Bypass grafting techniques and materials US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bypass grafting techniques and materials. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bypass grafting techniques and materials US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Bypass grafting techniques and materials Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Bypass grafting techniques and materials US Medical PG Question 2: Three days after undergoing coronary artery bypass surgery, a 72-year-old man has severe right upper quadrant pain, fever, nausea, and vomiting. He has type 2 diabetes mellitus, benign prostatic hyperplasia, peripheral vascular disease, and chronic mesenteric ischemia. He had smoked one pack of cigarettes daily for 30 years but quit 10 years ago. He drinks 8 cans of beer a week. His preoperative medications include metformin, aspirin, simvastatin, and finasteride. His temperature is 38.9°C (102°F), pulse is 102/min, respirations are 18/min, and blood pressure is 110/60 mmHg. Auscultation of the lungs shows bilateral inspiratory crackles. Cardiac examination shows no murmurs, rubs or gallops. Abdominal examination shows soft abdomen with tenderness and sudden inspiratory arrest upon palpation in the right upper quadrant. There is no rebound tenderness or guarding. Laboratory studies show the following:
Hemoglobin 13.1 g/dL
Hematocrit 42%
Leukocyte count 15,700/mm3
Segmented neutrophils 65%
Bands 10%
Lymphocytes 20%
Monocytes 3%
Eosinophils 1%
Basophils 0.5%
AST 40 U/L
ALT 100 U/L
Alkaline phosphatase 85 U/L
Total bilirubin 1.5 mg/dL
Direct 0.9 mg/dL
Amylase 90 U/L
Abdominal ultrasonography shows a distended gallbladder, thickened gallbladder wall with pericholecystic fluid, and no stones. Which of the following is the most appropriate next step in management?
- A. Intravenous heparin therapy followed by embolectomy
- B. Careful observation with serial abdominal examinations
- C. Endoscopic retrograde cholangiopancreatography with papillotomy
- D. Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy (Correct Answer)
- E. Immediate cholecystectomy
Bypass grafting techniques and materials Explanation: ***Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy***
- The patient presents with **acalculous cholecystitis**, characterized by severe RUQ pain, fever, leukocytosis, elevated transaminases, and ultrasonographic findings of a distended gallbladder with a thickened wall and pericholecystic fluid, but no stones.
- Given his comorbid conditions (diabetes, PVD, recent CABG) and the severity of his illness, empirical **broad-spectrum antibiotics** (like piperacillin-tazobactam) along with image-guided **percutaneous cholecystostomy** for gallbladder decompression are the most appropriate management, avoiding the high risks of immediate surgery.
*Intravenous heparin therapy followed by embolectomy*
- This approach is indicated for **acute mesenteric ischemia with embolism**, which can present with severe abdominal pain and signs of hypoperfusion.
- While the patient has chronic mesenteric ischemia, his current symptoms and imaging findings are more consistent with cholecystitis, and there is no clear evidence of acute embolic event requiring embolectomy.
*Careful observation with serial abdominal examinations*
- This patient exhibits signs of a severe inflammatory process (fever, leukocytosis, RUQ tenderness, elevated LFTs, and sonographic findings of severe inflammation) and systemic illness, making **conservative observation insufficient** and potentially dangerous.
- **Acalculous cholecystitis** is a serious condition with a high risk of complications like perforation and sepsis, especially in critically ill patients, and requires prompt intervention.
*Endoscopic retrograde cholangiopancreatography with papillotomy*
- **ERCP with papillotomy** is indicated for conditions like **choledocholithiasis** (common bile duct stones) or **cholangitis**, which cause biliary obstruction.
- The ultrasound shows **no stones** and features specific to cholecystitis rather than common bile duct obstruction, making ERCP inappropriate as an initial step.
*Immediate cholecystectomy*
- While cholecystectomy is the definitive treatment for cholecystitis, immediate open or laparoscopic cholecystectomy in a critically ill patient with **acalculous cholecystitis** after recent CABG carries a **very high morbidity and mortality risk**.
- **Percutaneous cholecystostomy** offers a safer, less invasive alternative for source control and stabilizes the patient before potential delayed definitive surgery if needed, once the patient's condition improves.
Bypass grafting techniques and materials US Medical PG Question 3: In the coronary steal phenomenon, vessel dilation is paradoxically harmful because blood is diverted from ischemic areas of the myocardium. Which of the following is responsible for the coronary steal phenomenon?
- A. Venodilation
- B. Microvessel dilation (Correct Answer)
- C. Dilation of the large coronary arteries
- D. Systemic arterial dilation
- E. Volume loss of fluid in the periphery
Bypass grafting techniques and materials Explanation: ***Microvessel dilation***
- The coronary steal phenomenon occurs when **vasodilators** are administered, causing dilation of **healthy coronary microvessels** and a decrease in resistance.
- This preferentially diverts blood flow away from already **ischemic areas** with maximally dilated intrinsic microvessels, worsening myocardial ischemia.
*Venodilation*
- **Venodilation** primarily reduces **preload** by increasing venous capacitance, not by directly altering coronary microcirculatory blood flow distribution in a way that causes "steal."
- While some vasodilators have venodilatory effects, this specific effect is not the mechanism behind coronary steal.
*Dilation of the large coronary arteries*
- Dilation of large coronary arteries alone doesn't cause the "steal" but rather improves overall blood flow. The critical issue is the differential response of **collateral** and **non-collateral microvessels**.
- **Stenoses** in large coronary arteries are the underlying pathology, but the steal phenomenon itself results from changes in **downstream microvascular resistance**.
*Systemic arterial dilation*
- **Systemic arterial dilation** primarily reduces afterload and can lower blood pressure, but it does not specifically explain the redistribution of coronary blood flow to the detriment of ischemic zones within the myocardium.
- The key to coronary steal is the **heterogeneity of response** at the microvascular level within the coronary circulation.
*Volume loss of fluid in the periphery*
- **Volume loss** in the periphery would influence overall circulatory dynamics and cardiac output but is not directly responsible for the **localized myocardial blood flow redistribution** characteristic of the coronary steal phenomenon.
- Coronary steal is a physiological process related to **vasoreactivity** and not hypovolemia.
Bypass grafting techniques and materials US Medical PG Question 4: A 53-year-old Asian woman comes to the physician because of a 2-month history of severe pain in her right leg while walking. She used to be able to walk a half-mile (800-m) to the grocery store but has been unable to walk 200 meters without stopping because of the pain over the past month. She can continue to walk after a break of around 5 minutes. She has hypertension, atrial fibrillation, and type 2 diabetes mellitus. She has smoked one pack of cigarettes daily for the past 32 years. Current medications include metformin, enalapril, aspirin, and warfarin. Vital signs are within normal limits. Examination shows an irregularly irregular pulse. The right lower extremity is cooler than the left lower extremity. The skin over the right leg appears shiny and dry. Femoral pulses are palpated bilaterally; pedal pulses are diminished on the right side. Which of the following is the most appropriate next step in management?
- A. MRI spine screening
- B. Duplex ultrasonography
- C. Ankle-brachial index (Correct Answer)
- D. Nerve conduction studies
- E. Biopsy of tibial artery
Bypass grafting techniques and materials Explanation: ***Ankle-brachial index***
- The patient's symptoms of **intermittent claudication** (leg pain with exertion relieved by rest) and risk factors (smoking, diabetes, atrial fibrillation, hypertension) are highly suggestive of **peripheral artery disease (PAD)**. The **ankle-brachial index (ABI)** is the most appropriate initial diagnostic step as it is a quick, non-invasive, and reliable test to screen for PAD by comparing blood pressure in the ankles to blood pressure in the arms.
- A **diminished pedal pulse** on the right side and **cooler, shiny, dry skin** further support the suspicion of PAD, making ABI crucial for confirming the diagnosis and assessing its severity.
*MRI spine screening*
- While spinal pathology can cause leg pain, symptoms like **neurogenic claudication** typically improve with leaning forward or sitting and are not consistently relieved by standing still. The patient's pain relief with rest after walking points away from spinal stenosis.
- The patient's specific peripheral signs like a **cooler leg**, **diminished pedal pulses**, and **trophic changes** are not typical findings for spinal compression.
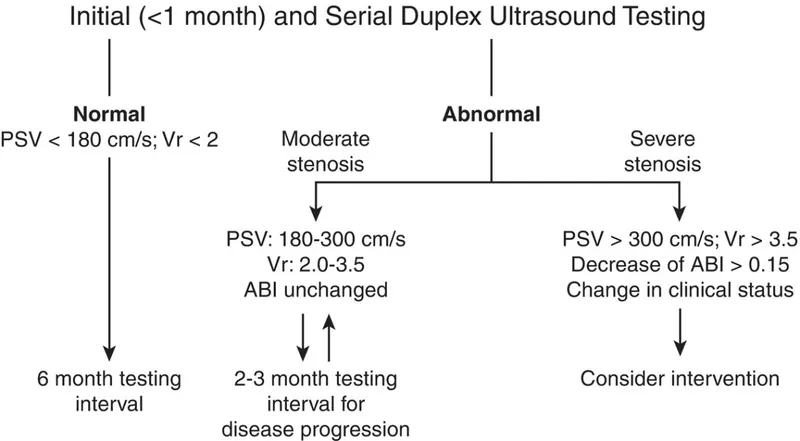
*Duplex ultrasonography*
- **Duplex ultrasonography** is a more advanced imaging technique used to visualize the blood vessels and assess blood flow, typically performed *after* an abnormal ABI confirms the presence of PAD.
- It helps in **localizing stenoses** and assessing their severity, but it is not the primary diagnostic screening tool in the initial evaluation of suspected PAD.
*Nerve conduction studies*
- **Nerve conduction studies (NCS)** are used to diagnose neuropathies. While diabetes is a risk factor for neuropathy, the patient's symptoms are classic for **vascular claudication** (pain with exertion, relieved by rest), rather than neuropathic pain, which is often described as burning, tingling, or numbing and does not typically resolve promptly with rest.
- The physical exam findings of a **cool leg** and **diminished pulses** are not consistent with a primary neurological problem.
*Biopsy of tibial artery*
- A **biopsy of the tibial artery** is an invasive procedure generally reserved for specific types of vasculitis (e.g., giant cell arteritis, polyarteritis nodosa) when other less invasive diagnostics have been inconclusive or raised suspicion for these conditions.
- It is not indicated for the initial workup of suspected **atherosclerotic peripheral artery disease**, which is the most likely diagnosis given the patient's risk factors and symptoms.
Bypass grafting techniques and materials US Medical PG Question 5: A 38-year-old man is brought to the emergency department 35 minutes after he sustained a gunshot wound to the right thigh. He has type 1 diabetes mellitus. On arrival, his pulse is 112/min, respirations are 20/min, and blood pressure is 115/69 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. There is an entrance wound on the anteromedial surface of the right thigh 2 cm below the inguinal ligament. There is no bruit or thrill. There is no exit wound. The pedal pulse is diminished on the right side compared to the left. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hematocrit 46%
Serum
Urea nitrogen 24 mg/dL
Glucose 160 mg/dL
Creatinine 3.1 mg/dL
Which of the following is the most appropriate next step in management?
- A. Digital subtraction angiography
- B. Wound cleaning and tetanus toxoid
- C. CT angiography
- D. Duplex ultrasonography (Correct Answer)
- E. Fasciotomy
Bypass grafting techniques and materials Explanation: ***Duplex ultrasonography***
- The patient has suffered a **gunshot wound** to the thigh with a **diminished pedal pulse**, indicating potential **vascular injury** (a "soft sign" requiring imaging).
- Given his **significantly elevated creatinine (3.1 mg/dL)** and **type 1 diabetes mellitus**, imaging studies requiring **IV iodinated contrast** carry substantial risk for **contrast-induced nephropathy** and further renal deterioration.
- **Duplex ultrasonography** is a **non-invasive, contrast-free method** to assess vascular flow and identify injuries like **arterial dissection**, **thrombosis**, or **pseudoaneurysm**. While operator-dependent, it is the most appropriate initial diagnostic step in this hemodynamically stable patient with significant renal impairment.
- This allows vascular assessment while **minimizing nephrotoxic risk** in a patient with pre-existing renal dysfunction.
*CT angiography*
- **CT angiography** is the **gold standard** for evaluating penetrating extremity trauma with soft signs of vascular injury in most cases, offering rapid and highly accurate vascular imaging.
- However, it requires administration of **intravenous iodinated contrast**, which poses significant risk for **contrast-induced nephropathy** in this patient with **baseline creatinine of 3.1 mg/dL** and **diabetes mellitus**.
- While CTA would typically be preferred in trauma settings, the severe renal impairment makes duplex ultrasonography the safer initial choice in this stable patient.
*Digital subtraction angiography*
- This is an **invasive angiographic technique** that uses **iodinated contrast** and carries even higher contrast load than CTA, posing substantial risk for **contrast-induced nephropathy** given the patient's **elevated creatinine**.
- While it offers high resolution and therapeutic capability, the risks associated with contrast and invasive arterial access outweigh its benefits for initial assessment in this scenario.
- Reserved for cases where intervention is anticipated or non-invasive imaging is inconclusive.
*Wound cleaning and tetanus toxoid*
- These are essential components of wound care for any penetrating injury but do not address the immediate concern of **potential vascular injury** causing the diminished pedal pulse.
- Prioritizing definitive diagnosis of vascular compromise is critical before focusing solely on local wound management, as a missed arterial injury could lead to limb loss.
*Fasciotomy*
- **Fasciotomy** is a surgical procedure to relieve **compartment syndrome**, which can develop secondary to vascular injury, reperfusion, or significant soft tissue trauma.
- While compartment syndrome is a risk with this injury, there is no immediate clinical evidence of it (no severe pain out of proportion to exam, no tense compartments documented).
- Diagnosis of the vascular injury should be established first, as fasciotomy may be needed later if ischemia is prolonged or after revascularization.
Bypass grafting techniques and materials US Medical PG Question 6: A 65-year-old man comes to his primary care physician with a 6-month history of bilateral calf pain. The pain usually occurs after walking his dog a few blocks and is more severe on the right side. He has coronary artery disease, essential hypertension, and type 2 diabetes mellitus. He has smoked two packs of cigarettes daily for 43 years and drinks two alcoholic beverages a day. Current medications include metformin, lisinopril, and aspirin. He is 183 cm (5 ft 11 in) tall and weighs 113 kg (250 lb); BMI is 34.9 kg/m2. His temperature is 37°C (98.6°F), pulse is 84/min, and blood pressure is 129/72 mm Hg. Cardiac examination shows a gallop without murmurs. The legs have shiny skin with reduced hair below the knee. Femoral and popliteal pulses are palpable bilaterally. Dorsal pedal pulses are 1+ on the left and absent on the right. Ankle-brachial index (ABI) is performed in the office. ABI is 0.5 in the right leg, and 0.6 in the left leg. Which of the following is the most appropriate initial step in management?
- A. Propranolol therapy
- B. Graded exercise therapy (Correct Answer)
- C. Vascular bypass surgery
- D. Spinal cord stimulation
- E. Percutaneous transluminal angioplasty with stenting
Bypass grafting techniques and materials Explanation: ***Graded exercise therapy***
- **Graded exercise therapy** is the recommended initial treatment for patients with **intermittent claudication** due to peripheral artery disease (PAD). It improves walking distance and reduces symptoms by promoting collateral circulation and endothelial function.
- This patient's symptoms (bilateral calf pain with exertion, shiny skin, reduced hair, absent dorsal pedal pulse on the right, and low ABI scores) are classic for **PAD with claudication**.
*Propranolol therapy*
- **Propranolol** is a non-selective beta-blocker that can worsen claudication symptoms by inhibiting beta-2 mediated vasodilation in peripheral arteries.
- While beta-blockers may be indicated for some cardiac conditions, they are generally avoided or used cautiously in PAD due to their potential to exacerbate peripheral vasoconstriction.
*Vascular bypass surgery*
- **Vascular bypass surgery** is typically reserved for patients with **severe, limb-threatening ischemia** (critical limb ischemia) or those with claudication that is refractory to conservative management.
- This patient's symptoms, while significant, are consistent with intermittent claudication, which is usually managed initially with lifestyle modifications and exercise.
*Spinal cord stimulation*
- **Spinal cord stimulation** is a treatment option primarily for **refractory chronic neuropathic pain** or **critical limb ischemia** not amenable to revascularization, aiming to reduce pain and potentially improve wound healing.
- It is not an initial treatment for intermittent claudication and doesn't address the underlying vascular obstruction causing claudication.
*Percutaneous transluminal angioplasty with stenting*
- **Percutaneous transluminal angioplasty with stenting** is a revascularization procedure considered when conservative therapies fail to improve claudication or for critical limb ischemia.
- It is not the initial step in management for intermittent claudication. **Lifestyle modifications** and supervised exercise are the first-line treatments.
Bypass grafting techniques and materials US Medical PG Question 7: A 72-year-old woman presents with left lower limb swelling. She first noticed her left leg was swollen about 2 weeks ago. She denies any pain and initially thought the swelling would subside on its own. Past medical history is significant for hypertension and hyperlipidemia. She is a smoker with a 35 pack-year history and an occasional drinker. She takes chlorthalidone, lisinopril, atorvastatin and a multivitamin. On physical examination, her left leg appears larger than her right with 2+ pitting edema up to her knee. She also has a few distended superficial veins along the posterior aspect of her left leg. Lower extremities have 2+ pulses bilaterally. The ultrasound of her left lower thigh and leg shows an obstructing thrombosis of the distal portion of the femoral vein. Which of the following veins serve as collateral pathways to help mitigate the consequences of this patient's condition?
- A. Giacomini vein
- B. Fibular vein
- C. Accessory saphenous vein
- D. Perforator veins (Correct Answer)
- E. Deep femoral vein
Bypass grafting techniques and materials Explanation: ***Perforator veins***
- **Perforator veins** connect the **superficial venous system** to the **deep venous system**, normally allowing blood to flow from superficial to deep veins through one-way valves.
- In cases of **deep vein thrombosis (DVT)**, when the deep venous system is obstructed, these veins can serve as **important collateral pathways**, allowing blood to be rerouted from the obstructed deep system to the superficial system, thereby preventing excessive venous engorgement and helping to reduce severe edema.
- This explains the **distended superficial veins** seen on examination in this patient—blood is being diverted through perforators to the superficial system.
*Giacomini vein*
- The **Giacomini vein** is a **superficial vein** connecting the small saphenous vein to the great saphenous vein, typically in the popliteal fossa and posterior thigh.
- It primarily shunts blood within the **superficial system** and does not provide significant collateral drainage when the deep venous system is occluded.
*Fibular vein*
- The **fibular vein** (also known as the peroneal vein) is a **deep vein** of the lower leg, running alongside the fibula and draining into the posterior tibial veins.
- While it is part of the deep venous system, the thrombosis in this case is in the **femoral vein** (more proximal), so the fibular vein would drain into the same obstructed system rather than serving as a bypass collateral.
*Accessory saphenous vein*
- The **accessory saphenous vein** is a **superficial vein** that runs parallel to and is a tributary of the great saphenous vein in the thigh.
- It is part of the superficial system and does not provide a collateral pathway **from** the obstructed deep system, though it may carry increased flow if perforators are diverting blood to the superficial system.
*Deep femoral vein*
- The **deep femoral vein** (profunda femoris vein) is a **deep vein** that drains the deep compartments of the thigh and joins the common femoral vein.
- While it can provide some collateral drainage when the superficial femoral vein (femoral vein) is occluded, it ultimately drains into the **same deep venous system** proximally and is not the primary collateral mechanism connecting superficial and deep systems.
Bypass grafting techniques and materials US Medical PG Question 8: A 75-year-old man presents to the emergency department because of pain in his left thigh and left calf for the past 3 months. The pain occurs at rest, increases with walking, and is mildly improved by hanging the foot off the bed. He has had hypertension for 25 years and type 2 diabetes mellitus for 30 years. He has smoked 30–40 cigarettes per day for the past 45 years. On examination, femoral, popliteal, and dorsalis pedis pulses are faint on both sides. The patient’s foot is shown in the image. Resting ankle-brachial index (ABI) is found to be 0.30. Antiplatelet therapy and aggressive risk factors modifications are initiated. Which of the following is the best next step for this patient?
- A. Cilostazol
- B. Exercise therapy
- C. Urgent assessment for revascularization (Correct Answer)
- D. Amputation
- E. Systemic anticoagulation with heparin
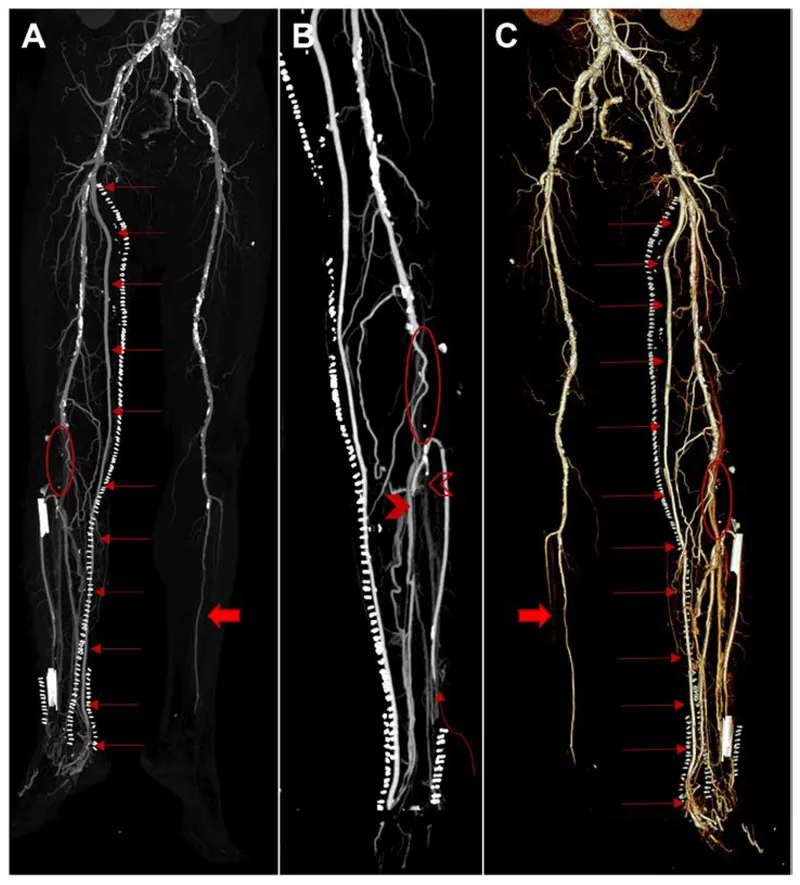
Bypass grafting techniques and materials Explanation: ***Urgent assessment for revascularization***
- The patient presents with **critical limb ischemia (CLI)**, indicated by rest pain, non-healing wounds, and an extremely low ankle-brachial index (ABI) of 0.30. CLI requires urgent revascularization to prevent limb loss.
- The clinical picture (rest pain relieved by dependency, long-standing risk factors like smoking, hypertension, diabetes, and faint pulses) points to severe **peripheral arterial disease (PAD)** that has progressed to a limb-threatening stage.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to improve walking distance in patients with intermittent claudication, but it is **contraindicated in patients with heart failure** and not indicated for critical limb ischemia.
- It is not effective for relieving rest pain or preventing limb loss in severe PAD and would delay necessary definitive treatment.
*Exercise therapy*
- **Supervised exercise therapy** is recommended for patients with intermittent claudication to improve walking distance and quality of life.
- However, for patients with **critical limb ischemia** and rest pain, exercise is typically too painful and not the primary intervention for limb salvage.
*Amputation*
- **Amputation** is a last resort when revascularization attempts have failed or are not feasible, and the limb is unsalvageable or poses an immediate threat to the patient's life.
- It is premature to consider amputation before assessing the possibility of revascularization, which aims to restore blood flow and save the limb.
*Systemic anticoagulation with heparin*
- **Systemic anticoagulation with heparin** is primarily used for acute limb ischemia due to emboli or acute thrombosis, to prevent further clot propagation.
- While this patient has severe PAD, which is a chronic condition, there's no indication of acute arterial occlusion necessitating systemic heparin; the immediate need is to address the chronic severe ischemia via revascularization.
Bypass grafting techniques and materials US Medical PG Question 9: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Bypass grafting techniques and materials Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Bypass grafting techniques and materials US Medical PG Question 10: A 34-year-old woman is brought into the emergency department by emergency medical services after an electrical fire in her apartment. She is coughing with an O2 saturation of 98%, on 2L of nasal cannula. The patient's physical exam is significant for a burn on her right forearm that appears to be dry, white, and leathery in texture. Her pulses and sensations are intact in all extremities. The patient's vitals are HR 110, BP 110/80, T 99.2, RR 20. She has no evidence of soot in her mouth and admits to leaving the room as soon as the fire started. Which of the following is the best treatment for this patient?
- A. Excision and grafting (Correct Answer)
- B. Bacitracin
- C. Amputation
- D. Mafenide acetate
- E. Pain relievers
Bypass grafting techniques and materials Explanation: ***Excision and grafting***
* The burn is described as **dry, white, and leathery**, which are classic features of a **full-thickness (third-degree) burn**.
* Full-thickness burns destroy all skin layers including the dermis, and typically have **loss of sensation** at the burn site due to nerve ending destruction.
* **Excision and grafting** is the definitive treatment for full-thickness burns, involving removal of necrotic tissue and skin grafting to promote healing and prevent infection.
* The patient has intact pulses and sensations in all extremities (indicating no compartment syndrome or vascular compromise), making her a good candidate for this procedure.
*Bacitracin*
* **Bacitracin** is an antibiotic ointment used for **superficial (first-degree) or minor partial-thickness burns**.
* It is insufficient for a **full-thickness burn**, which requires surgical debridement and grafting for proper healing.
*Amputation*
* **Amputation** is reserved for cases of **irreversible tissue damage** with compromised vascularity, extensive non-viable tissue, or severe crush injuries.
* This patient has **intact pulses and sensations in all extremities**, indicating the limb is viable and perfused, making amputation inappropriate.
*Mafenide acetate*
* **Mafenide acetate** is a topical antimicrobial agent that penetrates eschar and can be used for deep burns to prevent infection.
* While useful as adjunctive therapy, it does **not replace the need for surgical excision and grafting**, which is the definitive treatment for full-thickness burns.
*Pain relievers*
* **Pain relievers** are important supportive care for burn patients but are **not definitive treatment**.
* They manage symptoms but do not address the underlying need for debridement and wound closure through grafting.
More Bypass grafting techniques and materials US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.