemia**, which requires urgent intervention to restore blood flow.
*Arthroscopic synovectomy*
- This is a surgical procedure to remove inflamed synovial tissue from a joint, typically performed for conditions like **rheumatoid arthritis** or other inflammatory arthropathies that have not responded to medical management.
- It is irrelevant to the management of acute vascular compromise of a limb.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used in the long-term management of **intermittent claudication** due to peripheral artery disease to improve walking distance and reduce symptoms.
- It has no role in the acute treatment of **severe limb ischemia**, which is an emergency requiring immediate revascularization, not a medication for chronic symptoms.
Endovascular procedures overview US Medical PG Question 10: A 62-year-old man presents to the emergency department with sudden onset of severe left leg pain accompanied by numbness and weakness. His medical history is remarkable for hypertension and hyperlipidemia. His vital signs include a blood pressure of 155/92 mm Hg, a temperature of 37.1°C (98.7°F), and an irregular pulse of 92/min. Physical examination reveals absent left popliteal and posterior tibial pulses. His left leg is noticeably cold and pale. There is no significant tissue compromise, nerve damage, or sensory loss. Which of the following will most likely be required for this patient's condition?
- A. Antibiotics
- B. Warfarin
- C. Fasciotomy
- D. Amputation
- E. Thromboembolectomy (Correct Answer)
Endovascular procedures overview Explanation: ***Thromboembolectomy***
- The sudden onset of severe leg pain, numbness, and weakness with absent pulses, a cold, pale limb, and an irregular pulse suggests **acute limb ischemia** likely due to an **arterial embolus**, which requires emergent surgical removal.
- Given the symptoms and history of an irregular pulse (suggesting possible atrial fibrillation), a thromboembolectomy is the most appropriate first-line treatment to restore blood flow and prevent permanent damage.
*Antibiotics*
- Antibiotics are used to treat **bacterial infections** and are not indicated for acute limb ischemia caused by a vascular occlusion.
- There are no signs of infection present, such as fever, redness, or purulent discharge, that would warrant antibiotic therapy.
*Warfarin*
- Warfarin is an **anticoagulant** used for long-term prevention of clot formation, particularly in conditions like atrial fibrillation or deep vein thrombosis.
- While anticoagulation may eventually be part of management to prevent future events, it is insufficient as immediate therapy for an acute, established arterial embolus causing critical limb ischemia.
*Fasciotomy*
- Fasciotomy is performed to relieve **compartment syndrome**, which occurs when increased pressure within a muscle compartment compromises circulation and nerve function.
- While compartment syndrome can be a complication of reperfusion after prolonged ischemia, it is not the primary treatment for the initial arterial occlusion; the first step is to restore blood flow to prevent the need for it.
*Amputation*
- Amputation is a last resort considered when the limb is **irreversibly ischemic** and non-viable, or when revascularization attempts have failed and there is extensive tissue necrosis or infection.
- In this case, there is no significant tissue compromise or nerve damage mentioned, indicating that the limb is still salvageable with timely intervention.
More Endovascular procedures overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.