Carotid endarterectomy indications and technique US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Carotid endarterectomy indications and technique. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
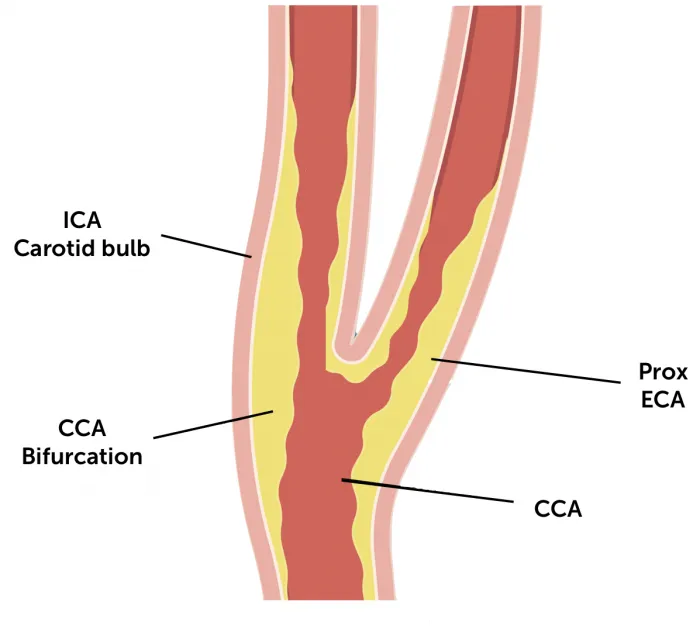
Carotid endarterectomy indications and technique US Medical PG Question 1: A 71-year-old woman presents with a transient episode of right arm and hand weakness that resolved in approximately one hour. Her symptoms started while she was gardening. Her past medical history is notable for hypertension, diabetes, anxiety, and dyslipidemia. Her current medications include insulin, metformin, and fluoxetine. Examination reveals a left carotid bruit. Ultrasound duplex of her carotid arteries demonstrates right and left carotid stenosis of 35% and 50%, respectively. Which of the following is the best next step in management?
- A. Bilateral carotid endarterectomy
- B. Left carotid endarterectomy only
- C. Aspirin (Correct Answer)
- D. Observation
- E. Warfarin
Carotid endarterectomy indications and technique Explanation: ***Aspirin***
- This patient suffered a **transient ischemic attack (TIA)** given her transient focal neurological deficit. Given that her carotid stenosis is **moderate (35% and 50%)**, **antiplatelet therapy** with aspirin is the initial and best next step to prevent future strokes.
- Aspirin helps prevent platelet aggregation, reducing the risk of **thrombus formation** in already stenotic vessels.
*Bilateral carotid endarterectomy*
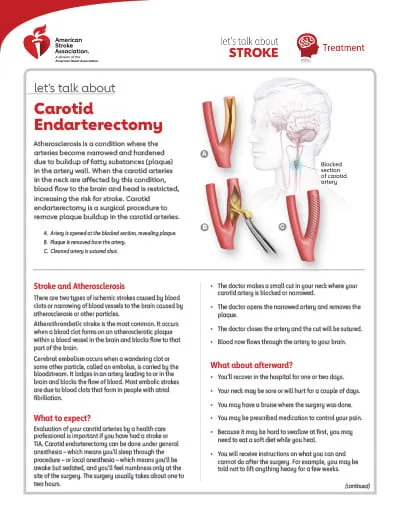
- This is not the best next step, as **carotid endarterectomy** is generally reserved for symptomatic patients with **high-grade stenosis** (e.g., typically >70%).
- Performing bilateral procedures at once carries higher risks than staged procedures or medical management for moderate stenosis.
*Left carotid endarterectomy only*
- This is not indicated. While symptoms occurred on the right side (implying a left-sided lesion), a **left carotid endarterectomy** is primarily considered for **high-grade stenosis** in symptomatic patients.
- Her left carotid stenosis is 50%, which is considered moderate and not an immediate indication for surgery.
*Observation*
- This is inappropriate as the patient has experienced a **TIA**, indicating a high risk of future stroke.
- Without intervention, including antiplatelet therapy, the risk of a debilitating stroke is significantly increased.
*Warfarin*
- **Warfarin** is an anticoagulant used for conditions like atrial fibrillation or deep vein thrombosis but is **not the primary treatment for TIA due to carotid stenosis**.
- Its use in this context may increase the risk of bleeding without providing superior benefit to aspirin in preventing arterial clots from carotid plaques.
Carotid endarterectomy indications and technique US Medical PG Question 2: A 68-year-old man is brought to the emergency department because of right-sided weakness for 2 hours. He has hypertension, dyslipidemia, and type 2 diabetes. Current medications include hydrochlorothiazide, metoprolol, amlodipine, pravastatin, and metformin. His pulse is 87/min and blood pressure is 164/98 mm Hg. Neurological examination shows right-sided weakness, facial droop, and hyperreflexia. Sensation is intact. Which of the following is the most likely cause of these findings?
- A. Lipohyalinosis of penetrating vessels (Correct Answer)
- B. Dissection of the vertebral artery
- C. Stenosis of the internal carotid artery
- D. Rupture of an intracranial aneurysm
- E. Embolism from the left atrium
Carotid endarterectomy indications and technique Explanation: ***Lipohyalinosis of penetrating vessels***
- This patient presents with an acute onset of **hemiparesis**, **facial droop**, and hyperreflexia, without cortical signs like cortical sensory loss or aphasia, which is characteristic of a **lacunar stroke**.
- **Lipohyalinosis** is the most common cause of lacunar infarcts, resulting from chronic hypertension and diabetes affecting small penetrating arteries in the brain.
*Dissection of the vertebral artery*
- Vertebral artery dissection typically presents with **posterior circulation symptoms** such as vertigo, ataxia, brainstem dysfunction, and often includes severe headache or neck pain.
- The presented symptoms of pure motor hemiparesis are more indicative of an anterior circulation event involving deeper structures.
*Stenosis of the internal carotid artery*
- Significant **internal carotid artery stenosis** typically causes larger territorial infarcts by reducing blood flow or via artery-to-artery embolism to the middle cerebral artery territory.
- This would result in symptoms like **aphasia**, **cortical sensory deficits**, or **homonymous hemianopia**, which are not present here.
*Rupture of an intracranial aneurysm*
- A ruptured intracranial aneurysm usually causes a **subarachnoid hemorrhage**, leading to a sudden, severe headache ("thunderclap headache"), meningismus, and altered consciousness.
- While focal neurological deficits can occur, the primary presentation is distinct from the patient's symptoms of a gradual onset of pure motor deficit.
*Embolism from the left atrium*
- An embolism from the left atrium (e.g., due to atrial fibrillation) typically causes a **cortical infarct** involving a larger vascular territory, such as the middle cerebral artery.
- This would result in symptoms like **aphasia**, **neglect**, or **cortical sensory deficits**, which are absent in this presentation of pure motor hemiparesis.
Carotid endarterectomy indications and technique US Medical PG Question 3: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Carotid endarterectomy indications and technique Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Carotid endarterectomy indications and technique US Medical PG Question 4: An 85-year-old woman otherwise healthy presents with left-sided weakness. Her symptoms started 4 hours ago while she was on the phone with her niece. The patient recalls dropping the phone and not being able to pick it up with her left hand. No significant past medical history. No current medications. Physical examination reveals decreased sensation on the left side, worse in the left face and left upper extremity. There is significant weakness of the left upper extremity and weakness and drooping of the lower half of the left face. Ophthalmic examination reveals conjugate eye deviation to the right. A noncontrast CT of the head is unremarkable. The patient is started on aspirin. A repeat contrast CT of the head a few days later reveals an ischemic stroke involving the lateral convexity of right cerebral hemisphere. Which of the following additional findings would most likely be seen in this patient?
- A. Homonymous hemianopsia (Correct Answer)
- B. Horner's syndrome
- C. Amaurosis fugax
- D. Profound lower limb weakness
- E. Prosopagnosia
Carotid endarterectomy indications and technique Explanation: ***Homonymous hemianopsia***
- The patient has an ischemic stroke affecting the **right cerebral hemisphere**, specifically the **lateral convexity**. This suggests involvement of the **middle cerebral artery (MCA)** territory.
- The **optic radiations** carrying visual information from the contralateral visual field pass through the parietal and temporal lobes to the occipital cortex. Damage to these radiations in the right hemisphere would result in a **left homonymous hemianopsia**.
*Horner's syndrome*
- Characterized by **ptosis**, **miosis**, and **anhidrosis** on one side of the face.
- It results from damage to the **sympathetic pathway**, typically in the brainstem, spinal cord above T1, or sympathetic chain, which is not the primary location of this stroke.
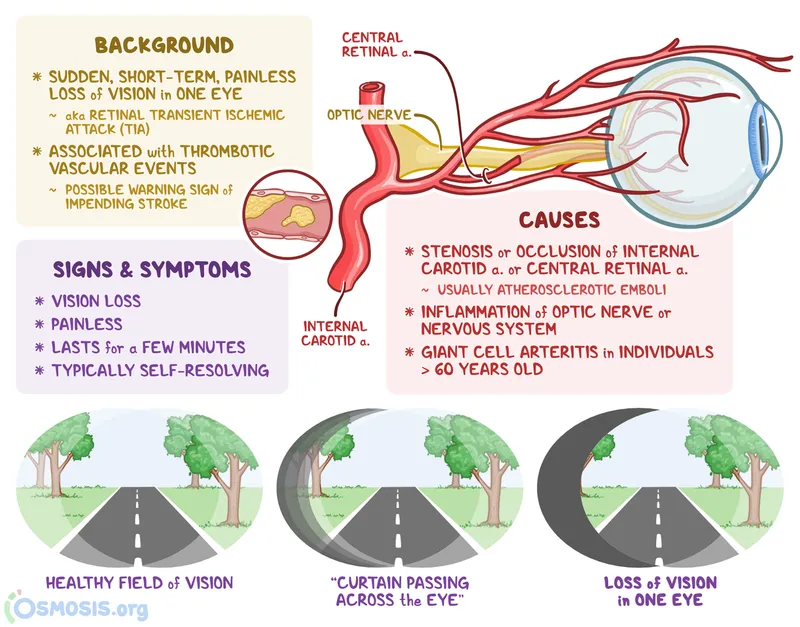
*Amaurosis fugax*
- This is a **transient monocular vision loss** ("curtain coming down") due to temporary interruption of blood flow to the retina, usually from an **ipsilateral carotid artery embolus**.
- It is typically a symptom of impending stroke or TIA, not a direct neurological deficit resulting from a cerebral hemisphere stroke.
*Profound lower limb weakness*
- The described stroke involves the **lateral convexity of the right cerebral hemisphere**, fed by the **middle cerebral artery (MCA)**.
- The MCA primarily supplies the upper limb and facial motor/sensory cortices, leading to more pronounced **upper limb and facial weakness** rather than profound lower limb weakness, which is more characteristic of an **anterior cerebral artery (ACA)** stroke.
*Prosopagnosia*
- This is the inability to recognize familiar faces, often due to damage to the **fusiform gyrus** in the temporal and occipital lobes, usually on the **right side**.
- While it can occur with right hemisphere strokes, it is a specific higher-order cognitive deficit and not the *most likely* additional finding in this presentation focused on motor and sensory deficits and conjugate eye deviation.
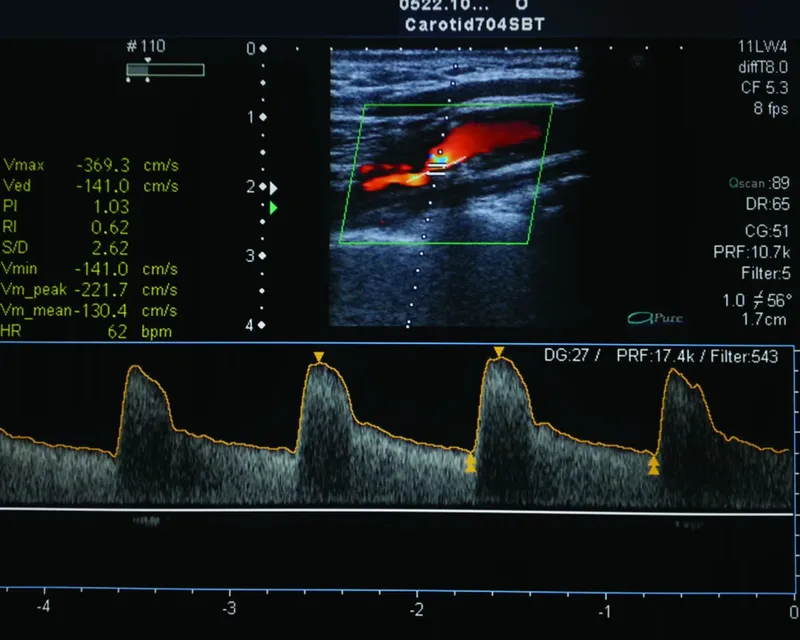
Carotid endarterectomy indications and technique US Medical PG Question 5: A 76-year-old man comes to the emergency department because of an episode of seeing jagged edges followed by loss of central vision in his right eye. The episode occurred 6 hours ago and lasted approximately 5 minutes. The patient has no pain. He has a 3-month history of intermittent blurriness out of his right eye and reports a 10-minute episode of slurred speech and left-sided facial droop that occurred 2 months ago. He has hypercholesterolemia, stable angina pectoris, hypertension, and a 5-year history of type 2 diabetes mellitus. Medications include glyburide, atorvastatin, labetalol, isosorbide, lisinopril, and aspirin. He feels well. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 76/min, respirations are 12/min, and blood pressure is 154/78 mm Hg. The extremities are well perfused with strong peripheral pulses. Ophthalmologic examination shows visual acuity of 20/30 in the left eye and 20/40 in the right eye. Visual fields are normal. Fundoscopic examination shows two pale spots along the supratemporal and inferotemporal arcade. Neurologic examination shows no focal findings. Cardiopulmonary examination shows systolic rumbling at the right carotid artery. The remainder of the examination shows no abnormalities. An ECG shows normal sinus rhythm with no evidence of ischemia. Which of the following is the most appropriate next step in management?
- A. Echocardiography
- B. Fluorescein angiography
- C. Temporal artery biopsy
- D. Reassurance and follow-up
- E. Carotid duplex ultrasonography (Correct Answer)
Carotid endarterectomy indications and technique Explanation: ***Carotid duplex ultrasonography***
- The patient's presentation with **transient monocular vision loss** (**amaurosis fugax**), transient ischemic attack (TIA) symptoms (**slurred speech, facial droop**), and a **carotid bruit** strongly suggests carotid artery stenosis as the source of emboli.
- **Carotid duplex ultrasonography** is the gold standard initial non-invasive imaging test to assess for **carotid artery stenosis** in symptomatic patients.
*Echocardiography*
- While echocardiography can identify cardiac sources of emboli (e.g., atrial fibrillation, valvular vegetations, PFO), the presence of a **carotid bruit** and prior TIA symptoms points more directly to carotid disease as the cause of transient visual and neurological deficits.
- This would be a reasonable next step if carotid studies were negative or if there were strong cardiac risk factors without carotid ones.
*Fluorescein angiography*
- **Fluorescein angiography** is used to evaluate the retinal circulation and can identify areas of ischemia or neovascularization, but it is not the primary diagnostic tool for determining the **etiology of amaurosis fugax** in a patient with a carotid bruit.
- It would be considered if a primary retinal vascular disease, rather than embolic phenomenon, were suspected.
*Temporal artery biopsy*
- **Temporal artery biopsy** is used to diagnose **giant cell arteritis (temporal arteritis)**, which can cause amaurosis fugax.
- However, this patient lacks typical symptoms of giant cell arteritis such as headache, jaw claudication, scalp tenderness, or an elevated ESR/CRP, making it less likely given the prominent carotid bruit and other embolic symptoms.
*Reassurance and follow-up*
- Given the patient's history of multiple transient ischemic events (amaurosis fugax, TIA) and clear signs of potential atherosclerotic disease (**carotid bruit**, multiple cardiovascular risk factors), **reassurance alone is inappropriate**.
- These are warning signs of impending stroke, and prompt investigation and management are crucial to prevent further, potentially permanent, neurological damage.
Carotid endarterectomy indications and technique US Medical PG Question 6: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
Carotid endarterectomy indications and technique Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
Carotid endarterectomy indications and technique US Medical PG Question 7: An 81-year-old woman presents to her physician complaining of occasional right-sided weakness in her arm and leg. She reports 3 such episodes over the last 6 months, each lasting only 1 hour and not significantly affecting her daily functioning. The patient denies numbness and tingling, pain, weakness in her left side, and changes in her speech. She has a past medical history of hypertension and coronary artery disease with stable angina, and her medications include 81 mg aspirin, 20 mg lisinopril, 5 mg amlodipine, and 20 mg atorvastatin daily. The patient reports a 40-pack-year smoking history and occasional alcohol intake. At this visit, her temperature is 98.5°F (36.9°C), blood pressure is 142/87 mmHg, pulse is 70/min, and respirations are 14/min. She has a grade II systolic ejection murmur best heard at the right upper sternal border, and there is a carotid bruit on the left side. Her lungs are clear. Neurologic exam reveals intact cranial nerve function, 1+ deep tendon reflexes in bilateral patellae and biceps, as well as 5/5 strength and intact pinprick sensation in all extremities. Carotid ultrasound is performed and identifies 52% stenosis on the right side and 88% on the left. Which of the following is the best next step in management?
- A. Perform carotid endarterectomy on left side only (Correct Answer)
- B. Repeat carotid ultrasound in 6 months
- C. Perform carotid endarterectomy on both sides
- D. Increase atorvastatin to 80 mg daily
- E. Perform carotid artery angioplasty with stenting (CAS)
Carotid endarterectomy indications and technique Explanation: ***Perform carotid endarterectomy on left side only***
- The patient's symptoms (right-sided weakness) are consistent with **transient ischemic attacks (TIAs)** affecting the left cerebral hemisphere, fed by the **left carotid artery**.
- Her left carotid artery shows **88% stenosis**, which is a high-grade stenosis in a symptomatic patient, warranting intervention like **carotid endarterectomy (CEA)** to prevent stroke.
*Repeat carotid ultrasound in 6 months*
- This approach is appropriate for **asymptomatic patients** with moderate stenosis (e.g., 50-79%) or for those with low-grade stenosis.
- Given the patient's **symptomatic TIAs** and **high-grade stenosis (88%)** on the left, waiting 6 months would significantly increase her risk of stroke.
*Perform carotid endarterectomy on both sides*
- The patient's symptoms are localized to the right side, implicating the **left carotid artery**.
- While the right carotid artery has 52% stenosis, it is currently **asymptomatic** and does not meet current guidelines for immediate surgical intervention.
*Increase atorvastatin to 80 mg daily*
- While **high-intensity statin therapy (atorvastatin 80 mg)** is crucial for **atherosclerosis management** and stroke prevention, it is not the primary next step for a symptomatic patient with high-grade carotid stenosis.
- Medical therapy alone is insufficient to address the immediate stroke risk posed by the **88% left carotid stenosis**.
*Perform carotid artery angioplasty with stenting (CAS)*
- **Carotid artery stenting (CAS)** is an alternative to CEA, but it generally carries a **higher stroke risk** in older patients (over 70-75 years) and those without specific indications (e.g., high surgical risk for CEA, previous neck radiation, recurrent stenosis after CEA).
- For an 81-year-old, **CEA is generally preferred over CAS** for symptomatic high-grade stenosis due to a lower risk of periprocedural stroke.
Carotid endarterectomy indications and technique US Medical PG Question 8: A 63-year-old female with known breast cancer presents with progressive motor weakness in bilateral lower extremities and difficulty ambulating. Physical exam shows 4 of 5 motor strength in her legs and hyper-reflexia in her patellar tendons. Neurologic examination 2 weeks prior was normal. Imaging studies, including an MRI, show significant spinal cord compression by the metastatic lesion and complete erosion of the T12 vertebrae. She has no metastatic disease to the visceral organs and her oncologist reports her life expectancy to be greater than one year. What is the most appropriate treatment?
- A. Palliative pain management consultation
- B. Surgical decompression and postoperative radiotherapy (Correct Answer)
- C. High-dose corticosteroids and clinical observation
- D. Radiation therapy alone
- E. Chemotherapy alone
Carotid endarterectomy indications and technique Explanation: ***Surgical decompression and postoperative radiotherapy***
- There is **spinal cord compression** by a metastatic lesion in a patient with a good prognosis (>1 year life expectancy) and rapidly progressive neurological deficits. **Surgical decompression** offers immediate relief of compression, while **postoperative radiotherapy** helps local tumor control.
- This combined approach is superior in preserving neurological function and improving quality of life for patients with **epidural spinal cord compression (ESCC)** in this clinical context.
*Palliative pain management consultation*
- While pain management is important in cancer care, this option alone does not address the **progressive neurological deficits** due to spinal cord compression.
- This patient's condition requires active treatment to prevent further neurological compromise and is not solely focused on comfort measures at this stage given her prognosis.
*Spinal dose corticosteroids and clinical observation*
- **Corticosteroids** can temporarily reduce edema around the spinal cord, but they do not resolve the mechanical compression caused by the eroded T12 vertebrae.
- **Clinical observation** without definitive intervention risks irreversible neurological damage given the rapid progression of symptoms.
*Radiation therapy alone*
- While radiation therapy is effective for local tumor control, it may not provide **rapid enough decompression** for acute or rapidly progressing neurological deficits due to significant mechanical compression.
- In cases of severe compression, such as bone erosion and cord involvement, surgery is usually needed prior to or in combination with radiation.
*Chemotherapy alone*
- **Chemotherapy** for breast cancer is a systemic treatment and may take time to reduce tumor burden, which is not suitable for urgent relief of **spinal cord compression**.
- It does not provide immediate mechanical decompression and is generally not the primary treatment for acute ESCC, especially with bone involvement.
Carotid endarterectomy indications and technique US Medical PG Question 9: A 65-year-old man comes to the emergency department because of sudden, worsening pain in his right calf and foot that started 30 minutes ago. He also has a tingling sensation and weakness in his right leg. He has had no similar episodes, recent trauma, or claudication. He has type 2 diabetes mellitus and was diagnosed with hypertension 20 years ago. His sister has systemic sclerosis. He works as an office administrator and sits at his desk most of the day. He has smoked one and a half packs of cigarettes daily for 30 years. Current medications include metformin and lisinopril. His pulse is 110/min, respirations are 16/min, and blood pressure is 140/90 mm Hg. His right leg is pale and cool to touch. Muscle strength in his right leg is mildly reduced. Pedal pulses are absent on the right. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Popliteal artery aneurysm
- B. Atherosclerotic narrowing of the artery
- C. Arterial vasospasm
- D. Atheroembolism
- E. Arterial embolism (Correct Answer)
Carotid endarterectomy indications and technique Explanation: ***Arterial embolism***
- The sudden onset of severe unilateral limb pain, pallor, coolness, and absent pulses in a patient with risk factors for **atherosclerosis** and possible **arrhythmias** (given the history of hypertension and diabetes) strongly suggests acute limb ischemia due to an arterial embolism.
- The patient's presentation aligns with the "6 P's" of acute limb ischemia: **pain, pallor, pulselessness, paresthesias, poikilothermia (coolness), and paralysis** (weakness).
*Popliteal artery aneurysm*
- While a popliteal artery aneurysm can cause acute limb ischemia due to thrombosis or embolism within the aneurysm, it is more commonly associated with chronic limb ischemia or rupture, and a **palpable pulsatile mass** is typically present, which is not mentioned.
- The suddenness and severity of symptoms are more indicative of an embolic event rather than a thrombotic event within an aneurysm, which often presents less acutely.
*Atherosclerotic narrowing of the artery*
- **Atherosclerotic narrowing** typically causes chronic limb ischemia with symptoms like **claudication**, which is pain that worsens with exercise and improves with rest. The patient explicitly denies claudication.
- Acute worsening of atherosclerotic narrowing, often due to **plaque rupture and thrombosis**, would usually affect a limb with pre-existing claudication, and the onset might be less abrupt than described.
*Arterial vasospasm*
- **Arterial vasospasm** (e.g., Raynaud's phenomenon) primarily affects the small arteries and arterioles, typically in the digits, and is often triggered by cold or stress.
- It would not typically cause acute, severe, and widespread limb ischemia with absent pedal pulses in a large artery, and the patient's symptoms are not consistent with known vasospastic disorders affecting large vessels.
*Atheroembolism*
- **Atheroembolism** (e.g., "blue toe syndrome") typically involves multiple, small cholesterol emboli showering downstream, causing patchy ischemia, livedo reticularis, and renal or gastrointestinal involvement.
- While the patient has significant atherosclerotic risk factors, the sudden, complete obliteration of flow to the entire right leg, indicated by absent pedal pulses and diffuse symptoms, points more towards a **single, larger embolic occlusion** rather than diffuse microemboli.
Carotid endarterectomy indications and technique US Medical PG Question 10: A 79-year-old man is brought to the emergency department after he noted the abrupt onset of weakness accompanied by decreased sensation on his left side. His symptoms developed rapidly, peaked within 1 minute, and began to spontaneously resolve 10 minutes later. Upon arrival in the emergency room 40 minutes after the initial onset of symptoms, they had largely resolved. The patient has essential hypertension, type 2 diabetes mellitus, chronic obstructive pulmonary disease, and a 50 pack-year smoking history. He also had an ST-elevation myocardial infarction 3 years ago. His brain CT scan without contrast is reported as normal. Carotid duplex ultrasonography reveals 90% stenosis of the right internal carotid. His transthoracic echocardiogram does not reveal any intracardiac abnormalities. Which of the following interventions is most appropriate for this patient's condition?
- A. Carotid stenting (Correct Answer)
- B. Warfarin
- C. Low molecular weight heparin
- D. Hypercoagulability studies
- E. Aspirin and clopidogrel
Carotid endarterectomy indications and technique Explanation: ***Carotid stenting***
- The patient experienced a **transient ischemic attack (TIA)** with **90% stenosis of the right internal carotid artery**, which is a high-grade stenosis.
- **Carotid revascularization** is highly recommended for symptomatic patients with **high-grade carotid stenosis** (70–99%) to prevent future strokes.
- Both **carotid endarterectomy (CEA)** and **carotid stenting** are acceptable options. In this elderly patient (79 years) with significant comorbidities (COPD, prior MI, 50 pack-year smoking history), **carotid stenting** may be preferred as it avoids the surgical risks of general anesthesia and neck dissection.
*Warfarin*
- **Warfarin** is primarily used for preventing strokes in patients with **atrial fibrillation** or mechanical heart valves.
- It is **not the first-line treatment** for stroke prevention directly caused by symptomatic carotid artery stenosis.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is typically used for acute treatment of **deep vein thrombosis** and **pulmonary embolism**, or in certain acute coronary syndromes.
- It does not address the underlying **structural issue of severe carotid stenosis** for long-term stroke prevention.
*Hypercoagulability studies*
- While hypercoagulability can cause strokes, the patient's symptoms are clearly attributed to **severe carotid stenosis**.
- These studies are usually reserved for patients with strokes of **unexplained etiology**, especially younger patients, or those with unusual clot locations.
*Aspirin and clopidogrel*
- **Dual antiplatelet therapy (aspirin and clopidogrel)** is often used after a TIA or minor stroke, but typically for a limited duration (e.g., 21-90 days), and it is an adjunct to revascularization in severe carotid stenosis.
- Although important for **secondary stroke prevention**, it does not address the critical **90% carotid stenosis** that warrants revascularization.
More Carotid endarterectomy indications and technique US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.