Vascular Surgery

On this page
🩸 The Vascular Surgeon's Arsenal: Mastering Life-Saving Interventions
Blood moves silently through 60,000 miles of vessels until it doesn't-then minutes decide between limb and loss, patency and stroke, rupture and rescue. You'll master the pathophysiology driving vascular catastrophes, recognize the clinical patterns that distinguish claudication from compartment syndrome, and command the diagnostic algorithms and interventions that define modern vascular surgery. This lesson transforms you from observer to decision-maker, integrating hemodynamics, physical diagnosis, imaging interpretation, and evidence-based surgical strategy into rapid, life-saving action.
📌 Remember: SAVES - Stenosis assessment, Aneurysm evaluation, Venous insufficiency, Embolectomy techniques, Surgical bypass principles
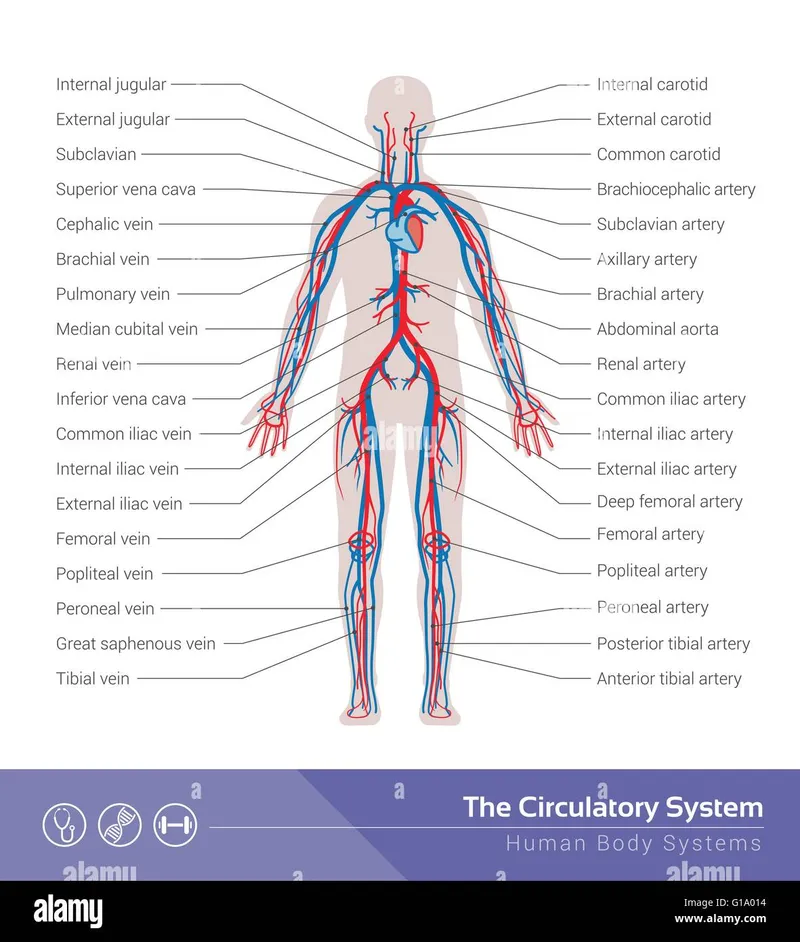
The vascular system processes 5 liters of blood every minute through 60,000 miles of vessels, maintaining perfusion pressures between 60-100 mmHg systemically. Understanding normal hemodynamics enables recognition of pathological states requiring surgical intervention.
-
Arterial System Architecture
- High-pressure conduits (120/80 mmHg average)
- Muscular wall thickness: 10-15% of vessel diameter
- Intimal layer: <0.1mm thickness in healthy vessels
- Medial layer: 70% of wall composition
- Adventitial layer: 20% structural support
- Flow velocity: 30-40 cm/sec in major vessels
-
Venous Return Mechanisms
- Low-pressure system (5-10 mmHg central venous pressure)
- Valve competency: >95% closure efficiency required
- Valve spacing: 2-5 cm intervals in lower extremities
- Calf muscle pump: 60% of venous return contribution
- Respiratory pump: 25% venous return assistance
| Parameter | Arterial | Venous | Capillary | Clinical Threshold |
|---|---|---|---|---|
| Pressure (mmHg) | 80-120 | 5-15 | 15-25 | <60 = ischemia |
| Wall Thickness | 15% diameter | 5% diameter | 0.5μm | >20% = stenosis |
| Flow Velocity | 30-40 cm/s | 10-15 cm/s | 0.3 mm/s | <10 cm/s = critical |
| Oxygen Content | 98% saturation | 75% saturation | Variable | <70% = hypoxia |
| Compliance | Low | High | Minimal | Reduced = disease |
💡 Master This: Vascular surgery success depends on understanding perfusion pressure gradients. Mean arterial pressure >65 mmHg ensures organ perfusion, while >80 mmHg optimizes healing in surgical patients.
Understanding these hemodynamic principles provides the foundation for recognizing when surgical intervention becomes necessary, setting the stage for mastering specific pathophysiological mechanisms that drive vascular disease progression.
🩸 The Vascular Surgeon's Arsenal: Mastering Life-Saving Interventions
⚙️ The Hemodynamic Engine: Understanding Vascular Pathophysiology
📌 Remember: STENOSIS - Symptoms at 70% narrowing, Turbulent flow begins, Endothelial dysfunction, Neointimal hyperplasia, Occlusion risk >90%, Surgical threshold >50% (carotid), Ischemia develops, Salvage window 6 hours
-
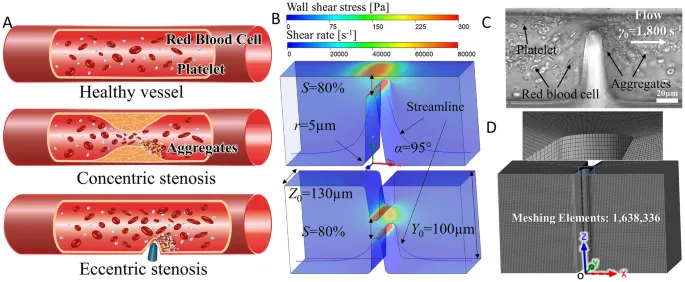
Atherosclerotic Progression Mechanisms
- Endothelial dysfunction: >40% nitric oxide reduction
- Lipid accumulation: LDL >160 mg/dL accelerates plaque formation
- Foam cell development: 72 hours post-injury
- Smooth muscle migration: 7-14 days timeline
- Fibrous cap formation: 6-12 months maturation
- Plaque vulnerability: <65μm cap thickness = rupture risk
-
Hemodynamic Consequences
- Critical stenosis: >70% diameter reduction
- Flow reserve depletion: 3:1 ratio normal to maximum
- Resting flow maintained until 85% stenosis
- Collateral development: 2-6 weeks establishment
- Pressure gradient: >20 mmHg across lesion
| Stenosis Severity | Diameter Reduction | Flow Reduction | Pressure Drop | Clinical Significance |
|---|---|---|---|---|
| Mild | <50% | <25% | <10 mmHg | Asymptomatic |
| Moderate | 50-69% | 25-75% | 10-40 mmHg | Exercise symptoms |
| Severe | 70-89% | 75-95% | 40-80 mmHg | Rest symptoms |
| Critical | 90-99% | 95-99% | >80 mmHg | Tissue loss risk |
| Occlusion | 100% | 100% | Variable | Acute ischemia |
⭐ Clinical Pearl: Reynolds number >2000 predicts turbulent flow and accelerated atherosclerosis. This occurs at >50% stenosis in most vessels, explaining why moderate lesions progress rapidly.
💡 Master This: Aneurysm formation follows Laplace's Law: $Tension = \frac{Pressure \times Radius}{Wall Thickness}$. Diameter >5.5 cm in abdominal aortic aneurysms creates exponential rupture risk, jumping from 1%/year at 4 cm to 25%/year at 6 cm.
These pathophysiological mechanisms create the clinical presentations that guide surgical decision-making, leading us to examine how pattern recognition enables rapid diagnosis and appropriate intervention timing.
⚙️ The Hemodynamic Engine: Understanding Vascular Pathophysiology
🎯 The Clinical Detective: Pattern Recognition in Vascular Disease
📌 Remember: The 6 Ps of acute limb ischemia - Pain, Pallor, Pulselessness, Paresthesias, Paralysis, Poikilothermia (cold). Paralysis and paresthesias indicate irreversible ischemia within 6 hours.
-
Acute Presentation Recognition Patterns
- Acute limb ischemia: 5 Ts timing framework
- Thrombosis: gradual onset over hours to days
- Trauma: immediate onset with obvious mechanism
- Thromboembolism: sudden onset, atrial fibrillation history
- Embolic source: 85% cardiac origin
- AF patients: 5x increased embolic risk
- Saddle embolus: bilateral symptoms, aortic bifurcation
- Tumor compression: progressive symptoms over weeks
- Thoracic outlet: positional symptoms, overhead activities
- Acute limb ischemia: 5 Ts timing framework
-
Chronic Presentation Patterns
- Claudication distance: <200 meters = severe disease
- Fontaine classification: Stage progression predictors
- Stage I: Asymptomatic - ABI 0.9-1.3
- Stage IIa: Claudication >200m - ABI 0.7-0.9
- Stage IIb: Claudication <200m - ABI 0.4-0.7
- Stage III: Rest pain - ABI <0.4
- Stage IV: Tissue loss - ABI <0.3
| Clinical Finding | Sensitivity | Specificity | Positive Predictive Value | Clinical Action |
|---|---|---|---|---|
| Absent pulse | 95% | 85% | 90% | Immediate imaging |
| ABI <0.9 | 90% | 95% | 85% | PAD workup |
| Bruit presence | 75% | 80% | 70% | Stenosis evaluation |
| Rest pain | 85% | 90% | 80% | Urgent referral |
| Tissue loss | 100% | 100% | 100% | Emergent surgery |
⭐ Clinical Pearl: Ankle pressure <50 mmHg or toe pressure <30 mmHg indicates critical limb ischemia requiring revascularization within 24-48 hours to prevent amputation.
💡 Master This: Rutherford classification provides standardized ischemia grading: Category 0 = viable limb, Category I = marginally threatened (salvageable if treated within 6 hours), Category II = immediately threatened (salvageable with immediate treatment), Category III = irreversible ischemia.
Pattern recognition enables rapid triage, but systematic comparison of similar presentations prevents diagnostic errors and guides appropriate intervention selection.
🎯 The Clinical Detective: Pattern Recognition in Vascular Disease
⚖️ The Differential Matrix: Systematic Vascular Diagnosis
📌 Remember: ARTERIAL vs VENOUS - Acute onset vs gradual, Rest pain vs activity pain, Temperature cold vs warm, Edema absent vs present, Red vs blue, Immobile vs mobile, Absent pulses vs present pulses, Lifeless vs livid
-
Acute Limb Ischemia Differential Framework
- Embolic occlusion: Sudden onset, normal contralateral pulses
- Cardiac source: 85% of cases
- AF prevalence: 60% of embolic events
- Saddle embolus: 15% bilateral presentation
- Aortic bifurcation involvement
- Immediate bilateral symptoms
- Mortality rate: 25-40% without surgery
- Thrombotic occlusion: Gradual onset, bilateral disease
- Atherosclerotic progression: weeks to months
- Collateral development: partial compensation
- Claudication history: 80% of patients
- Embolic occlusion: Sudden onset, normal contralateral pulses
-
Aneurysm vs Pseudoaneurysm Discrimination
- True aneurysm: All wall layers involved
- Growth rate: 2-4 mm/year average
- Rupture risk: 1%/year at 4-5 cm
- Wall composition: intact but weakened
- Pseudoaneurysm: Adventitia only containment
- Trauma history: 90% of cases
- Rapid expansion: days to weeks
- Rupture risk: immediate threat
- True aneurysm: All wall layers involved
| Condition | Onset | Pain Pattern | Pulse Exam | Temperature | Edema | Treatment Window |
|---|---|---|---|---|---|---|
| Arterial embolism | Sudden | Severe rest pain | Absent distal | Cold | None | 6 hours |
| Arterial thrombosis | Gradual | Progressive claudication | Diminished | Cool | Minimal | 6-12 hours |
| Venous thrombosis | Gradual | Aching, worse standing | Present | Warm | Significant | 24-48 hours |
| Compartment syndrome | Progressive | Severe with passive stretch | Present initially | Normal | Tense | 6 hours |
| Acute dissection | Sudden | Tearing, migrating | Variable | Variable | None | Immediate |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | ||||||
| flowchart TD |
Start["🩺 Acute Limb Pain
• Emergency arrival• Severe symptoms"]
Pulse["📋 Pulse Exam
• Bedside palpation• Doppler signal"]
Onset["📋 Onset Timing
• History of pain• Symptom duration"]
Edema["📋 Edema Pattern
• Check swelling• Pitting vs none"]
Embolic["🩺 Embolic Source
• Sudden occlusion• Likely AFib/cardiac"]
Thrombotic["🩺 Thrombotic Dis.
• Gradual narrowing• Plaque rupture"]
Venous["🩺 Venous Thrombo.
• DVT concern• Outflow blockage"]
Compartment["⚠️ Compartment Syn.
• ⬆️ Tissue pressure• Surgical emergency"]
Echo["🔬 Echocardiogram
• TTE or TEE test• View heart wall"]
Angio["🔬 Angiography
• Vessel imaging• Map arterial flow"]
Duplex["🔬 Duplex Ultrasound
• Vein compression• Check flow speed"]
Pressure["🔬 Pressure Measure
• Compartment probe• Check delta-P"]
Start --> Pulse Pulse -->|Absent| Onset Pulse -->|Present| Edema
Onset -->|Sudden| Embolic Onset -->|Gradual| Thrombotic
Edema -->|Significant| Venous Edema -->|Minimal| Compartment
Embolic --> Echo Thrombotic --> Angio Venous --> Duplex Compartment --> Pressure
style Start fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Pulse fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Onset fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Edema fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Embolic fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Thrombotic fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Venous fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Compartment fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style Echo fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Angio fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Duplex fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Pressure fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C
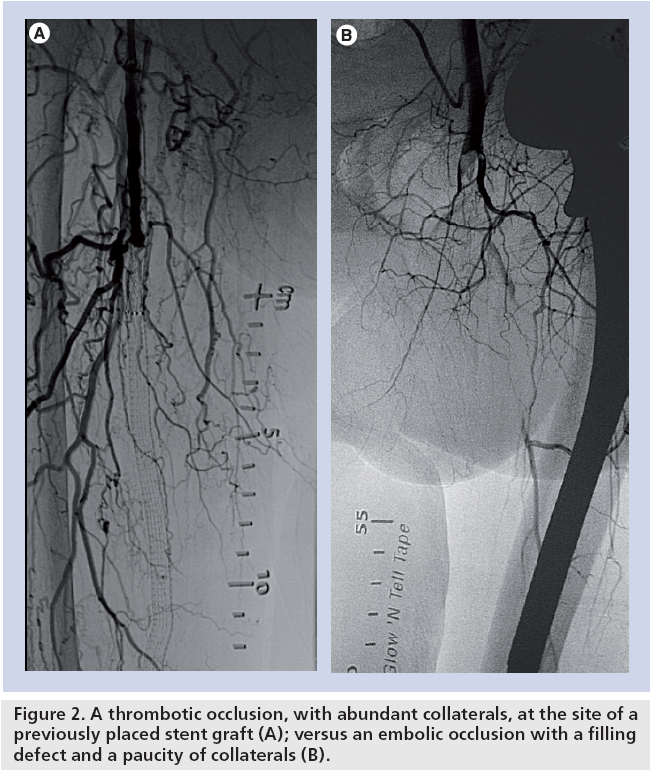
> ⭐ **Clinical Pearl**: **Embolic occlusion** shows **sharp cutoff** on angiography with **normal proximal vessel**, while **thrombotic occlusion** demonstrates **tapered narrowing** with **diffuse atherosclerotic changes** and **collateral circulation**.
> 💡 **Master This**: **Compartment pressure >30 mmHg** or **delta pressure <30 mmHg** (diastolic BP minus compartment pressure) indicates **compartment syndrome** requiring **immediate fasciotomy** regardless of pulse examination findings.
Systematic discrimination guides treatment selection, leading to evidence-based management algorithms that optimize outcomes while minimizing complications.
⚖️ The Differential Matrix: Systematic Vascular Diagnosis
🔧 The Surgical Algorithm: Evidence-Based Vascular Interventions
📌 Remember: ENDOVASCULAR vs OPEN - Early recovery, No general anesthesia, Day surgery possible, Outpatient feasible, Versatile approach, Anatomic limitations, Stenosis recurrence, Contrast nephrotoxicity, Ultrasound guidance, Less invasive, Angioplasty option, Rapid deployment
-
Endovascular Intervention Algorithms
- TASC Classification guides treatment approach
- TASC A lesions: Endovascular first-line (>95% success)
- TASC B lesions: Endovascular preferred (85-90% success)
- TASC C lesions: Open surgery preferred (70-80% success endovascular)
- TASC D lesions: Open surgery recommended (<60% success endovascular)
- Lesion characteristics determining approach
- Length <10 cm: Angioplasty/stenting preferred
- Length >20 cm: Bypass surgery preferred
- Calcification >50%: Atherectomy consideration
- Chronic total occlusion: Subintimal angioplasty or bypass
- TASC Classification guides treatment approach
-
Open Surgical Algorithms
- Bypass graft selection hierarchy
- Autogenous vein: First choice (85% 5-year patency)
- Prosthetic graft: Above-knee (70% 5-year patency)
- Composite graft: Below-knee (60% 5-year patency)
- Endarterectomy indications
- Carotid stenosis >70% symptomatic
- Carotid stenosis >80% asymptomatic
- Perioperative stroke risk <3%
- Life expectancy >5 years
- Bypass graft selection hierarchy
| Intervention | 30-day Patency | 1-year Patency | 5-year Patency | Complication Rate | Cost Ratio |
|---|---|---|---|---|---|
| Angioplasty alone | 95% | 75% | 50% | 5% | 1.0x |
| Angioplasty + Stent | 98% | 85% | 65% | 8% | 1.5x |
| Vein bypass | 98% | 90% | 85% | 15% | 3.0x |
| Prosthetic bypass | 95% | 85% | 70% | 20% | 2.5x |
| Endarterectomy | 99% | 95% | 90% | 10% | 2.0x |
⭐ Clinical Pearl: Drug-eluting stents reduce restenosis rates from 30-40% to 10-15% at 1 year, but require dual antiplatelet therapy for 12 months minimum, increasing bleeding risk by 2-3 fold.
💡 Master This: Surveillance protocols after vascular intervention include duplex ultrasound at 1, 6, 12 months, then annually. Peak systolic velocity ratio >2.5 indicates >50% stenosis requiring reintervention consideration.
Evidence-based algorithms optimize individual outcomes, but understanding multi-system interactions enables management of complex patients with multiple comorbidities.
🔧 The Surgical Algorithm: Evidence-Based Vascular Interventions
🌐 The Systems Integration: Multi-Organ Vascular Interactions
📌 Remember: CARDIAC-RENAL-PULMONARY axis - Cardiac output >4 L/min, Arterial pressure >65 mmHg, Renal function GFR >60, Diuresis >0.5 mL/kg/hr, Inotropic support minimal, Acid-base balance, Creatinine stable, Respiratory rate <20, Eoxygenation >95%, No ventilator dependence, Alveolar-arterial gradient <300, Lung compliance normal
-
Cardiovascular-Renal Integration
- Cardiorenal syndrome affects 30% of vascular patients
- Type 1: Acute cardiac → acute renal failure
- Type 2: Chronic cardiac → chronic renal dysfunction
- Type 3: Acute renal → acute cardiac dysfunction
- Type 4: Chronic renal → chronic cardiac disease
- Type 5: Systemic disease → both organs
- Contrast-induced nephropathy prevention
- Pre-hydration: 1 mL/kg/hr normal saline 12 hours pre/post
- Contrast volume: <3 mL/kg or <300 mL total
- N-acetylcysteine: 600 mg BID × 2 days
- Sodium bicarbonate: 3 mL/kg/hr × 1 hour pre-procedure
- Cardiorenal syndrome affects 30% of vascular patients
-
Pulmonary-Cardiovascular Interactions
- Pulmonary hypertension complicates 15% of major vascular procedures
- Mean PAP >25 mmHg increases perioperative mortality 3-fold
- Right heart catheterization guides fluid management
- Inhaled nitric oxide: 20-40 ppm for acute management
- Ventilator weaning protocols post-operatively
- Spontaneous breathing trial criteria: PEEP ≤8, FiO2 ≤40%
- Rapid shallow breathing index: <105 predicts successful extubation
- Cuff leak test: >110 mL air leak prevents post-extubation stridor
- Pulmonary hypertension complicates 15% of major vascular procedures
| System | Normal Values | Dysfunction Threshold | Intervention Trigger | Monitoring Frequency |
|---|---|---|---|---|
| Cardiac | EF >55% | EF <40% | EF <30% | Daily echo |
| Renal | GFR >90 | GFR <60 | GFR <30 | BID creatinine |
| Pulmonary | FEV1 >80% | FEV1 <60% | FEV1 <40% | Q6h ABG |
| Hepatic | Bilirubin <1.2 | Bilirubin >2.0 | Bilirubin >5.0 | Daily LFTs |
| Hematologic | Hgb >12 | Hgb <10 | Hgb <8 | BID CBC |
💡 Master This: Goal-directed therapy protocols targeting cardiac index >2.5 L/min/m², oxygen delivery >600 mL/min/m², and mixed venous saturation >70% reduce major complications by 25-30% in high-risk vascular patients.
Multi-system optimization enables complex case management, leading to development of rapid assessment tools and clinical reference frameworks for immediate decision-making.
🌐 The Systems Integration: Multi-Organ Vascular Interactions
🎯 The Vascular Command Center: Rapid Assessment Mastery
📌 Remember: RAPID VASCULAR ASSESSMENT - Radial pulse check, Ankle-brachial index, Perfusion assessment, Imaging urgency, Doppler signals, Vital signs stability, Aneurysm palpation, Sensory examination, Capillary refill, Urgent laboratory, Limb temperature, Arterial blood gas, Renal function
-
Essential Clinical Arsenal
- Critical time windows: 6 hours limb ischemia, 3 hours stroke, 1 hour rupture
- Hemodynamic thresholds: MAP >65 mmHg, ABI >0.9, toe pressure >30 mmHg
- Laboratory triggers: Lactate >4 mmol/L, CK >1000 U/L, creatinine increase >0.5 mg/dL
- Imaging priorities: CTA for acute presentations, duplex for chronic disease
-
Rapid Decision Framework
- Immediate surgery indications
- Ruptured aneurysm: hemodynamic instability
- Acute limb ischemia: Category II-III Rutherford
- Compartment syndrome: pressure >30 mmHg
- Traumatic vascular injury: hard signs present
- Urgent intervention (<24 hours)
- Critical limb ischemia: rest pain or tissue loss
- Symptomatic carotid stenosis: >70% stenosis
- Expanding aneurysm: >1 cm/year growth
- Acute venous thrombosis: phlegmasia cerulea dolens
- Immediate surgery indications
| Clinical Scenario | Assessment Time | Decision Point | Intervention Window | Success Rate |
|---|---|---|---|---|
| Ruptured AAA | <5 minutes | Hemodynamic status | <60 minutes | 50-70% |
| Acute limb ischemia | <10 minutes | Rutherford category | <6 hours | 85-95% |
| Carotid stroke | <15 minutes | NIHSS score | <3 hours | 70-80% |
| Compartment syndrome | <20 minutes | Pressure measurement | <6 hours | 90-95% |
| Mesenteric ischemia | <30 minutes | Lactate level | <12 hours | 60-75% |
💡 Master This: GLASS classification for acute limb ischemia guides amputation risk: Grade I (viable) = <5% amputation, Grade IIa (marginally threatened) = 10-15% amputation, Grade IIb (immediately threatened) = 25-50% amputation, Grade III (irreversible) = >95% amputation.
This rapid assessment framework transforms complex vascular presentations into systematic, evidence-based management protocols that optimize patient outcomes while minimizing decision-making delays in critical situations.
🎯 The Vascular Command Center: Rapid Assessment Mastery
Practice Questions: Vascular Surgery
Test your understanding with these related questions
A 72-year-old woman comes to the physician for follow-up care. One year ago, she was diagnosed with a 3.8-cm infrarenal aortic aneurysm found incidentally on abdominal ultrasound. She has no complaints. She has hypertension, type 2 diabetes mellitus, and COPD. Current medications include hydrochlorothiazide, lisinopril, glyburide, and an albuterol inhaler. She has smoked a pack of cigarettes daily for 45 years. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 12/min, and blood pressure is 145/85 mm Hg. Examination shows a faint abdominal bruit on auscultation. Ultrasonography of the abdomen shows a 4.9-cm saccular dilation of the infrarenal aorta. Which of the following is the most appropriate next step in management?













