Acute limb ischemia management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute limb ischemia management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute limb ischemia management US Medical PG Question 1: A 65-year-old man is referred by his primary care provider to a neurologist for leg pain. He reports a 6-month history of progressive bilateral lower extremity pain that is worse in his left leg. The pain is 5/10 in severity at its worst and is described as a "burning" pain. He has noticed that the pain is acutely worse when he walks downhill. He has started riding his stationary bike more often as it relieves his pain. His past medical history is notable for hypertension, diabetes mellitus, and a prior myocardial infarction. He also sustained a distal radius fracture the previous year after falling on his outstretched hand. He takes aspirin, atorvastatin, metformin, glyburide, enalapril, and metoprolol. He has a 30-pack-year smoking history and drinks 2-3 glasses of wine with dinner every night. His temperature is 99°F (37.2°C), blood pressure is 145/85 mmHg, pulse is 91/min, and respirations are 18/min. On exam, he is well-appearing and in no acute distress. A straight leg raise is negative. A valsalva maneuver does not worsen his pain. Which of the following is the most appropriate test to confirm this patient's diagnosis?
- A. Electromyography
- B. Ankle-brachial index
- C. Computerized tomography myelography
- D. Magnetic resonance imaging (Correct Answer)
- E. Radiography
Acute limb ischemia management Explanation: **Magnetic resonance imaging**
- **Magnetic resonance imaging (MRI)** is the most appropriate test for diagnosing **lumbar spinal stenosis** because it provides detailed imaging of soft tissues, including the **spinal cord, nerve roots, and intervertebral discs**.
- The patient's symptoms of bilateral lower extremity pain, worse with downhill walking and relieved by stationary biking (which typically involves a flexed spine), are classic for **neurogenic claudication** caused by spinal stenosis.
*Electromyography*
- **Electromyography (EMG)** measures electrical activity of muscles and can identify **radiculopathy** or **neuropathy** but does not directly visualize the spinal canal or its contents to diagnose the cause of nerve compression.
- While it could show nerve root involvement, it wouldn't be the primary diagnostic test to confirm **spinal stenosis** itself.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is used to diagnose **peripheral artery disease (PAD)**, which can also cause leg pain with activity (**vascular claudication**).
- However, the patient's pain being worse with downhill walking and relieved by spine flexion (like on a stationary bike) is more consistent with **neurogenic claudication** than vascular claudication.
*Computerized tomography myelography*
- **CT myelography** involves injecting contrast into the spinal canal and then performing a CT scan. While it can visualize the spinal canal, it is more invasive than MRI and exposes the patient to **ionizing radiation**.
- It is typically reserved for cases where MRI is contraindicated (e.g., pacemakers) or when MRI findings are inconclusive.
*Radiography*
- **Radiography (X-rays)** can show bony changes such as **spondylosis** and **degenerative disc disease**, which are often associated with spinal stenosis.
- However, X-rays do not directly visualize the **spinal cord, nerve roots, or soft tissue compression**, making them inadequate for confirming spinal stenosis as the cause of neurogenic claudication.
Acute limb ischemia management US Medical PG Question 2: A 20-year-old woman is brought to the emergency department because of severe muscle soreness, nausea, and darkened urine for 2 days. The patient is on the college track team and has been training intensively for an upcoming event. One month ago, she had a urinary tract infection and was treated with nitrofurantoin. She appears healthy. Her temperature is 37°C (98.6°F), pulse is 64/min, and blood pressure is 110/70 mm Hg. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and non-tender. There is diffuse muscle tenderness over the arms, legs, and back. Laboratory studies show:
Hemoglobin 12.8 g/dL
Leukocyte count 7,000/mm3
Platelet count 265,000/mm3
Serum
Creatine kinase 22,000 U/L
Lactate dehydrogenase 380 U/L
Urine
Blood 3+
Protein 1+
RBC negative
WBC 1–2/hpf
This patient is at increased risk for which of the following complications?
- A. Myocarditis
- B. Metabolic alkalosis
- C. Compartment syndrome
- D. Acute kidney injury (Correct Answer)
- E. Hemolytic anemia
Acute limb ischemia management Explanation: ***Acute kidney injury***
- The patient's elevated **creatine kinase (CK)** of 22,000 U/L, muscle soreness, and dark urine (positive for blood but negative for red blood cells) are all indicative of **rhabdomyolysis**.
- **Rhabdomyolysis** releases large amounts of myoglobin, which is nephrotoxic and can precipitate in the renal tubules, leading to **acute tubular necrosis** and subsequent acute kidney injury.
*Myocarditis*
- While CK elevations can be seen in myocarditis, this patient's presentation is dominated by **skeletal muscle symptoms** and a history of intense exercise.
- There are no specific cardiac symptoms or signs (e.g., chest pain, arrhythmias) to suggest myocardial involvement.
*Metabolic alkalosis*
- Rhabdomyolysis typically causes **metabolic acidosis** due to the release of cellular contents, including phosphate and sulfate.
- There is no clinical or lab evidence (e.g., vomiting, diuretic use) to suggest metabolic alkalosis.
*Compartment syndrome*
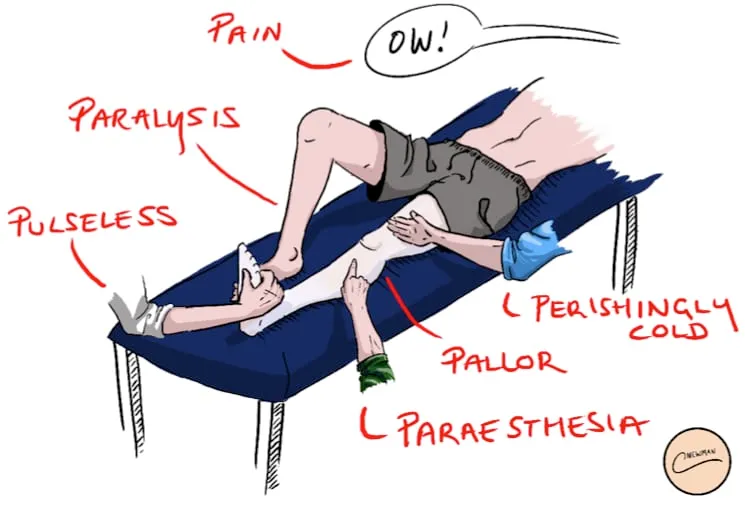
- **Compartment syndrome** involves increased pressure within a muscle compartment, leading to pain, pallor, paresthesia, pulselessness, and paralysis.
- While rhabdomyolysis can occasionally lead to severe swelling that causes compartment syndrome, the diffuse muscle tenderness and absence of focal limb findings make it less likely as the primary direct complication.
*Hemolytic anemia*
- Though the urine is positive for blood and negative for RBCs, this is characteristic of **myoglobinuria**, not hemoglobinuria, which would indicate hemolytic anemia.
- The patient's **hemoglobin** is normal (12.8 g/dL), and there are no other signs of hemolysis (e.g., jaundice, reticulocytosis).
Acute limb ischemia management US Medical PG Question 3: A 54-year-old man comes to the emergency department because of severe pain in his right leg that began suddenly 3 hours ago. He has had repeated cramping in his right calf while walking for the past 4 months, but it has never been this severe. He has type 2 diabetes mellitus, hypercholesterolemia, and hypertension. Current medications include insulin, enalapril, aspirin, and simvastatin. He has smoked one pack of cigarettes daily for 33 years. He does not drink alcohol. His pulse is 103/min and blood pressure is 136/84 mm Hg. Femoral pulses are palpable bilaterally. The popliteal and pedal pulses are absent on the right. Laboratory studies show:
Hemoglobin 16.1 g/dL
Serum
Urea nitrogen 14 mg/dL
Glucose 166 mg/dL
Creatinine 1.5 mg/dL
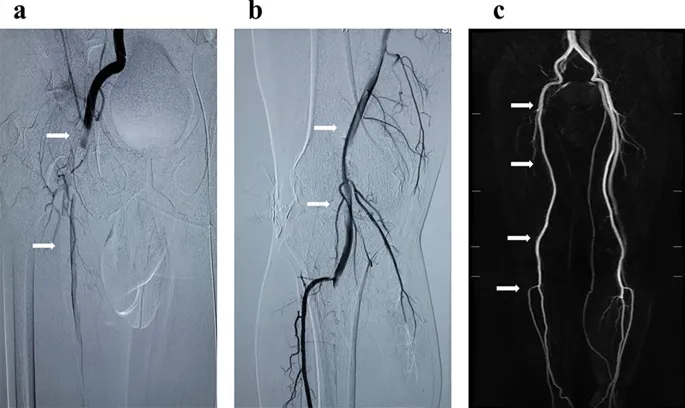
A CT angiogram of the right lower extremity is ordered. Which of the following is the most appropriate next step in management?
- A. Administer sodium bicarbonate
- B. Administer mannitol
- C. Administer normal saline (Correct Answer)
- D. Remote ischemic preconditioning
- E. Administer heparin anticoagulation
Acute limb ischemia management Explanation: ***Administer normal saline***
- The patient has an acute limb ischemia and needs a **CT angiogram** with contrast to locate the thrombus for intervention. Administering **normal saline** prior to contrast administration is crucial to prevent contrast-induced nephropathy, especially in a patient with **diabetes** and mildly elevated **creatinine**.
- **Aggressive hydration** with intravenous fluids helps maintain renal perfusion and dilute the contrast agent, thereby reducing its nephrotoxic effects.
*Administer sodium bicarbonate*
- While sometimes used for renal protection, **sodium bicarbonate** is generally reserved for patients with more severe metabolic acidosis or for specific situations where its alkalizing properties are beneficial.
- In this context, **normal saline** is the primary choice for generalized hydration and prevention of contrast-induced nephropathy before contrast administration.
*Administer mannitol*
- **Mannitol** is an osmotic diuretic used to induce diuresis and reduce intracranial pressure or treat cerebral edema.
- It is **not the primary fluid** for preventing contrast-induced nephropathy and could potentially worsen dehydration if used inappropriately.
*Remote ischemic preconditioning*
- **Remote ischemic preconditioning** involves inducing brief, controlled periods of ischemia and reperfusion in one organ to protect another organ from a subsequent, more prolonged ischemic insult.
- While an interesting concept, it is **not a standard or immediate treatment** for preventing contrast-induced nephropathy in this acute setting and has not shown consistent, strong evidence for this specific indication.
*Administer heparin anticoagulation*
- **Heparin anticoagulation** is critical for treating acute limb ischemia to prevent thrombus propagation. However, the question specifically asks for the most appropriate next step **in management regarding the CT angiogram**.
- While heparin should be given, **renal protection** prior to contrast administration is a more immediate and specific concern related to the ordered diagnostic test. The question asks for the step **before** the CT angiogram.
Acute limb ischemia management US Medical PG Question 4: Two days after undergoing emergency cardiac catherization for myocardial infarction, a 68-year-old woman has pain in her toes. During the intervention, she was found to have an occluded left anterior descending artery and 3 stents were placed. She has hypertension, hypercholesterolemia, and coronary artery disease. Prior to admission, her medications were metoprolol, enalapril, atorvastatin, and aspirin. Her temperature is 37.3°C (99.1°F), pulse is 93/min, and blood pressure is 115/78 mm Hg. Examination shows discoloration of the toes of both feet. A photograph of the right foot is shown. The lesions are cool and tender to palpation. The rest of the skin on the feet is warm; femoral and pedal pulses are palpable bilaterally. This patient is at increased risk for which of the following conditions?
- A. Acute kidney injury (Correct Answer)
- B. Migratory thrombophlebitis
- C. Basophilia
- D. Permanent flexion contracture
- E. Lipodermatosclerosis
Acute limb ischemia management Explanation: ***Acute kidney injury***
- This patient's presentation of painful, discolored, cool toes with palpable pulses (suggesting microembolism rather than large vessel occlusion) following cardiac catheterization is highly suggestive of **cholesterol atheroembolism**. This condition commonly leads to **acute kidney injury** as cholesterol crystals dislodge from atheromatous plaques and embolize to renal arteries.
- The risk of acute kidney injury is significant in cholesterol atheroembolism due to widespread microvascular occlusion in the kidneys, leading to **ischemic damage** and **renal dysfunction**.
*Migratory thrombophlebitis*
- **Migratory thrombophlebitis** (Trousseau's sign) is characterized by recurrent, migratory episodes of superficial venous thrombosis, often associated with underlying malignancy.
- It would present with **palpable, tender, cord-like veins** typically in the extremities, rather than multifocal discoloration of the toes.
*Basophilia*
- While **eosinophilia** is often associated with cholesterol atheroembolism due to the inflammatory response to cholesterol crystals, **basophilia** (an increase in basophils) is not a typical finding or complication.
- Basophilia can be seen in myeloproliferative disorders or allergic reactions, which are not suggested by this clinical picture.
*Permanent flexion contracture*
- A permanent flexion contracture is a **fixed deformation** of a joint, preventing full extension. It is typically caused by chronic inflammation, muscle imbalances, or prolonged immobilization.
- This is a long-term orthopedic complication that would not develop acutely **2 days after a cardiac catheterization** or be directly related to microembolism.
*Lipodermatosclerosis*
- **Lipodermatosclerosis** is a localized chronic inflammation and thickening of the skin and subcutaneous tissue, typically in the lower legs, associated with **chronic venous insufficiency**.
- It presents with **brawny edema**, hyperpigmentation, and inverted champagne bottle appearance of the leg, which is distinctly different from the acute painful toe discoloration seen here.
Acute limb ischemia management US Medical PG Question 5: A 68-year-old man presents to the emergency department with leg pain. He states that the pain started suddenly while he was walking outside. The patient has a past medical history of diabetes, hypertension, obesity, and atrial fibrillation. His temperature is 99.3°F (37.4°C), blood pressure is 152/98 mmHg, pulse is 97/min, respirations are 15/min, and oxygen saturation is 99% on room air. Physical exam is notable for a cold and pale left leg. The patient’s sensation is markedly diminished in the left leg when compared to the right, and his muscle strength is 1/5 in his left leg. Which of the following is the best next step in management?
- A. Graded exercise and aspirin
- B. Surgical thrombectomy
- C. CT angiogram
- D. Heparin drip (Correct Answer)
- E. Tissue plasminogen activator
Acute limb ischemia management Explanation: ***Heparin drip***
- This patient presents with signs and symptoms of **acute limb ischemia** (sudden onset leg pain, cold and pale limb, diminished sensation, and motor weakness) in the setting of **atrial fibrillation**.
- Immediate initiation of an **anticoagulant**, such as a heparin drip, is crucial to prevent further clot propagation while definitive treatment is being arranged.
*Graded exercise and aspirin*
- This management strategy is typically reserved for **chronic peripheral artery disease** (PAD) with intermittent claudication, not acute limb ischemia.
- In acute limb ischemia, immediate reperfusion is critical to preserve limb viability, which cannot be achieved with exercise or aspirin alone.
*Surgical thrombectomy*
- While **surgical thrombectomy** may be the definitive treatment for acute limb ischemia, it is not the *immediate* next step in management.
- Anticoagulation should be initiated *before* surgical intervention to stabilize the patient and prevent further thrombosis.
*CT angiogram*
- A **CT angiogram** is a valuable diagnostic tool to pinpoint the location and extent of the occlusion.
- However, in a patient with clear signs of acute limb ischemia, **anticoagulation should not be delayed** for imaging alone. Heparin should be started immediately, and imaging can be performed concurrently if feasible or shortly thereafter.
*Tissue plasminogen activator*
- **Tissue plasminogen activator (tPA)** is a thrombolytic agent that can be used in some cases of acute limb ischemia, particularly for smaller, more distal thrombi or when surgical options are difficult.
- However, its use carries a higher risk of bleeding complications and is generally considered after initial anticoagulation and a thorough assessment, sometimes guided by angiography. It's not typically the *first* step in an emergency presentation like this.
Acute limb ischemia management US Medical PG Question 6: A 72-year-old man comes to the emergency department because of severe, acute, right leg pain for 2 hours. The patient's symptoms started suddenly while he was doing household chores. He has no history of leg pain at rest or with exertion. Yesterday, he returned home after a 6-hour bus ride from his grandson's home. He has hypertension treated with ramipril. He appears uncomfortable. His temperature is 37.4°C (99.3°F), pulse is 105/min and irregular, and blood pressure is 146/92 mm Hg. The right lower extremity is cool and tender to touch. A photograph of the limb is shown. Femoral pulses are palpable bilaterally; popliteal and pedal pulses are decreased on the right side. Sensation to pinprick and light touch and muscle strength are decreased in the right lower extremity. Which of the following is most likely to confirm the underlying source of this patient's condition?
- A. Biopsy of a superficial vein
- B. Doppler ultrasonography of the legs
- C. Digital subtraction angiography
- D. Manometry
- E. Echocardiography (Correct Answer)
Acute limb ischemia management Explanation: ***Echocardiography***
- The patient's presentation with acute, severe leg pain, coolness, decreased pulses, and neurological deficits in the right lower extremity, along with an **irregular pulse** (suggesting **atrial fibrillation**), points to an **arterial embolism**.
- An **echocardiogram** is crucial to identify the source of the embolus, most commonly a **left atrial thrombus** due to atrial fibrillation, which would then confirm the underlying cause.
*Biopsy of a superficial vein*
- A biopsy of a superficial vein would be indicated for conditions like **vasculitis** or **thrombophlebitis**, which are not consistent with the acute, severe arterial occlusion observed.
- This test would not help in identifying the source of an arterial embolus causing acute limb ischemia.
*Doppler ultrasonography of the legs*
- While **Doppler ultrasonography** can confirm the presence of **arterial occlusion** and assess flow, it does not identify the **source** of an embolus.
- It is more useful for diagnosing deep vein thrombosis or chronic arterial insufficiency, which are not the primary concern here.
*Digital subtraction angiography*
- **Digital subtraction angiography** is an invasive procedure that can precisely map the arterial tree and identify the location of the **occlusion**.
- However, it primarily pinpoints the site of the blockage and doesn't reveal the **etiology** or the source of an embolus in the heart.
*Manometry*
- **Manometry** is used to measure pressures, typically in the gastrointestinal tract or for compartment syndrome, and is not relevant for diagnosing the source of an arterial embolus.
- This diagnostic tool has no role in the investigation of acute limb ischemia or its cardiac origin.
Acute limb ischemia management US Medical PG Question 7: A 25-year-old patient is brought into the emergency department after he was found down by the police in 5 degree celsius weather. The police state the patient is a heroin-user and is homeless. The patient's vitals are T 95.3 HR 80 and regular BP 150/90 RR 10. After warming the patient, you notice his left lower leg is now much larger than his right leg. On exam, the patient has a loss of sensation on his left lower extremity. There is a faint palpable dorsalis pedal pulse, but no posterior tibial pulse. The patient is unresponsive to normal commands, but shrieks in pain upon passive stretch of his left lower leg. What is the most probable cause of this patient's condition?
- A. Diabetes
- B. Cellulitis
- C. Embolized clot
- D. Reperfusion associated edema (Correct Answer)
- E. Necrotizing fasciitis
Acute limb ischemia management Explanation: ***Reperfusion associated edema***
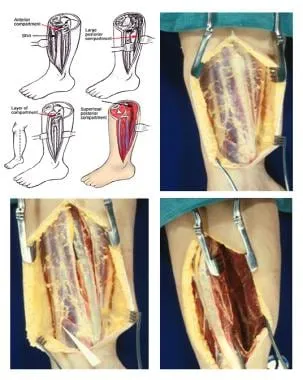
- The patient's history of being found in cold weather, along with signs of **hypothermia** (T 95.3), suggests a period of **ischemia** followed by reperfusion. The sudden swelling, pain on passive stretch, and sensory loss in the left lower leg are classic signs of **compartment syndrome**, which can be triggered by reperfusion injury and edema.
- While a faint dorsalis pedis pulse is present, the absence of a posterior tibial pulse indicates significant compromised blood flow, and the severe pain on passive stretch is a hallmark of increased pressure within a muscle compartment.
*Diabetes*
- While diabetes can cause neuropathy and vascular complications, it does not typically present with acute, severe localized swelling and pain on passive stretch in a previously healthy 25-year-old.
- The acute nature of the symptoms following exposure to cold and subsequent warming points away from chronic diabetic complications.
*Cellulitis*
- Cellulitis is a bacterial skin infection that would typically present with **erythema**, **warmth**, and spreading tenderness, but not the severe, deep, and acute pain on passive stretch or the profound sensory deficit seen here.
- It does not explain the initial period of cold exposure followed by reperfusion.
*Embolized clot*
- An embolized clot would cause acute limb ischemia, characterized by the "6 Ps" (**pain, pallor, pulselessness, paresthesias, paralysis, poikilothermia**). While the patient has some of these, the dramatic swelling *after warming* and the pain on passive stretch are more indicative of compartment syndrome due to reperfusion.
- The presence of a faint dorsalis pedal pulse makes complete arterial occlusion less likely, though significant compromise is present.
*Necrotizing fasciitis*
- Necrotizing fasciitis presents with rapidly progressing pain out of proportion to exam, skin changes (e.g., **bullae, crepitus, discoloration**), and systemic toxicity. While serious, it does not fit the context of acute swelling and pain primarily triggered by reperfusion after cold exposure.
- The primary presentation here is related to pressure-induced injury from edema, not primarily an aggressive bacterial infection of the fascia.
Acute limb ischemia management US Medical PG Question 8: Four days after undergoing a craniotomy and evacuation of a subdural hematoma, a 56-year-old man has severe pain and swelling of his right leg. He has chills and nausea. He has type 2 diabetes mellitus and chronic kidney disease, and was started on hemodialysis 2 years ago. Prior to admission, his medications were insulin, enalapril, atorvastatin, and sevelamer. His temperature is 38.3°C (101°F), pulse is 110/min, and blood pressure is 130/80 mm Hg. Examination shows a swollen, warm, and erythematous right calf. Dorsiflexion of the right foot causes severe pain in the right calf. The peripheral pulses are palpated bilaterally. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 11,800/mm3
Platelet count 230,000/mm3
Serum
Glucose 87 mg/dL
Creatinine 1.9 mg/dL
Which of the following is the most appropriate next step in treatment?
- A. Urokinase therapy
- B. Iliac stenting
- C. Warfarin therapy
- D. Unfractionated heparin therapy (Correct Answer)
- E. Inferior vena cava filter
Acute limb ischemia management Explanation: ***Unfractionated heparin therapy***
- The patient presents with classic symptoms of **deep vein thrombosis (DVT)**, including unilateral leg pain, swelling, warmth, erythema, and a positive Homan's sign (pain on dorsiflexion). The recent craniotomy places him at high risk for DVT.
- **Unfractionated heparin is the anticoagulant of choice** for this patient due to TWO critical factors:
1. **Recent craniotomy (4 days ago)**: Requires a rapidly reversible anticoagulant in case of intracranial bleeding; UFH can be reversed with protamine sulfate
2. **Chronic kidney disease on hemodialysis**: Low molecular weight heparin (LMWH) is contraindicated in severe renal failure (CrCl <30 mL/min) as it is renally eliminated and increases bleeding risk. UFH is not renally cleared and can be monitored with aPTT.
*Urokinase therapy*
- **Urokinase is a thrombolytic agent** used to dissolve existing clots, primarily in cases of massive pulmonary embolism or severe DVT with limb-threatening ischemia (phlegmasia cerulea dolens).
- Given the patient's **recent craniotomy and subdural hematoma evacuation**, thrombolytic therapy is **absolutely contraindicated** due to very high risk of intracranial hemorrhage. Recent neurosurgery is a contraindication for at least 2-4 weeks.
*Iliac stenting*
- **Iliac vein stenting** is a procedure typically used to treat chronic **iliac vein compression** (e.g., May-Thurner syndrome) or chronic post-thrombotic obstruction.
- This is an **acute DVT presentation** (4 days post-op) with no indication of chronic iliac vein compression or obstruction. Stenting has no role in acute DVT management.
*Warfarin therapy*
- **Warfarin is an oral anticoagulant** used for long-term DVT treatment but has a **delayed onset of action** (requires 5-7 days to reach therapeutic INR).
- It is **not suitable for acute initial treatment** of DVT, especially in a patient requiring rapid anticoagulation. Warfarin must be overlapped with parenteral anticoagulation (heparin) initially.
- Additionally, warfarin dosing is complex in dialysis patients due to altered vitamin K metabolism.
*Inferior vena cava filter*
- An **IVC filter** is indicated for patients with DVT who have an **absolute contraindication to anticoagulation** (e.g., active bleeding, recent hemorrhagic stroke) or who develop recurrent thromboembolism despite adequate anticoagulation.
- This patient **does not have a contraindication to anticoagulation**. While he had recent neurosurgery, unfractionated heparin is safe to use with careful monitoring and is rapidly reversible if needed.
- IVC filters have significant complications (thrombosis, filter migration, IVC perforation) and should be avoided when anticoagulation is feasible.
Acute limb ischemia management US Medical PG Question 9: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Acute limb ischemia management Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Acute limb ischemia management US Medical PG Question 10: A 65-year-old man comes to the emergency department because of sudden, worsening pain in his right calf and foot that started 30 minutes ago. He also has a tingling sensation and weakness in his right leg. He has had no similar episodes, recent trauma, or claudication. He has type 2 diabetes mellitus and was diagnosed with hypertension 20 years ago. His sister has systemic sclerosis. He works as an office administrator and sits at his desk most of the day. He has smoked one and a half packs of cigarettes daily for 30 years. Current medications include metformin and lisinopril. His pulse is 110/min, respirations are 16/min, and blood pressure is 140/90 mm Hg. His right leg is pale and cool to touch. Muscle strength in his right leg is mildly reduced. Pedal pulses are absent on the right. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Popliteal artery aneurysm
- B. Atherosclerotic narrowing of the artery
- C. Arterial vasospasm
- D. Atheroembolism
- E. Arterial embolism (Correct Answer)
Acute limb ischemia management Explanation: ***Arterial embolism***
- The sudden onset of severe unilateral limb pain, pallor, coolness, and absent pulses in a patient with risk factors for **atherosclerosis** and possible **arrhythmias** (given the history of hypertension and diabetes) strongly suggests acute limb ischemia due to an arterial embolism.
- The patient's presentation aligns with the "6 P's" of acute limb ischemia: **pain, pallor, pulselessness, paresthesias, poikilothermia (coolness), and paralysis** (weakness).
*Popliteal artery aneurysm*
- While a popliteal artery aneurysm can cause acute limb ischemia due to thrombosis or embolism within the aneurysm, it is more commonly associated with chronic limb ischemia or rupture, and a **palpable pulsatile mass** is typically present, which is not mentioned.
- The suddenness and severity of symptoms are more indicative of an embolic event rather than a thrombotic event within an aneurysm, which often presents less acutely.
*Atherosclerotic narrowing of the artery*
- **Atherosclerotic narrowing** typically causes chronic limb ischemia with symptoms like **claudication**, which is pain that worsens with exercise and improves with rest. The patient explicitly denies claudication.
- Acute worsening of atherosclerotic narrowing, often due to **plaque rupture and thrombosis**, would usually affect a limb with pre-existing claudication, and the onset might be less abrupt than described.
*Arterial vasospasm*
- **Arterial vasospasm** (e.g., Raynaud's phenomenon) primarily affects the small arteries and arterioles, typically in the digits, and is often triggered by cold or stress.
- It would not typically cause acute, severe, and widespread limb ischemia with absent pedal pulses in a large artery, and the patient's symptoms are not consistent with known vasospastic disorders affecting large vessels.
*Atheroembolism*
- **Atheroembolism** (e.g., "blue toe syndrome") typically involves multiple, small cholesterol emboli showering downstream, causing patchy ischemia, livedo reticularis, and renal or gastrointestinal involvement.
- While the patient has significant atherosclerotic risk factors, the sudden, complete obliteration of flow to the entire right leg, indicated by absent pedal pulses and diffuse symptoms, points more towards a **single, larger embolic occlusion** rather than diffuse microemboli.
More Acute limb ischemia management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.