Aortic dissection management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aortic dissection management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aortic dissection management US Medical PG Question 1: A 58-year-old man is brought to the emergency department by his family because of severe upper back pain, which he describes as ripping. The pain started suddenly 1 hour ago while he was watching television. He has hypertension for 13 years, but he is not compliant with his medications. He denies the use of nicotine, alcohol or illicit drugs. His temperature is 36.5°C (97.7°F), the heart rate is 110/min and the blood pressure is 182/81 mm Hg in the right arm and 155/71 mm Hg in the left arm. CT scan of the chest shows an intimal flap limited to the descending aorta. Intravenous opioid analgesia is started. Which of the following is the best next step in the management of this patient condition?
- A. Intravascular ultrasound
- B. Emergency surgical intervention
- C. Sublingual nitroglycerin
- D. Intravenous esmolol (Correct Answer)
- E. Oral metoprolol and/or enalapril
Aortic dissection management Explanation: ***Intravenous esmolol***
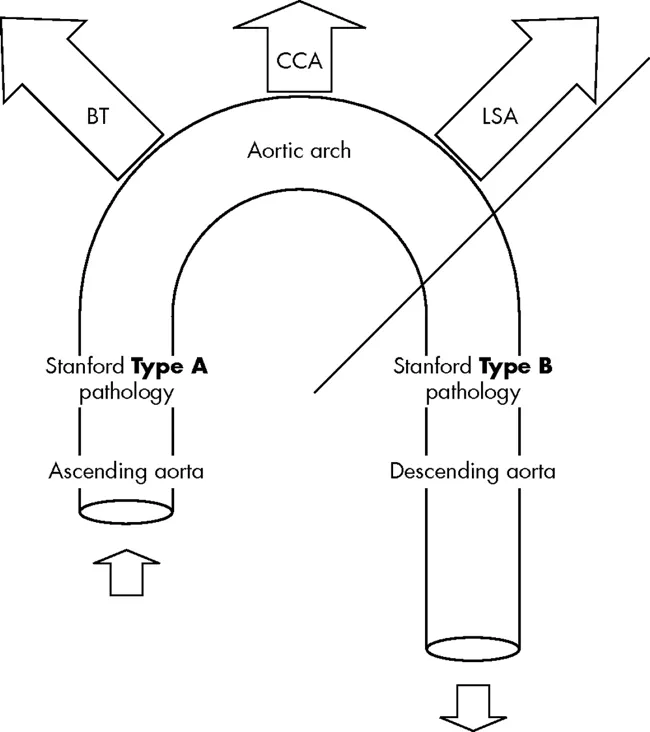
- This patient presents with an **acute aortic dissection** (descending aorta, Type B), characterized by sudden severe ripping back pain and a significant blood pressure difference between the arms [1]. The immediate priority is to reduce **heart rate** and **blood pressure** to decrease shear stress on the aortic wall and prevent progression of the dissection.
- **Intravenous beta-blockers** like esmolol are the first-line medical treatment for uncomplicated Type B aortic dissections, as they rapidly decrease heart rate and blood pressure, which helps to mitigate further aortic injury.
*Intravascular ultrasound*
- While intravascular ultrasound can provide detailed imaging of the aorta, it is an **invasive procedure** and not the immediate next step in managing an acute, hemodynamically unstable condition like aortic dissection where rapid blood pressure control is paramount.
- The patient already has a diagnostic CT scan confirming the intimal flap; thus, additional imaging during the acute stabilization phase is not typically the first priority over medical management [2].
*Emergency surgical intervention*
- **Emergency surgical intervention** is primarily indicated for **Type A aortic dissections** (involving the ascending aorta) or for complicated Type B dissections (e.g., malperfusion, rupture, rapid expansion) [1].
- This patient has an **uncomplicated Type B dissection** (limited to the descending aorta) that is initially managed medically with aggressive heart rate and blood pressure control.
*Sublingual nitroglycerin*
- **Nitroglycerin** primarily causes **vasodilation**, which can lower blood pressure but also induces reflex tachycardia, potentially increasing shear stress on the dissected aorta.
- It is **contraindicated** in acute aortic dissection as the increase in heart rate can worsen the dissection.
*Oral metoprolol and/or enalapril*
- **Oral medications** like metoprolol and enalapril are not suitable for the **initial acute management** of aortic dissection because their onset of action is too slow to achieve rapid and precise control of heart rate and blood pressure.
- **Intravenous agents** are required for immediate and titratable blood pressure and heart rate reduction in this emergency setting.
Aortic dissection management US Medical PG Question 2: A 55-year-old man is brought to the emergency department 30 minutes after the sudden onset of severe, migrating anterior chest pain, shortness of breath, and sweating at rest. He has hypertension, hypercholesterolemia, and type 2 diabetes mellitus. Medications include atorvastatin, hydrochlorothiazide, lisinopril, and metformin. He has smoked one pack of cigarettes daily for 25 years. He is in severe distress. His pulse is 110/min, respirations are 20/min, and blood pressure is 150/85 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Cardiac examination shows a grade 3/6, high-pitched, blowing, diastolic murmur heard best over the right sternal border. The lungs are clear to auscultation. Femoral pulses are decreased bilaterally. An ECG shows sinus tachycardia and left ventricular hypertrophy. Which of the following is the most likely diagnosis?
- A. Esophageal rupture
- B. Pulmonary embolism
- C. Aortic dissection (Correct Answer)
- D. Papillary muscle rupture
- E. Spontaneous pneumothorax
Aortic dissection management Explanation: ***Aortic dissection***
- The sudden onset of **severe, migrating anterior chest pain**, autonomic symptoms (sweating at rest), and **decreased bilateral femoral pulses** are highly characteristic of aortic dissection.
- The presence of a new **diastolic murmur** (indicating aortic insufficiency due to dissection extending to the aortic valve), along with a history of **hypertension** and **smoking**, further supports this diagnosis.
- **Decreased bilateral femoral pulses** suggest involvement of the descending aorta compromising flow to both lower extremities.
*Esophageal rupture*
- While esophageal rupture can cause **sudden, severe chest pain**, it typically presents with **odynophagia**, **vomiting**, and often **subcutaneous emphysema** or **Hamman's sign**, which are absent here.
- It would not explain the **diastolic murmur** or the **bilateral decreased femoral pulses**.
*Pulmonary embolism*
- **Shortness of breath** and **chest pain** can occur with pulmonary embolism, but the pain is typically **pleuritic** rather than migrating.
- It would not cause a **diastolic murmur** or **decreased peripheral pulses**.
*Papillary muscle rupture*
- Papillary muscle rupture is a complication of **myocardial infarction**, usually causing **acute severe mitral regurgitation** with a new **systolic murmur** and signs of **heart failure**.
- The patient's presentation with migrating pain and a **diastolic murmur** is inconsistent with this diagnosis.
*Spontaneous pneumothorax*
- A spontaneous pneumothorax causes **sudden, sharp, pleuritic chest pain** and **dyspnea**, often accompanied by **decreased breath sounds** on the affected side.
- It would not cause a **diastolic murmur** or **decreased femoral pulses**.
Aortic dissection management US Medical PG Question 3: A 43-year-old man is brought to the emergency department because of severe retrosternal pain radiating to the back and left shoulder for 4 hours. The pain began after attending a farewell party for his coworker at a local bar. He had 3–4 episodes of nonbilious vomiting before the onset of the pain. He has hypertension. His father died of cardiac arrest at the age of 55 years. He has smoked one pack of cigarettes daily for the last 23 years and drinks 2–3 beers daily. His current medications include amlodipine and valsartan. He appears pale. His temperature is 37° C (98.6° F), pulse is 115/min, and blood pressure is 90/60 mm Hg. There are decreased breath sounds over the left base and crepitus is palpable over the thorax. Abdominal examination shows tenderness to palpation in the epigastric region; bowel sounds are normal. Laboratory studies show:
Hemoglobin 16.5 g/dL
Leukocyte count 11,100/mm3
Serum
Na+ 133 mEq/L
K+ 3.2 mEq/L
Cl- 98 mEq/L
HCO3- 30 mEq/L
Creatinine 1.4 mg/dL
An ECG shows sinus tachycardia with left ventricular hypertrophy. Intravenous fluid resuscitation and antibiotics are begun. Which of the following is the most appropriate test to confirm the diagnosis in this patient?
- A. Aortography
- B. Transthoracic echocardiography
- C. Abdominal ultrasound
- D. CT scan of the chest (Correct Answer)
- E. Esophagogastroduodenoscopy
Aortic dissection management Explanation: ***CT scan of the chest***
- This patient's presentation of **severe retrosternal pain after forceful vomiting** (Mackler's triad: vomiting, chest pain, subcutaneous emphysema) strongly suggests **Boerhaave syndrome** (spontaneous esophageal perforation).
- The presence of **subcutaneous crepitus** (indicating pneumomediastinum) and **decreased breath sounds** (pleural effusion) are key findings.
- **CT scan of the chest with oral contrast is the gold standard** for diagnosing esophageal perforation, demonstrating **pneumomediastinum, pleural effusion, esophageal wall thickening**, and extravasation of contrast.
- CT is **highly sensitive (>90%) and specific**, non-invasive, and provides comprehensive evaluation of the mediastinum and pleural spaces.
*Esophagogastroduodenoscopy*
- While EGD can directly visualize esophageal mucosa, it is **relatively contraindicated** in suspected acute esophageal perforation.
- Insufflation during endoscopy risks **extending the perforation** and worsening mediastinal contamination.
- EGD may be considered after CT confirmation for therapeutic intervention or if diagnosis remains unclear, but is **not the initial confirmatory test**.
*Aortography*
- **Aortography** is used to diagnose aortic dissection, which can present with retrosternal pain radiating to the back.
- However, aortic dissection typically presents with **sudden tearing pain** without preceding vomiting, and would not explain the **crepitus** or timing after vomiting episodes.
- The clinical picture here is classic for esophageal perforation, not aortic pathology.
*Transthoracic echocardiography*
- **TTE** is useful for cardiac evaluation and can detect some aortic pathologies or pericardial effusion.
- It **cannot visualize the esophagus or mediastinum** adequately to diagnose esophageal perforation.
- While useful in ruling out cardiac causes of chest pain, it does not address the primary diagnosis suggested by this presentation.
*Abdominal ultrasound*
- **Abdominal ultrasound** evaluates intra-abdominal organs and free fluid but **cannot assess the esophagus or mediastinum**.
- It would miss the diagnosis of esophageal perforation entirely, as the pathology is located in the **thorax**, not the abdomen.
- Not useful for this clinical presentation despite epigastric tenderness.
Aortic dissection management US Medical PG Question 4: In a routine medical examination, a young man is noted to be tall with slight scoliosis and pectus excavatum. He had been told that he was over the 95% percentile for height as a child. Auscultation reveals a heart murmur, and transthoracic echocardiography shows an enlarged aortic root and mitral valve prolapse. Blood screening for fibrillin-1 (FBN1) gene mutation is positive and plasma homocysteine is normal. This patient is at high risk for which of the following complications?
- A. Intravascular thrombosis
- B. Infertility
- C. Aortic dissection (Correct Answer)
- D. Spontaneous pneumothorax
- E. Mucosal neuromas
Aortic dissection management Explanation: ***Aortic dissection***
- The constellation of **tall stature**, **scoliosis**, **pectus excavatum**, **enlarged aortic root**, **mitral valve prolapse**, and a **positive FBN1 gene mutation** is highly indicative of **Marfan syndrome**.
- **Aortic dissection** is the most life-threatening complication of Marfan syndrome due to the weakened connective tissue in the aortic wall, a direct consequence of the FBN1 mutation affecting fibrillin-1 protein.
- Patients with Marfan syndrome require regular cardiovascular surveillance and prophylactic beta-blocker therapy to reduce aortic wall stress.
*Intravascular thrombosis*
- This complication is more characteristic of conditions like **homocystinuria**, which is ruled out by the **normal plasma homocysteine** level.
- Marfan syndrome primarily affects connective tissue strength, not coagulation pathways or endothelial function.
*Infertility*
- Marfan syndrome does not inherently cause **infertility** in males or females.
- The primary health risks for Marfan patients are cardiovascular, musculoskeletal, and ophthalmologic (lens dislocation).
*Spontaneous pneumothorax*
- While **spontaneous pneumothorax** can occur in Marfan syndrome due to apical blebs and weakened pleural tissue, it is far less immediately life-threatening than aortic dissection.
- The question asks for the "high risk" complication, and cardiovascular complications (particularly aortic dissection and rupture) are the leading cause of mortality in Marfan syndrome.
*Mucosal neuromas*
- **Mucosal neuromas** are characteristic of **Multiple Endocrine Neoplasia type 2B (MEN2B)**, not Marfan syndrome.
- MEN2B involves RET proto-oncogene mutations and is associated with medullary thyroid cancer, pheochromocytoma, and a marfanoid habitus, which can be mistaken for Marfan syndrome.
Aortic dissection management US Medical PG Question 5: A 55-year-old man presents to the emergency department for chest pain. He states that the pain started last night and has persisted until this morning. He describes the pain as in his chest and radiating into his back between his scapulae. The patient has a past medical history of alcohol abuse and cocaine abuse. He recently returned from vacation on a transatlantic flight. The patient has smoked 1 pack of cigarettes per day for the past 20 years. His temperature is 99.5°F (37.5°C), blood pressure is 167/118 mmHg, pulse is 120/min, and respirations are 22/min. Physical exam reveals tachycardia and clear air movement bilaterally on cardiopulmonary exam. Which of the following is also likely to be found in this patient?
- A. Pulmonary artery thrombus
- B. Coronary artery thrombus
- C. Elevated lipase
- D. Asymmetric blood pressures in the upper extremities (Correct Answer)
- E. Coronary artery vasospasm
Aortic dissection management Explanation: ***Asymmetric blood pressures in the upper extremities***
- The patient's presentation with **sudden-onset, severe, tearing chest pain radiating to the back**, combined with **hypertension** and **tachycardia**, is highly suggestive of an **aortic dissection**. Asymmetric blood pressures are a classic sign.
- Aortic dissection involves a tear in the intima of the aorta, leading to a false lumen that can compress branch arteries, causing **pulse deficits** or **limb ischemia**, resulting in pressure differences.
*Pulmonary artery thrombus*
- While a **transatlantic flight** is a risk factor for **pulmonary embolism (PE)**, the described chest pain is typically pleuritic and not usually severe or radiating to the back in this manner.
- PE often presents with **dyspnea** and **hypoxia**, which are not prominent features described here.
*Coronary artery thrombus*
- **Cocaine abuse**, **smoking**, and **hypertension** are risk factors for **myocardial infarction (MI)** due to **coronary artery thrombosis**. However, MI pain is typically crushing or constricting, and radiation to the back between the scapulae is less common than in dissection.
- The description of **tearing pain** is more characteristic of aortic dissection than MI.
*Elevated lipase*
- The patient's history of **alcohol abuse** and **cocaine abuse** are risk factors for **pancreatitis**, which presents with elevated lipase. However, pancreatitis pain is typically **epigastric** and radiates to the back, but it's usually steady, severe, and often associated with nausea/vomiting, not the tearing quality described.
- The acute, severe, radiating chest pain pattern is not typical for an initial presentation of pancreatitis.
*Coronary artery vasospasm*
- **Cocaine abuse** is a known trigger for **coronary artery vasospasm**, leading to angina or MI, and can cause chest pain.
- However, the pain from vasospasm is usually anginal in quality, often responsive to nitrates, and less likely to present with the severe, tearing, interscapular back pain and hemodynamic instability suggestive of aortic dissection.
Aortic dissection management US Medical PG Question 6: A 58-year-old man presents to the emergency department for evaluation of intermittent chest pain over the past 6 months. His history reveals that he has had moderate exertional dyspnea and 2 episodes of syncope while working at his factory job. These episodes of syncope were witnessed by others and lasted roughly 30 seconds. The patient states that he did not have any seizure activity. His vital signs include: blood pressure 121/89 mm Hg, heart rate 89/min, temperature 37.0°C (98.6°F), and respiratory rate 16/min. Physical examination reveals a crescendo-decrescendo systolic murmur in the right second intercostal area. An electrocardiogram is performed, which shows left ventricular hypertrophy. Which of the following is the best next step for this patient?
- A. Transthoracic echocardiography (Correct Answer)
- B. Chest radiograph
- C. Computed tomography (CT) chest scan without contrast
- D. Cardiac chamber catheterization
- E. Transesophageal echocardiography
Aortic dissection management Explanation: ***Transthoracic echocardiography***
- The patient's symptoms (chest pain, exertional dyspnea, syncope) and physical exam findings (**crescendo-decrescendo systolic murmur at the right second intercostal space**, ECG showing **left ventricular hypertrophy**) are highly suggestive of **aortic stenosis**.
- **Transthoracic echocardiography** is the gold standard for diagnosing and assessing the severity of valvular heart diseases like aortic stenosis, quantifying valve area, pressure gradients, and ventricular function.
*Chest radiograph*
- A chest radiograph provides information about lung fields, cardiac size, and aortic calcification, but it cannot directly visualize or assess the function of heart valves.
- While it may show signs of heart failure (e.g., **pulmonary congestion**) or **cardiomegaly**, it is insufficient for a definitive diagnosis or severity assessment of valvular lesions.
*Computed tomography (CT) chest scan without contrast*
- A CT scan can detect calcification of the aortic valve, but it is not the primary imaging modality for assessing valvular function or the severity of stenotic lesions.
- CT is more useful for evaluating the **aorta for aneurysm** or dissection, or for **pulmonary pathology**, neither of which is the most likely diagnosis given the presenting symptoms.
*Cardiac chamber catheterization*
- Cardiac catheterization is an **invasive procedure** that is typically reserved for cases where non-invasive imaging is inconclusive or when planning for intervention (e.g., prior to valve replacement).
- It involves risks and is not the initial best step for diagnosis when a less invasive and highly informative test like echocardiography is available.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** provides more detailed images of the heart and valves compared to TTE because it avoids acoustic shadowing from the ribs and lungs.
- However, TEE is more invasive than TTE and is usually reserved for situations where TTE is inadequate or when a higher resolution view is needed, such as for infective endocarditis, prosthetic valve dysfunction, or before/during surgical procedures.
Aortic dissection management US Medical PG Question 7: A 62-year-old man presents to the emergency department with chest pain. He was at home watching television when he suddenly felt chest pain that traveled to his back. The patient has a past medical history of alcoholism, obesity, hypertension, diabetes, and depression. His temperature is 98.4°F (36.9°C), blood pressure is 177/118 mmHg, pulse is 123/min, respirations are 14/min, and oxygen saturation is 97% on room air. Physical exam reveals a S4 on cardiac exam and chest pain that seems to worsen with palpation. The patient smells of alcohol. The patient is started on 100% oxygen and morphine. Which of the following is the best next step in management?
- A. NPO, IV fluids, serum lipase
- B. Nitroprusside
- C. Labetalol (Correct Answer)
- D. Aspirin
- E. CT scan
Aortic dissection management Explanation: ***Labetalol***
- This patient's presentation with **sudden-onset chest pain radiating to the back**, **hypertension**, **tachycardia**, and a history of uncontrolled hypertension strongly suggests **aortic dissection**.
- **Labetalol** is an ideal initial step to rapidly reduce both heart rate and blood pressure, which is crucial in preventing further extension of the dissection.
*NPO, IV fluids, serum lipase*
- While **alcoholism** is a risk factor for **pancreatitis**, the classic presentation of **sudden-onset chest pain radiating to the back** with **severe hypertension** is not typical for pancreatitis.
- Although ruling out pancreatitis might be considered later, it's not the immediate priority over stabilizing a suspected dissection.
*Nitroprusside*
- **Nitroprusside** is a powerful vasodilator that lowers blood pressure but does not adequately control the **heart rate**.
- In **aortic dissection**, isolated blood pressure reduction without concomitant heart rate control can increase **shear stress** on the aortic wall, potentially worsening the dissection.
*Aspirin*
- **Aspirin** is used in the management of **acute coronary syndromes** to prevent platelet aggregation.
- In a suspected **aortic dissection**, aspirin is **contraindicated** as it can increase the risk of bleeding if surgical intervention is required.
*CT scan*
- A **CT scan** of the chest is the diagnostic test of choice for **aortic dissection** and would be performed soon.
- However, the **initial management priority** is to stabilize the patient hemodynamically by reducing heart rate and blood pressure *before* proceeding with imaging to prevent further aortic injury.
Aortic dissection management US Medical PG Question 8: A 59-year-old man is brought to the emergency department by paramedics following a high-speed motor vehicle collision. The patient complains of excruciating chest pain, which he describes as tearing. Further history reveals that the patient is healthy, taking no medications, and is not under the influence of drugs or alcohol. On physical examination, his heart rate is 97/min. His blood pressure is 95/40 mm Hg in the right arm and 60/30 mm Hg in the left arm. Pulses are absent in the right leg and diminished in the left. A neurological examination is normal. A chest X-ray reveals a widened mediastinum. Which of the following is the most likely etiology of this patient's condition?
- A. Myocardial rupture
- B. Diaphragmatic rupture
- C. Traumatic aortic dissection (Correct Answer)
- D. Rib fracture
- E. Pulmonary contusion
Aortic dissection management Explanation: ***Traumatic aortic dissection***
- The patient's **"tearing" chest pain**, profound **blood pressure differential** between arms, **absent/diminished pulses** in the legs, and a **widened mediastinum** on chest X-ray immediately after a high-speed collision are classic signs of a traumatic aortic dissection.
- The tearing pain, pulse deficits, and widened mediastinum collectively point to a catastrophic vascular injury, most commonly involving the **descending aorta** in trauma.
*Myocardial rupture*
- Myocardial rupture typically presents with sudden cardiac collapse, **pericardial tamponade**, and profound shock, which might be similar, but it would not explain the **pulse deficits** or the **widened mediastinum**.
- While a high-speed collision can cause myocardial contusion, a full rupture leading to hemodynamic instability would usually present differently than the described pulse deficits.
*Diaphragmatic rupture*
- Diaphragmatic rupture would typically present with respiratory distress, **herniation of abdominal contents** into the chest, and potentially muffled breath sounds on the affected side.
- It does not explain the asymmetrical blood pressures, pulse deficits, or the classic "tearing" chest pain related to a vascular event.
*Rib fracture*
- Rib fractures cause localized chest pain, which is usually exacerbated by breathing and movement, but they do not account for the systemic signs like **blood pressure discrepancies**, **pulse deficits**, or a **widened mediastinum**.
- While common in trauma, rib fractures alone are not life-threatening unless they lead to complications like pneumothorax or hemothorax, which are not suggested by the findings.
*Pulmonary contusion*
- Pulmonary contusion involves bruising of the lung tissue, leading to localized pain, **hemoptysis**, and **hypoxia**, often visible as infiltrates on chest imaging.
- This condition would not explain the **tearing pain**, **blood pressure differential**, **pulse deficits**, or the **widened mediastinum**, which are indicative of a major vascular injury.
Aortic dissection management US Medical PG Question 9: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Aortic dissection management Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Aortic dissection management US Medical PG Question 10: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Aortic dissection management Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
More Aortic dissection management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.