Urological trauma management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Urological trauma management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Urological trauma management US Medical PG Question 1: A 19-year-old man presents to the emergency department after a motor vehicle accident. The patient reports left shoulder pain that worsens with deep inspiration. Medical history is significant for a recent diagnosis of infectious mononucleosis. His temperature is 99°F (37.2°C), blood pressure is 80/55 mmHg, pulse is 115/min, and respiratory rate is 22/min. On physical exam, there is abdominal guarding, abdominal tenderness in the left upper quadrant, and rebound tenderness. The patient’s mucous membranes are dry and skin turgor is reduced. Which of the following most likely represents the acute changes in renal plasma flow (RPF) and glomerular filtration rate (GFR) in this patient?
- A. No change in RPF and decreased GFR
- B. Decreased RPF and decreased GFR (Correct Answer)
- C. No change in RPF and increased GFR
- D. Decreased RPF and no change in GFR
- E. No change in RPF and GFR
Urological trauma management Explanation: ***Decreased RPF and decreased GFR***
- This patient presents with signs of **hypovolemic shock** (hypotension with BP 80/55 mmHg, tachycardia, dry mucous membranes, reduced skin turgor) likely due to **splenic rupture** from the motor vehicle accident, exacerbated by splenomegaly from **infectious mononucleosis**.
- With a blood pressure of 80/55 mmHg (MAP ~73 mmHg), the patient is at or below the **lower limit of renal autoregulation** (~80 mmHg MAP).
- In acute hypovolemic shock, **renal blood flow and RPF decrease** due to systemic hypotension and **sympathetic vasoconstriction**.
- Although **angiotensin II-mediated efferent arteriolar constriction** attempts to preserve GFR by maintaining glomerular capillary pressure, this compensation is **insufficient** when MAP falls below the autoregulatory range.
- Result: **Both RPF and GFR decrease**, though GFR may be relatively preserved compared to the magnitude of RPF decrease initially.
*No change in RPF and decreased GFR*
- This scenario would suggest decreased filtration despite normal renal perfusion, implying a primary glomerular barrier problem.
- In hypovolemic shock, **RPF is always decreased** due to reduced systemic blood flow and renal vasoconstriction.
*Decreased RPF and no change in GFR*
- While renal autoregulation attempts to maintain stable GFR despite changes in blood pressure, this mechanism works only within the **autoregulatory range (MAP 80-180 mmHg)**.
- At BP 80/55 mmHg, autoregulation is overwhelmed, and **GFR will decrease** along with RPF.
*No change in RPF and increased GFR*
- An **increased GFR** is inconsistent with hypovolemic shock and would require either increased RPF or enhanced glomerular filtration pressure.
- Maintaining normal RPF during severe hypotension is physiologically implausible.
*No change in RPF and GFR*
- This suggests normal renal function despite **severe hypotension and hypovolemia**, which contradicts basic renal physiology.
- The body's compensatory mechanisms cannot fully maintain both RPF and GFR when systemic blood pressure falls below the autoregulatory threshold.
Urological trauma management US Medical PG Question 2: A 65-year-old man is brought to the emergency department by ambulance after falling during a hiking trip. He was hiking with friends when he fell off a 3 story ledge and was not able to be rescued until 6 hours after the accident. On arrival, he is found to have multiple lacerations as well as a pelvic fracture. His past medical history is significant for diabetes and benign prostatic hyperplasia, for which he takes metformin and prazosin respectively. Furthermore, he has a family history of autoimmune diseases. Selected lab results are shown below:
Serum:
Na+: 135 mEq/L
Creatinine: 1.5 mg/dL
Blood urea nitrogen: 37 mg/dL
Urine:
Na+: 13.5 mEq/L
Creatinine: 18 mg/dL
Osmolality: 580 mOsm/kg
Which of the following is the most likely cause of this patient's increased creatinine level?
- A. Autoimmune disease
- B. Compression of urethra by prostate
- C. Blood loss (Correct Answer)
- D. Diabetic nephropathy
- E. Rhabdomyolysis
Urological trauma management Explanation: ***Correct: Blood loss***
- The fall from a 3-story ledge and subsequent **pelvic fracture** indicate a high likelihood of significant **internal bleeding** and **hypovolemia**, leading to decreased renal perfusion and a pre-renal acute kidney injury (AKI) as evidenced by the elevated BUN/creatinine ratio (37/1.5 = 24.7), low urine sodium, and high urine osmolality.
- **Hypovolemia** from blood loss is a common cause of **pre-renal AKI**, characterized by the kidneys attempting to conserve fluid, resulting in concentrated urine with low sodium.
*Incorrect: Autoimmune disease*
- While a family history of autoimmune diseases exists, there is no direct evidence in the current presentation (e.g., specific markers, symptoms) to suggest an **autoimmune nephritis** as the acute cause of his renal dysfunction.
- Autoimmune causes of kidney injury typically present with proteinuria, hematuria, or other systemic inflammatory signs, which are not described.
*Incorrect: Compression of urethra by prostate*
- Although the patient has benign prostatic hyperplasia (BPH) and takes prazosin (an alpha-blocker to treat BPH), their current presentation of **pre-renal AKI** with concentrated urine does not fit typical **post-renal obstruction**.
- **Post-renal obstruction** from BPH would typically present with symptoms like difficulty urinating, elevated bladder volume, and often hydronephrosis, none of which are indicated here as the primary cause of acute renal failure.
*Incorrect: Diabetic nephropathy*
- The patient's history of diabetes makes **diabetic nephropathy** a potential cause of chronic kidney disease, but the **acute increase in creatinine** following a traumatic event strongly suggests an acute insult rather than a sudden exacerbation of chronic diabetic kidney disease.
- **Diabetic nephropathy** usually develops over years, presenting with proteinuria and a gradual decline in GFR, not an acute surge in creatinine following an injury, and it does not explain the pre-renal parameters seen in the urine.
*Incorrect: Rhabdomyolysis*
- While a severe fall could potentially cause **rhabdomyolysis** (muscle breakdown), the provided lab values do not include elevated **creatine kinase**, which is the hallmark of this condition.
- Although rhabdomyolysis can cause AKI, the **pre-renal parameters** (high BUN/Cr ratio, low urine Na, high urine osmolality) are more consistent with hypovolemia from blood loss rather than direct tubular injury from myoglobin.
Urological trauma management US Medical PG Question 3: A 79-year-old man with a history of prostate cancer is brought to the emergency department because of lower abdominal pain for 1 hour. He has not urinated for 24 hours. Abdominal examination shows a palpable bladder that is tender to palpation. A pelvic ultrasound performed by the emergency department resident confirms the diagnosis of acute urinary retention. An attempt to perform transurethral catheterization is unsuccessful. A urology consultation is ordered and the urologist plans to attempt suprapubic catheterization. As the urologist is called to see a different emergency patient, she asks the emergency department resident to obtain informed consent for the procedure. The resident recalls a lecture about the different modes of catheterization, but he has never seen or performed a suprapubic catheterization himself. Which of the following statements by the emergency department resident is the most appropriate?
- A. “I would prefer that you obtain informed consent when you become available again.” (Correct Answer)
- B. “Suprapubic catheterization is not the treatment of choice for this patient.”
- C. “I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency.”
- D. “I will make sure the patient reads and signs the informed consent form.”
- E. “I will ask the patient to waive informed consent because this is an urgent procedure.”
Urological trauma management Explanation: ***"I would prefer that you obtain informed consent when you become available again."***
- Informed consent requires that the person obtaining consent be **knowledgeable about the procedure**, its risks, benefits, and alternatives, and be able to answer the patient's questions thoroughly. The resident, having never performed or seen the procedure, cannot fulfill this requirement.
- The urologist, as the attending physician performing the procedure and the expert in suprapubic catheterization, is the most appropriate person to **educate the patient and obtain consent**.
*"Suprapubic catheterization is not the treatment of choice for this patient."*
- **Urethral catheterization is the first-line treatment for acute urinary retention**; however, it was unsuccessful.
- **Suprapubic catheterization is the appropriate next step** when transurethral catheterization fails or is contraindicated.
*"I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency."*
- There is **no legal prohibition** for a resident to obtain informed consent, provided they are competent to do so and have adequate knowledge of the procedure.
- The issue here is the resident's **lack of knowledge and experience** with the particular procedure, not their legal status as a resident.
*"I will make sure the patient reads and signs the informed consent form."*
- Simply having the patient read and sign a form is **insufficient for valid informed consent**.
- Informed consent is a **process of communication** that ensures the patient understands the procedure, not just a signature on a document.
*"I will ask the patient to waive informed consent because this is an urgent procedure."*
- While this is an urgent situation, it is **not an emergency that precludes obtaining informed consent**.
- **Waiving informed consent** is generally reserved for life-threatening emergencies where immediate intervention is required to save a patient's life and there is no time to obtain consent, which is not the case here.
Urological trauma management US Medical PG Question 4: A 58-year-old man presents to the emergency department following a motor vehicle accident where he was an unrestrained passenger. On initial presentation in the field, he had diffuse abdominal tenderness and his blood pressure is 70/50 mmHg and pulse is 129/min. Following administration of 2 L of normal saline, his blood pressure is 74/58 mmHg. He undergoes emergency laparotomy and the source of the bleeding is controlled. On the second post-operative day, his blood pressure is 110/71 mmHg and pulse is 90/min. There is a midline abdominal scar with no erythema and mild tenderness. Cardiopulmonary examination is unremarkable. He has had 300 mL of urine output over the last 24 hours. Urinalysis shows 12-15 RBC/hpf, 2-5 WBC/hpf, and trace protein. What additional finding would you expect to see on urinalysis?
- A. WBC casts
- B. RBC casts
- C. Fatty casts
- D. Hyaline casts
- E. Muddy brown casts (Correct Answer)
Urological trauma management Explanation: ***Muddy brown casts***
- The patient's history of **post-traumatic hypovolemic shock** leading to prolonged hypotension, coupled with **oliguria** and an elevated blood pressure on post-operative day 2, are highly suggestive of **acute tubular necrosis (ATN)**.
- **Muddy brown granular casts** are a hallmark finding of ATN, representing sloughed renal tubular cells and heme pigments.
*WBC casts*
- **WBC casts** are characteristic of **pyelonephritis** or **interstitial nephritis**, often accompanied by fever, flank pain, and significant pyuria, none of which are the primary presentation here.
- While there are some WBCs in the urine, the overall clinical picture does not point towards an infectious or inflammatory renal process as the primary cause of renal dysfunction.
*RBC casts*
- **RBC casts** indicate **glomerulonephritis** or severe tubular damage with hemorrhage, suggesting glomerular inflammation or a vasculitic process.
- While the urinalysis shows 12-15 RBC/hpf, the absence of other strong indicators of glomerular disease and the prominent history of shock make ATN a more likely diagnosis than glomerulonephritis.
*Fatty casts*
- **Fatty casts** are typically seen in **nephrotic syndrome**, associated with significant proteinuria (>3.5g/day), hyperlipidemia, and edema.
- The patient's trace proteinuria and the absence of other nephrotic syndrome features make this finding unlikely.
*Hyaline casts*
- **Hyaline casts** are composed of Tamm-Horsfall mucoprotein and can be found in **healthy individuals** as well as in states of **dehydration** or mild renal injury.
- While the patient was likely dehydrated, hyaline casts are non-specific and do not explain the degree of renal dysfunction and oliguria observed in this case.
Urological trauma management US Medical PG Question 5: A 40-year-old woman was admitted to the surgical service after an uncomplicated appendectomy. She underwent surgery yesterday and had an uneventful postoperative course. However, she now complains that she is unable to completely void. She also complains of pain in the suprapubic area. You examine her and confirm the tenderness and fullness in the suprapubic region. You ask the nurse to perform a bladder scan, which reveals 450cc. What is the next appropriate step in management?
- A. Catheterization (Correct Answer)
- B. Oral bethanechol chloride
- C. Neostigmine methylsulfate injection
- D. Intravenous furosemide
- E. Intravenous neostigmine methylsulfate
Urological trauma management Explanation: **Catheterization**
- The patient is presenting with **acute urinary retention**, confirmed by the inability to void, suprapubic pain, and a bladder scan showing 450cc, which exceeds the typical threshold for intervention (often 200-300cc).
- **Immediate catheterization** (usually Foley catheterization) is necessary to drain the bladder, relieve discomfort, and prevent complications like bladder distension injury or hydronephrosis.
*Oral bethanechol chloride*
- Bethanechol is a **cholinergic agonist** used to stimulate bladder contraction in cases of hypotonic bladder, but it is not appropriate for acute, complete urinary retention requiring immediate drainage.
- Its onset of action is too slow for the urgency of acute retention, and it would not resolve the immediate discomfort or risk of bladder damage.
*Neostigmine methylsulfate injection*
- Neostigmine is an **acetylcholinesterase inhibitor** that increases acetylcholine levels, potentially improving bladder contractility, but it is not typically the first-line treatment for acute postoperative urinary retention.
- Like bethanechol, it doesn't provide the rapid relief of bladder distension that catheterization does and is more often considered for chronic or neurogenic bladder dysfunction once acute retention is managed.
*Intravenous furosemide*
- Furosemide is a **loop diuretic** that increases urine production, which would exacerbate the problem in a patient with acute urinary retention.
- Increasing urine output without the ability to void would worsen bladder distension and patient discomfort, making it a contraindicated intervention.
*Intravenous neostigmine methylsulfate*
- While neostigmine can be given intravenously, its use in acute postoperative urinary retention is **not a primary treatment**.
- Its effect is slower than direct bladder drainage, and the immediate priority is to decompress the bladder to relieve symptoms and prevent complications.
Urological trauma management US Medical PG Question 6: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Urological trauma management Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Urological trauma management US Medical PG Question 7: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Urological trauma management Explanation: ***Bulbous urethra***
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
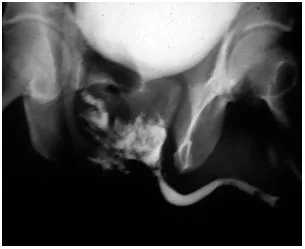
Urological trauma management US Medical PG Question 8: A 40-year-old sailor is brought to a military treatment facility 20 minutes after being involved in a navy ship collision. He appears ill. He reports a sensation that he needs to urinate but is unable to void. His pulse is 140/min, respirations are 28/min, and blood pressure is 104/70 mm Hg. Pelvic examination shows ecchymoses over the scrotum and perineum. There is tenderness over the suprapubic region and blood at the urethral meatus. Digital rectal examination shows a high-riding prostate. Abdominal ultrasound shows a moderately distended bladder. X-rays of the pelvis show fractures of all four pubic rami. Which of the following is the most likely cause of this patient's symptoms?
- A. Tearing of the anterior urethra
- B. Rupture of the corpus cavernosum
- C. Tearing of the posterior urethra (Correct Answer)
- D. Tearing of the ureter
- E. Rupture of the bladder
Urological trauma management Explanation: ***Tearing of the posterior urethra***
- The combination of **pelvic fractures**, **blood at the urethral meatus**, inability to void despite a sensation to do so, and a **high-riding prostate** are classic signs of posterior urethral injury.
- The posterior urethra, particularly the membranous portion, is vulnerable to shear forces and tearing during severe pelvic trauma.
*Tearing of the anterior urethra*
- Anterior urethral injuries are typically associated with a **straddle injury** or direct trauma to the perineum, not necessarily pelvic fractures.
- While blood at the meatus can occur, the **high-riding prostate** and extensive pelvic fractures point away from an isolated anterior injury.
*Rupture of the corpus cavernosum*
- This is usually a result of "penile fracture" during sexual intercourse and presents with sudden pain, detumescence, and a characteristic "eggplant" deformity, which are not described here.
- It does not explain the inability to void, high-riding prostate, or association with pelvic fractures.
*Tearing of the ureter*
- Ureteral injuries are typically associated with penetrating trauma or iatrogenic injury during surgery; they rarely occur with blunt pelvic trauma of this nature.
- Symptoms would include flank pain, hematuria, or urine leakage into the retroperitoneum, not significant urethral bleeding or a high-riding prostate.
*Rupture of the bladder*
- Bladder rupture can be intra- or extraperitoneal and is often associated with pelvic fractures. However, it typically causes gross hematuria and often free fluid in the peritoneum (intraperitoneal rupture) or extravasation into the space of Retzius (extraperitoneal rupture).
- While a distended bladder is noted, the presence of **blood at the urethral meatus** and a **high-riding prostate** strongly implicate urethral injury rather than primarily bladder rupture.
Urological trauma management US Medical PG Question 9: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Urological trauma management Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Urological trauma management US Medical PG Question 10: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Urological trauma management Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
More Urological trauma management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.