Abdominal aortic aneurysm repair US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Abdominal aortic aneurysm repair. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Abdominal aortic aneurysm repair US Medical PG Question 1: A 70-year-old man presents for his annual check-up. He says he feels well except for occasional abdominal pain. He describes the pain as 4/10–5/10 in intensity, diffusely localized to the periumbilical and epigastric regions, radiating to the groin. The pain occurs 1–2 times a month and always subsides on its own. The patient denies any recent history of fever, chills, nausea, vomiting, change in body weight, or change in bowel and/or bladder habits. His past medical history is significant for hypertension, hyperlipidemia, and peripheral vascular disease, managed with lisinopril and simvastatin. The patient reports a 40-pack-year smoking history and 1–2 alcoholic drinks a day. The blood pressure is 150/100 mm Hg and the pulse is 80/min. Peripheral pulses are 2+ bilaterally in all extremities. Abdominal exam reveals a bruit in the epigastric region along with mild tenderness to palpation with no rebound or guarding. There is also a pulsatile abdominal mass felt on deep palpation at the junction of the periumbilical and the suprapubic regions. The remainder of the physical exam is normal. Laboratory studies show:
Serum total cholesterol 175 mg/dL
Serum total bilirubin 1 mg/dL
Serum amylase 25 U/L
Serum alanine aminotransferase (ALT) 20 U/L
Serum aspartate aminotransferase (AST) 16 U/L
Which of the following is the most likely diagnosis in this patient?
- A. Mesenteric ischemia
- B. Acute pancreatitis
- C. Abdominal aortic aneurysm (Correct Answer)
- D. Acute gastritis
- E. Diverticulitis
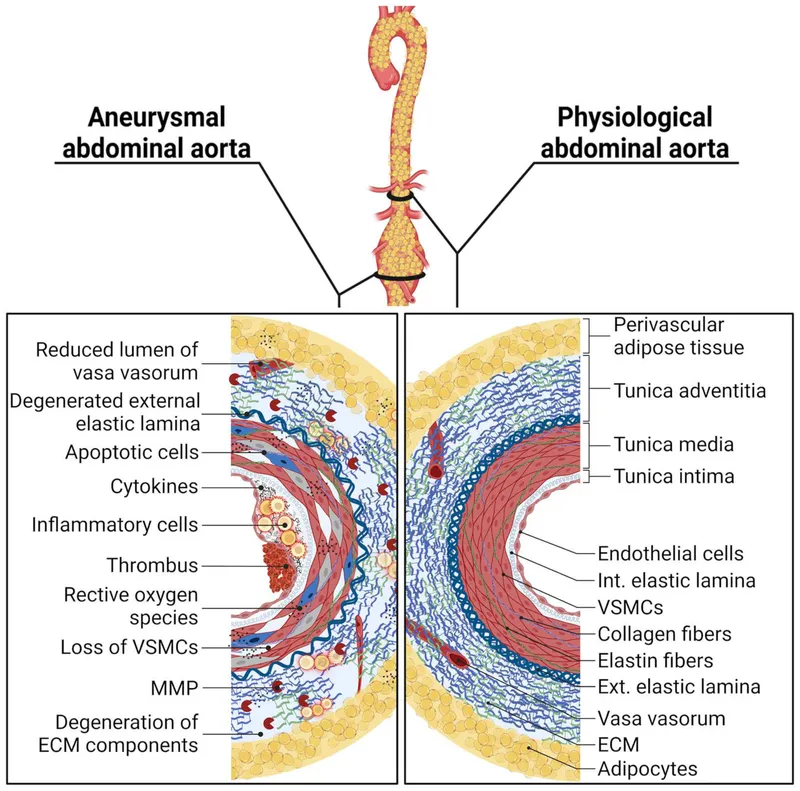
Abdominal aortic aneurysm repair Explanation: ***Abdominal aortic aneurysm***
- The presence of a **pulsatile abdominal mass**, epigastric bruit, and a history of **hypertension, hyperlipidemia, peripheral vascular disease, and smoking** are highly suggestive of an abdominal aortic aneurysm (AAA).
- The diffuse, radiating abdominal pain, while non-specific, can be associated with an expanding aneurysm, and the patient's age and risk factors significantly increase the likelihood of AAA.
*Mesenteric ischemia*
- Mesenteric ischemia typically presents with **severe abdominal pain out of proportion to physical exam findings**, often postprandial, and can be associated with weight loss due to fear of eating.
- While the patient has vascular risk factors, the pain is described as moderate, infrequent, and subsiding on its own, and there is no mention of weight loss, making it less likely.
*Acute pancreatitis*
- Acute pancreatitis is characterized by **severe epigastric pain that radiates to the back**, often accompanied by nausea, vomiting, and elevated serum **amylase and lipase** levels.
- This patient's pain is diffuse and radiates to the groin, not the back, and his serum amylase is normal, ruling out acute pancreatitis.
*Acute gastritis*
- Acute gastritis typically causes **epigastric pain, nausea, and vomiting**, often triggered by NSAIDs, alcohol, or H. pylori infection.
- The patient's pain is diffuse, radiates to the groin, and occurs infrequently, with no mention of triggers or other gastrointestinal symptoms typical of gastritis.
*Diverticulitis*
- Diverticulitis usually presents with **left lower quadrant pain**, fever, leukocytosis, and changes in bowel habits.
- This patient's pain is periumbilical/epigastric, has no associated fever or changes in bowel habits, and is not consistent with the typical presentation of diverticulitis.
Abdominal aortic aneurysm repair US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Abdominal aortic aneurysm repair Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Abdominal aortic aneurysm repair US Medical PG Question 3: A 68-year-old man presents for a screening ultrasound scan. He has been feeling well and is in his usual state of good health. His medical history is notable for mild hypertension and a 100-pack-year tobacco history. He has a blood pressure of 128/86 and heart rate of 62/min. Physical examination is clear lung sounds and regular heart sounds. On ultrasound, an infrarenal aortic aneurysm of 4 cm in diameter is identified. Which of the following is the best initial step for this patient?
- A. Reassurance
- B. Beta-blockers
- C. Urgent repair
- D. Surveillance (Correct Answer)
- E. Elective repair
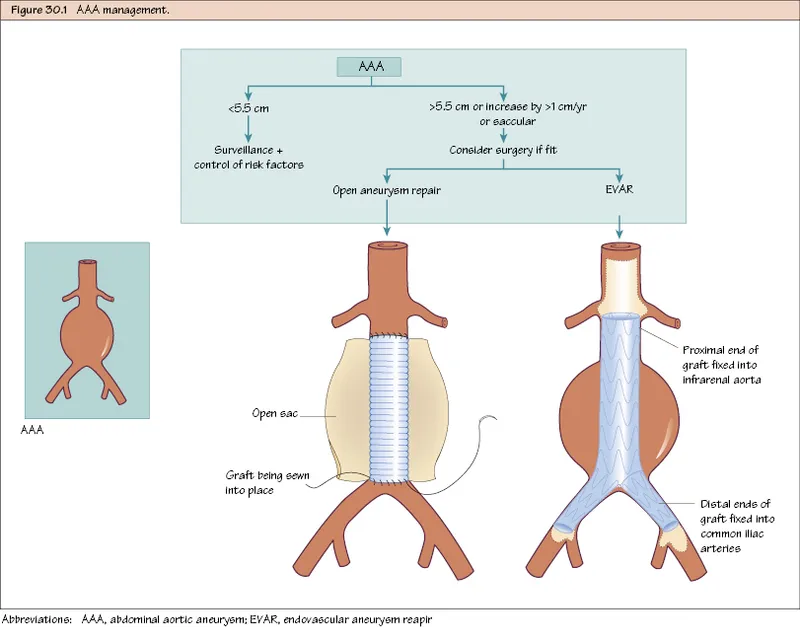
Abdominal aortic aneurysm repair Explanation: **Surveillance**
- An **infrarenal aortic aneurysm** of 4 cm in diameter in an asymptomatic patient is typically managed with **regular surveillance** to monitor for growth.
- Surgical intervention is generally reserved for aneurysms larger than 5.5 cm or those that are rapidly expanding or symptomatic.
*Reassurance*
- While it's important to provide reassurance, simply doing so without a concrete plan for follow-up would be inappropriate given the potential for **aneurysm expansion** and rupture.
- The patient's **tobacco history** is a significant risk factor for aneurysm progression and warrants monitoring.
*Beta-blockers*
- Beta-blockers may be part of the medical management for **hypertension** and could theoretically slow aneurysm growth by reducing pulsatile stress.
- However, they are not the primary **initial step** for an asymptomatic aneurysm of this size and do not replace the need for surveillance.
*Urgent repair*
- **Urgent repair** is indicated for symptomatic aneurysms, those that are rapidly expanding, or those showing signs of rupture or impending rupture, none of which are present here.
- A 4 cm aneurysm in an asymptomatic patient does not meet the criteria for **urgent intervention**.
*Elective repair*
- **Elective repair** is typically considered for aneurysms exceeding 5.5 cm in diameter or those that are symptomatic or rapidly growing.
- A 4 cm aneurysm is below the threshold for **elective repair** in an asymptomatic patient without other high-risk features.
Abdominal aortic aneurysm repair US Medical PG Question 4: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Abdominal aortic aneurysm repair Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
Abdominal aortic aneurysm repair US Medical PG Question 5: A 71-year-old man with hypertension is taken to the emergency department after the sudden onset of stabbing abdominal pain that radiates to the back. He has smoked 1 pack of cigarettes daily for 20 years. His pulse is 120/min and thready, respirations are 18/min, and blood pressure is 82/54 mm Hg. Physical examination shows a periumbilical, pulsatile mass and abdominal bruit. There is epigastric tenderness. Which of the following is the most likely underlying mechanism of this patient's current condition?
- A. Mesenteric atherosclerosis
- B. Gastric mucosal ulceration
- C. Portal vein stasis
- D. Abdominal wall defect
- E. Aortic wall stress (Correct Answer)
Abdominal aortic aneurysm repair Explanation: ***Aortic wall stress***
- The patient's presentation with **sudden onset of stabbing abdominal pain radiating to the back**, **hypotension** (BP 82/54 mm Hg), **tachycardia** (pulse 120/min), and a **pulsatile periumbilical mass** with an **abdominal bruit** is highly suggestive of a ruptured **abdominal aortic aneurysm (AAA)**.
- **Aortic wall stress**, often exacerbated by **hypertension** and **smoking**, leads to the progressive weakening and dilation of the aortic wall, eventually resulting in rupture.
*Mesenteric atherosclerosis*
- This condition typically causes **chronic abdominal pain** that is worse after eating (**postprandial angina**) due to inadequate blood supply to the intestines.
- It does not usually present with an acute, catastrophic event like **shock** and a **pulsatile mass**.
*Gastric mucosal ulceration*
- Ulceration can cause **epigastric pain**, but a ruptured ulcer would typically present with signs of **peritonitis** (rigidity, rebound tenderness) and potentially **hematemesis** or **melena**, which are not described.
- It would not cause a **pulsatile periumbilical mass** or the characteristic back pain of an AAA.
*Portal vein stasis*
- **Portal vein stasis** or **thrombosis** often leads to **portal hypertension**, **ascites**, and **gastrointestinal bleeding** from varices.
- It does not explain the acute onset of severe abdominal pain, hypotension, a pulsatile mass, or an abdominal bruit.
*Abdominal wall defect*
- An **abdominal wall defect**, such as a hernia, can cause localized pain and sometimes bowel obstruction.
- However, it does not account for the **hypotension**, **tachycardia**, **radiating pain to the back**, or the **pulsatile mass**, all of which point to a major vascular emergency.
Abdominal aortic aneurysm repair US Medical PG Question 6: An 88-year-old woman with no significant medical history is brought to the emergency room by her daughter after a fall, where the woman lightly hit her head against a wall. The patient is lucid and complains of a mild headache. The daughter indicates that her mother did not lose consciousness after the fall. On exam, there are no focal neurological deficits, but you decide to perform a CT scan to be sure there is no intracranial bleeding. The CT scan is within normal limits and head MRI is performed (shown). Which of the following conditions has the most similar risk factor to this patient's condition?
- A. Pulmonary embolism
- B. Raynaud's phenomenon
- C. Prinzmetal's angina
- D. Abdominal aortic aneurysm
- E. Thoracic aortic aneurysm (Correct Answer)
Abdominal aortic aneurysm repair Explanation: ***Thoracic aortic aneurysm***
- The MRI images show numerous **microhemorrhages** (dark spots on the GRE/SWI sequences), indicative of **cerebral amyloid angiopathy (CAA)**, a common cause of lobar intracerebral hemorrhage in the elderly.
- CAA is most strongly associated with **advanced age** (the primary risk factor), and both CAA and **thoracic aortic aneurysm (TAA)** can be associated with **underlying connective tissue abnormalities** and vascular wall weakening processes.
- While the exact pathophysiology differs, both conditions involve progressive vascular wall degeneration that increases with age.
*Abdominal aortic aneurysm*
- While AAA is strongly associated with **advanced age**, **hypertension**, and **smoking**, it is primarily driven by **atherosclerotic degeneration** rather than the amyloid deposition seen in CAA.
- AAA has a particularly strong association with smoking (the most important modifiable risk factor), which is not characteristic of CAA.
*Pulmonary embolism*
- Primarily caused by **venous thromboembolism** (VTE) due to factors like immobility, surgery, cancer, and hypercoagulable states, which are distinct from CAA risk factors.
- While age is a risk factor for PE, the underlying mechanisms (thrombosis vs. vascular wall amyloid deposition) differ fundamentally.
*Raynaud's phenomenon*
- Characterized by **vasospasm** of small arteries and arterioles, typically triggered by cold or stress, and is often associated with connective tissue diseases.
- Its pathophysiology is unrelated to the progressive vascular wall degeneration and amyloid deposition seen in CAA.
*Prinzmetal's angina*
- Caused by **coronary artery spasm**, leading to transient myocardial ischemia, often occurring at rest and typically not associated with age-related vascular degeneration.
- The mechanism is localized vascular spasm rather than widespread degenerative arterial disease or amyloid deposition.
Abdominal aortic aneurysm repair US Medical PG Question 7: A 67-year-old man presents to the emergency department with abdominal pain that started 1 hour ago. The patient has a past medical history of diabetes and hypertension as well as a 40 pack-year smoking history. His blood pressure is 107/58 mmHg, pulse is 130/min, respirations are 23/min, and oxygen saturation is 98% on room air. An abdominal ultrasound demonstrates focal dilation of the aorta with peri-aortic fluid. Which of the following is the best next step in management?
- A. Serial annual abdominal ultrasounds
- B. Emergent surgical intervention (Correct Answer)
- C. Administer labetalol
- D. Counsel the patient in smoking cessation
- E. Urgent surgery within the next day
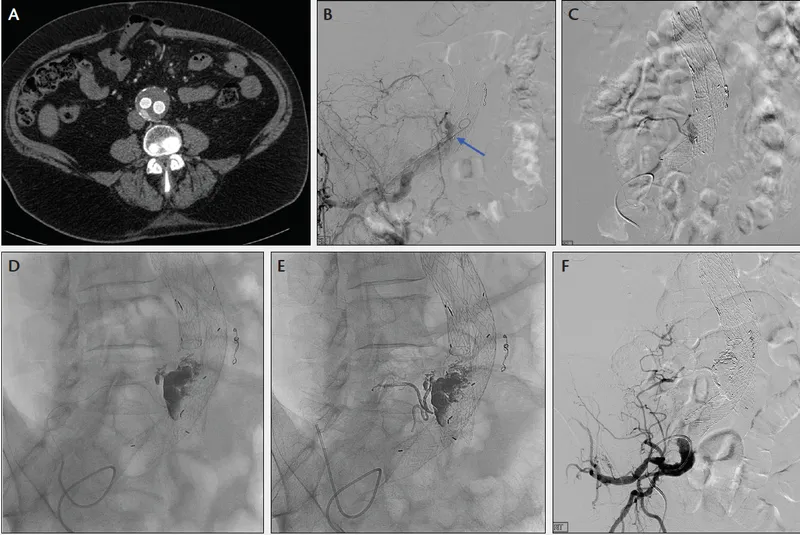
Abdominal aortic aneurysm repair Explanation: ***Emergent surgical intervention***
- The patient's presentation with acute **abdominal pain**, **hypotension**, and **tachycardia** combined with ultrasound findings of focal aortic dilation and peri-aortic fluid strongly suggests a **ruptured abdominal aortic aneurysm (AAA)**.
- A ruptured AAA is a life-threatening emergency requiring immediate surgical repair to prevent further hemorrhage and death.
*Serial annual abdominal ultrasounds*
- This approach is appropriate for asymptomatic patients with smaller, stable AAAs (typically <5.5 cm) to monitor for growth.
- In this case, the patient is symptomatic with signs of rupture, making surveillance an inappropriate and dangerous management strategy.
*Administer labetalol*
- Medications like labetalol are used to control blood pressure in conditions like aortic dissection or to slow the progression of AAAs, but they are contraindicated in hypotensive patients with a ruptured AAA.
- In this patient, labetalol would worsen the existing hypotension and could lead to cardiovascular collapse.
*Counsel the patient in smoking cessation*
- Smoking cessation is a crucial long-term intervention to reduce the risk of AAA expansion and rupture.
- While important, it does not address the immediate, life-threatening emergency of a ruptured AAA.
*Urgent surgery within the next day*
- Waiting until the next day for surgery in a patient with a suspected ruptured AAA is unacceptable.
- The patient's hemodynamic instability (hypotension, tachycardia) indicates active bleeding, and any delay significantly increases morbidity and mortality.
Abdominal aortic aneurysm repair US Medical PG Question 8: A previously healthy 64-year-old man comes to the physician 3 days after noticing a lump in his right groin while he was bathing. He has no history of trauma to the region. He has hypercholesterolemia and hypertension treated with atorvastatin and labetalol. He has smoked 2 packs of cigarettes daily for 35 years. His vital signs are within normal limits. Examination shows a 4-cm (1.6-in), nontender, pulsatile mass with a palpable thrill at the right midinguinal point. On auscultation, a harsh continuous murmur is heard over the mass. Femoral and pedal pulses are palpable bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Femoral lymphadenopathy
- B. Femoral abscess
- C. Femoral hernia
- D. Arteriovenous fistula of the femoral vessels
- E. Femoral artery aneurysm (Correct Answer)
Abdominal aortic aneurysm repair Explanation: ***Femoral artery aneurysm***
- A **pulsatile mass** with a **palpable thrill** and a **harsh continuous murmur** heard over the mass in the groin is highly indicative of an aneurysm with turbulent flow.
- The patient's history of **smoking** and **hypercholesterolemia** are significant risk factors for **atherosclerosis**, which is the most common cause of peripheral aneurysms.
*Femoral lymphadenopathy*
- Lymphadenopathy typically presents as a **nontender, firm, rubbery mass** that is usually **non-pulsatile**.
- It would not typically be associated with a **thrill** or a **harsh continuous murmur**, which are signs of vascular flow.
*Femoral abscess*
- An abscess would present with signs of **inflammation**, such as redness, warmth, tenderness, and possibly fever, none of which are mentioned here.
- An abscess is typically a **non-pulsatile, fluctuant mass** and would not exhibit a thrill or a continuous murmur.
*Femoral hernia*
- A hernia is a protrusion of abdominal contents through a weakened area, often reducible and typically **non-pulsatile**.
- A hernia would not characteristically present with a **thrill** or a **harsh continuous murmur**, which are vascular findings.
*Arteriovenous fistula of the femoral vessels*
- While an AV fistula can cause a **pulsatile mass**, **thrill**, and **continuous murmur**, it typically arises from trauma or iatrogenic injury, which is not present in this case.
- An AV fistula would also likely involve more immediate symptoms and potentially distal ischemia or signs of venous congestion, which are not described.
Abdominal aortic aneurysm repair US Medical PG Question 9: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Abdominal aortic aneurysm repair Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Abdominal aortic aneurysm repair US Medical PG Question 10: A 56-year-old man presents to the emergency department with severe chest pain and a burning sensation. He accidentally drank a cup of fluid at his construction site 2 hours ago. The liquid was later found to contain lye. On physical examination, his blood pressure is 100/57 mm Hg, respiratory rate is 21/min, pulse is 84/min, and temperature is 37.7°C (99.9°F). The patient is sent immediately to the radiology department. The CT scan shows air in the mediastinum, and a contrast swallow study confirms the likely diagnosis. Which of the following is the best next step in the management of this patient’s condition?
- A. Ceftriaxone
- B. Oral antidote
- C. Dexamethasone
- D. Surgical repair (Correct Answer)
- E. Nasogastric lavage
Abdominal aortic aneurysm repair Explanation: ***Surgical repair***
- The presence of **mediastinal air** on CT scan and confirmation of **esophageal perforation** by contrast swallow study indicate a surgical emergency.
- **Emergency surgical repair** is crucial to prevent widespread mediastinitis, sepsis, and potential mortality from corrosive ingestion.
*Ceftriaxone*
- While **antibiotics** like Ceftriaxone might be used as adjuncts to prevent infection, they are not the primary treatment for an established esophageal perforation.
- Antibiotics alone will not address the structural defect or contain the leakage of corrosive material into the mediastinum.
*Oral antidote*
- For corrosive ingestions, administering an **oral antidote** is contraindicated as it can worsen tissue damage or induce vomiting, leading to further esophageal injury.
- The immediate priority is managing the perforation, not neutralizing the corrosive agent internally.
*Dexamethasone*
- **Corticosteroids** like dexamethasone are sometimes considered in the management of corrosive ingestions to reduce stricture formation, but their role is controversial and they are not the initial treatment for an acute perforation.
- In an active perforation, corticosteroids would not address the immediate life-threatening issue of mediastinal contamination.
*Nasogastric lavage*
- **Nasogastric lavage** is contraindicated in corrosive ingestions, especially with suspected or confirmed perforation.
- Passing a tube could further injure the already damaged tissue and increase the risk of perforation or exacerbate an existing one.
More Abdominal aortic aneurysm repair US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.