Urinary retention management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Urinary retention management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Urinary retention management US Medical PG Question 1: A 37-year-old woman presents with an inability to void in the hours after giving birth to her first child via vaginal delivery. Her delivery involved the use of epidural anesthesia as well as pelvic trauma from the use of forceps. She is currently experiencing urinary leakage and complains of increased lower abdominal pressure. Which of the following is the most appropriate treatment for this patient’s condition?
- A. Pessary insertion
- B. Pelvic floor muscle strengthening
- C. Antimuscarinic drugs
- D. Midurethral sling
- E. Urethral catheterization (Correct Answer)
Urinary retention management Explanation: ***Urethral catheterization***
- The patient is experiencing **postpartum urinary retention** (inability to void) and **overflow incontinence** (urinary leakage due to bladder overdistension), alongside increased lower abdominal pressure, all indicative of an overfilled bladder.
- **Urethral catheterization** is the most appropriate immediate treatment to relieve bladder distension, prevent kidney damage, and allow bladder recovery.
*Pessary insertion*
- **Pessaries** are used for pelvic organ prolapse or stress urinary incontinence, not for acute postpartum urinary retention.
- They provide structural support but do not address the inability to void in an overdistended bladder.
*Pelvic floor muscle strengthening*
- **Pelvic floor exercises** are beneficial for stress incontinence or mild degrees of prolapse.
- They are contraindicated in acute urinary retention as they may worsen the inability to void if the issue is a failure of bladder contractility or urethral relaxation.
*Antimuscarinic drugs*
- **Antimuscarinics** relax the detrusor muscle and are used to treat overactive bladder symptoms (e.g., urgency, frequency).
- They would worsen bladder emptying in a patient with urinary retention.
*Midurethral sling*
- A **midurethral sling** is a surgical procedure for stress urinary incontinence.
- It is an invasive treatment for a chronic condition and is not appropriate for acute postpartum urinary retention.
Urinary retention management US Medical PG Question 2: A 65-year-old man is brought to the emergency department by ambulance after falling during a hiking trip. He was hiking with friends when he fell off a 3 story ledge and was not able to be rescued until 6 hours after the accident. On arrival, he is found to have multiple lacerations as well as a pelvic fracture. His past medical history is significant for diabetes and benign prostatic hyperplasia, for which he takes metformin and prazosin respectively. Furthermore, he has a family history of autoimmune diseases. Selected lab results are shown below:
Serum:
Na+: 135 mEq/L
Creatinine: 1.5 mg/dL
Blood urea nitrogen: 37 mg/dL
Urine:
Na+: 13.5 mEq/L
Creatinine: 18 mg/dL
Osmolality: 580 mOsm/kg
Which of the following is the most likely cause of this patient's increased creatinine level?
- A. Autoimmune disease
- B. Compression of urethra by prostate
- C. Blood loss (Correct Answer)
- D. Diabetic nephropathy
- E. Rhabdomyolysis
Urinary retention management Explanation: ***Correct: Blood loss***
- The fall from a 3-story ledge and subsequent **pelvic fracture** indicate a high likelihood of significant **internal bleeding** and **hypovolemia**, leading to decreased renal perfusion and a pre-renal acute kidney injury (AKI) as evidenced by the elevated BUN/creatinine ratio (37/1.5 = 24.7), low urine sodium, and high urine osmolality.
- **Hypovolemia** from blood loss is a common cause of **pre-renal AKI**, characterized by the kidneys attempting to conserve fluid, resulting in concentrated urine with low sodium.
*Incorrect: Autoimmune disease*
- While a family history of autoimmune diseases exists, there is no direct evidence in the current presentation (e.g., specific markers, symptoms) to suggest an **autoimmune nephritis** as the acute cause of his renal dysfunction.
- Autoimmune causes of kidney injury typically present with proteinuria, hematuria, or other systemic inflammatory signs, which are not described.
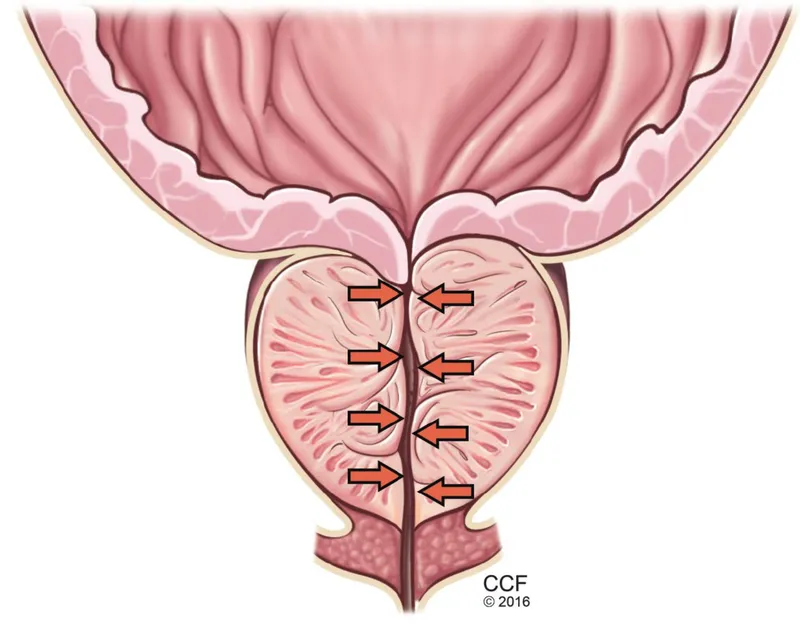
*Incorrect: Compression of urethra by prostate*
- Although the patient has benign prostatic hyperplasia (BPH) and takes prazosin (an alpha-blocker to treat BPH), their current presentation of **pre-renal AKI** with concentrated urine does not fit typical **post-renal obstruction**.
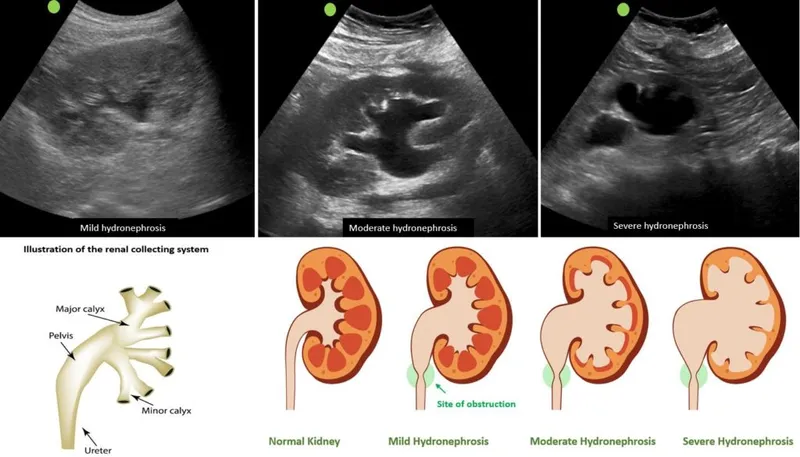
- **Post-renal obstruction** from BPH would typically present with symptoms like difficulty urinating, elevated bladder volume, and often hydronephrosis, none of which are indicated here as the primary cause of acute renal failure.
*Incorrect: Diabetic nephropathy*
- The patient's history of diabetes makes **diabetic nephropathy** a potential cause of chronic kidney disease, but the **acute increase in creatinine** following a traumatic event strongly suggests an acute insult rather than a sudden exacerbation of chronic diabetic kidney disease.
- **Diabetic nephropathy** usually develops over years, presenting with proteinuria and a gradual decline in GFR, not an acute surge in creatinine following an injury, and it does not explain the pre-renal parameters seen in the urine.
*Incorrect: Rhabdomyolysis*
- While a severe fall could potentially cause **rhabdomyolysis** (muscle breakdown), the provided lab values do not include elevated **creatine kinase**, which is the hallmark of this condition.
- Although rhabdomyolysis can cause AKI, the **pre-renal parameters** (high BUN/Cr ratio, low urine Na, high urine osmolality) are more consistent with hypovolemia from blood loss rather than direct tubular injury from myoglobin.
Urinary retention management US Medical PG Question 3: A 65-year-old woman comes to the physician for the evaluation of several episodes of urinary incontinence over the past several months. She reports that she was not able to get to the bathroom in time. During the past 6 months, her husband has noticed that she is starting to forget important appointments and family meetings. She has type 2 diabetes mellitus treated with metformin. The patient had smoked a pack of cigarettes daily for 45 years. Her vital signs are within normal limits. On mental status examination, she is confused and has short-term memory deficits. She walks slowly taking short, wide steps. Muscle strength is normal. Deep tendon reflexes are 2+ bilaterally. Which of the following is the most likely underlying cause of this patient's urinary incontinence?
- A. Bacterial infection of the urinary tract
- B. Normal pressure hydrocephalus (Correct Answer)
- C. Detrusor-sphincter dyssynergia
- D. Impaired detrusor contractility
- E. Loss of sphincter function
Urinary retention management Explanation: ***Normal pressure hydrocephalus***
- The patient's presentation with **urinary incontinence**, **memory deficits/dementia**, and an **ataxic gait** (slow, short, wide steps) represents the classic triad of **Normal Pressure Hydrocephalus (NPH)**.
- While the incontinence itself is urge-type (not getting to the bathroom in time), the constellation of symptoms points to NPH as the underlying neurological cause.
*Bacterial infection of the urinary tract*
- Although urinary tract infections can cause **acute urinary incontinence**, especially in the elderly, they do not explain the accompanying **memory loss** and **gait disturbance**.
- There are no symptoms typical of infection such as **dysuria**, **frequency**, or **fever** mentioned in the vignette.
*Detrusor-sphincter dyssynergia*
- This condition involves involuntary contraction of the urethral sphincter during detrusor contraction, typically seen in **spinal cord injury** patients, and is characterized by **incomplete bladder emptying**, not primarily urge incontinence alone.
- It does not account for the **cognitive decline** or **gait abnormalities** presented.
*Impaired detrusor contractility*
- **Impaired detrusor contractility** (underactive bladder) typically leads to **overflow incontinence** with incomplete emptying, characterized by a constant dribble and difficulty initiating urination, which contrasts with the presented urge incontinence.
- This condition does not explain the patient's **dementia** or **gait disturbance**.
*Loss of sphincter function*
- **Loss of sphincter function** (stress incontinence) typically causes urine leakage with increased intra-abdominal pressure (e.g., coughing, sneezing, lifting), which is different from the patient's report of not making it to the bathroom in time which points towards urge incontinence.
- This condition also does not explain the neurological symptoms of **dementia** and **gait ataxia**.
Urinary retention management US Medical PG Question 4: A 72-year-old multiparous woman comes to the physician for the evaluation of episodes of involuntary urine leakage for the past 6 months. She loses small amounts of urine without warning after laughing or sneezing. She also sometimes forgets the names of her grandchildren and friends. She is retired and lives at an assisted-living facility. She has insulin-dependent diabetes mellitus type 2. Her mother received a ventriculoperitoneal shunt around her age. She walks without any problems. Sensation to pinprick and light touch is normal. Which of the following is the primary underlying etiology for this patient's urinary incontinence?
- A. Urethral hypermobility (Correct Answer)
- B. Decreased cerebrospinal fluid absorption
- C. Detrusor-sphincter dyssynergia
- D. Impaired detrusor contractility
- E. Loss of sphincter control
Urinary retention management Explanation: ***Urethral hypermobility***
- This patient presents with **stress urinary incontinence**, characterized by involuntary urine leakage during activities that increase intra-abdominal pressure, such as **laughing or sneezing**.
- **Urethral hypermobility** is a common cause of stress incontinence, where the urethra and bladder neck rotate downward and backward during increased abdominal pressure, compromising sphincter function.
*Decreased cerebrospinal fluid absorption*
- This is linked to **normal pressure hydrocephalus**, presenting with a triad of **gait disturbance**, **urinary incontinence**, and **dementia**.
- While the patient has incontinence and memory issues, her normal gait and the absence of clear hydrocephalus symptoms makes this less likely to be the primary cause of her specific type of incontinence.
*Detrusor-sphincter dyssynergia*
- This condition involves uncoordinated contraction of the **detrusor muscle** and external urethral sphincter, typically seen in individuals with **neurological disorders** like spinal cord injury.
- It results in incomplete bladder emptying and usually presents with urgency, frequency, and overflow incontinence, which does not match the patient's symptoms of leakage with straining.
*Impaired detrusor contractility*
- This leads to **overflow incontinence**, where the bladder is unable to empty completely and continuously leaks urine.
- Symptoms usually include a weak stream, hesitancy, and a feeling of incomplete emptying, which are not described in this patient.
*Loss of sphincter control*
- This can cause **stress incontinence**, but the term "loss of sphincter control" is a broad description. **Urethral hypermobility** specifically describes the mechanical mechanism leading to the loss of effective sphincter closure during exertion.
- While related, urethral hypermobility is a more specific and accurate primary etiology for stress incontinence in this context.
Urinary retention management US Medical PG Question 5: A 40-year-old woman was admitted to the surgical service after an uncomplicated appendectomy. She underwent surgery yesterday and had an uneventful postoperative course. However, she now complains that she is unable to completely void. She also complains of pain in the suprapubic area. You examine her and confirm the tenderness and fullness in the suprapubic region. You ask the nurse to perform a bladder scan, which reveals 450cc. What is the next appropriate step in management?
- A. Catheterization (Correct Answer)
- B. Oral bethanechol chloride
- C. Neostigmine methylsulfate injection
- D. Intravenous furosemide
- E. Intravenous neostigmine methylsulfate
Urinary retention management Explanation: **Catheterization**
- The patient is presenting with **acute urinary retention**, confirmed by the inability to void, suprapubic pain, and a bladder scan showing 450cc, which exceeds the typical threshold for intervention (often 200-300cc).
- **Immediate catheterization** (usually Foley catheterization) is necessary to drain the bladder, relieve discomfort, and prevent complications like bladder distension injury or hydronephrosis.
*Oral bethanechol chloride*
- Bethanechol is a **cholinergic agonist** used to stimulate bladder contraction in cases of hypotonic bladder, but it is not appropriate for acute, complete urinary retention requiring immediate drainage.
- Its onset of action is too slow for the urgency of acute retention, and it would not resolve the immediate discomfort or risk of bladder damage.
*Neostigmine methylsulfate injection*
- Neostigmine is an **acetylcholinesterase inhibitor** that increases acetylcholine levels, potentially improving bladder contractility, but it is not typically the first-line treatment for acute postoperative urinary retention.
- Like bethanechol, it doesn't provide the rapid relief of bladder distension that catheterization does and is more often considered for chronic or neurogenic bladder dysfunction once acute retention is managed.
*Intravenous furosemide*
- Furosemide is a **loop diuretic** that increases urine production, which would exacerbate the problem in a patient with acute urinary retention.
- Increasing urine output without the ability to void would worsen bladder distension and patient discomfort, making it a contraindicated intervention.
*Intravenous neostigmine methylsulfate*
- While neostigmine can be given intravenously, its use in acute postoperative urinary retention is **not a primary treatment**.
- Its effect is slower than direct bladder drainage, and the immediate priority is to decompress the bladder to relieve symptoms and prevent complications.
Urinary retention management US Medical PG Question 6: A 55-year-old woman with type 1 diabetes mellitus comes to the physician because of a 3-month history of progressively worsening urinary incontinence. She has started to wear incontinence pads because of frequent involuntary dribbling of urine that occurs even when resting. She has the sensation of a full bladder even after voiding. Her only medication is insulin. Physical examination shows a palpable suprapubic mass. Urinalysis is unremarkable. Urodynamic studies show an increased post-void residual volume. Which of the following interventions is most likely to benefit this patient?
- A. Prazosin therapy
- B. Duloxetine therapy
- C. Oxybutynin therapy
- D. Intermittent catheterization (Correct Answer)
- E. Amitriptyline therapy
Urinary retention management Explanation: ***Intermittent catheterization***
- This patient presents with symptoms and findings consistent with **overflow incontinence** due to **diabetic autonomic neuropathy** affecting bladder function.
- Intermittent catheterization is the most effective intervention for managing **high post-void residual volumes** and preventing complications like UTIs and kidney damage in such cases.
*Prazosin therapy*
- **Prazosin** is an alpha-1 adrenergic antagonist, typically used to treat **hypertension** and **benign prostatic hyperplasia**.
- While it can relax the bladder neck, it is not the primary treatment for overflow incontinence due to impaired detrusor contractility and a high post-void residual.
*Duloxetine therapy*
- **Duloxetine** is a serotonin-norepinephrine reuptake inhibitor (SNRI) primarily used to treat **stress incontinence** by increasing urethral sphincter tone.
- It would not address the underlying issue of poor bladder emptying and high post-void residual volume in this patient.
*Oxybutynin therapy*
- **Oxybutynin** is an anticholinergic medication used to treat **urge incontinence** by reducing involuntary detrusor contractions.
- In this case of overflow incontinence, it could worsen bladder emptying by further inhibiting detrusor muscle contraction.
*Amitriptyline therapy*
- **Amitriptyline** is a tricyclic antidepressant that can have anticholinergic effects and is occasionally used for **nocturia** or **neuropathic pain**.
- It is not indicated for the management of overflow incontinence due to poor bladder emptying and could potentially exacerbate urinary retention.
Urinary retention management US Medical PG Question 7: A 68-year-old woman comes to the physician for the evaluation of loss of urine for the last year. The patient states that she loses control over her bladder when walking or standing up. She reports frequent, small-volume urine losses with no urge to urinate prior to the leakage. She tried to strengthen her pelvic muscles with supervised Kegel exercises and using a continence pessary but her symptoms did not improve. The patient is sexually active with her husband. She has type 2 diabetes mellitus controlled with metformin. She does not smoke or drink alcohol. Vital signs are within normal limits. Her hemoglobin A1c is 6.3% and fingerstick blood glucose concentration is 110 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
- A. Tighter glycemic control
- B. Urethral sling (Correct Answer)
- C. Topical vaginal estrogen
- D. Biofeedback
- E. Urethropexy
Urinary retention management Explanation: ***Urethral sling***
- The patient exhibits symptoms consistent with **stress urinary incontinence**, characterized by urine leakage with increased intra-abdominal pressure (e.g., walking, standing), especially since conservative measures have failed.
- A **urethral sling** is a highly effective surgical treatment for stress urinary incontinence, providing support to the urethra and bladder neck.
*Tighter glycemic control*
- While uncontrolled diabetes can contribute to **polyuria** and **diabetic neuropathy** affecting bladder function, this patient's diabetes is well-controlled (HbA1c 6.3%).
- Tighter glycemic control is unlikely to resolve symptoms of stress urinary incontinence when the primary issue is anatomical support.
*Topical vaginal estrogen*
- **Topical vaginal estrogen** is effective for genitourinary syndrome of menopause, which can cause **vaginal atrophy** and **urge incontinence** symptoms.
- It is not the primary treatment for stress urinary incontinence, especially after the failure of conservative measures.
*Biofeedback*
- **Biofeedback** is often used in conjunction with **pelvic floor muscle training** (Kegel exercises) to improve patient awareness and control of these muscles.
- The patient has already tried supervised Kegel exercises without improvement, suggesting that biofeedback alone is unlikely to be sufficient.
*Urethropexy*
- **Urethropexy** is a surgical procedure that repositions and supports the urethra, similar in principle to a urethral sling.
- While it is a surgical option for stress incontinence, **urethral slings** (midurethral slings) are generally preferred due to their high efficacy and minimally invasive nature compared to traditional urethropexy procedures.
Urinary retention management US Medical PG Question 8: A 67-year-old man presents to the emergency department with trouble urinating. The patient states that in general he has had difficulty urinating but recently, it has taken significant effort for him to initiate a urinary stream. He finds himself unable to completely void and states he has suprapubic tenderness as a result. These symptoms started suddenly 3 days ago. The patient has a history of benign prostatic hyperplasia, constipation, and diabetes mellitus. His current medications include finasteride, sodium docusate, and hydrochlorothiazide. He recently started taking phenylephrine for seasonal allergies. The patient’s last bowel movement was 2 days ago. His temperature is 99.0°F (37.2°C), blood pressure is 167/98 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 100% on room air. Physical exam is notable for suprapubic tenderness, and an ultrasound reveals 750 mL of fluid in the bladder. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Prostatic adenocarcinoma
- B. Medication-induced symptoms (Correct Answer)
- C. Constipation
- D. Urinary tract infection
- E. Worsening benign prostatic hypertrophy
Urinary retention management Explanation: ***Medication-induced symptoms***
- The patient recently started **phenylephrine**, an **alpha-1 adrenergic agonist**, which can cause **urethral constriction** and worsen urinary outflow obstruction, especially in patients with BPH.
- The **sudden onset** of severe urinary retention, leading to suprapubic tenderness and a distended bladder (750 mL), is highly suggestive of a medication side effect given his existing BPH.
*Prostatic adenocarcinoma*
- While prostatic adenocarcinoma can cause urinary symptoms, these typically develop **gradually** and are less likely to present with such an acute, severe urinary retention episode.
- There are no other features like **weight loss**, **bone pain**, or abnormal **PSA levels** mentioned to suggest malignancy.
*Constipation*
- Although **severe constipation** can sometimes exacerbate urinary symptoms by physical compression on the bladder, the patient's last bowel movement was 2 days ago, which is not severe enough to cause acute urinary retention of this magnitude.
- The primary cause of his urinary symptoms is more likely related to bladder outflow obstruction rather than external compression from constipation.
*Urinary tract infection*
- A UTI typically presents with symptoms like **dysuria**, **frequency**, **urgency**, **fever**, and **chills**, none of which are prominent here.
- While a UTI can cause some urinary difficulty, it's less likely to be the sole cause of such acute and severe urinary retention or a bladder volume of 750 mL without other infection signs.
*Worsening benign prostatic hypertrophy*
- Although the patient has BPH and is on finasteride, a **sudden dramatic worsening** over 3 days, leading to complete inability to void and a large bladder volume, is less typical for a gradual disease progression.
- The acute change points more strongly to an **exacerbating factor**, such as a new medication, rather than a natural progression of BPH.
Urinary retention management US Medical PG Question 9: A 59-year-old man comes to the physician because of a 3-month history of frequent urination. He has to urinate every 1–2 hours during the day and wakes up at least 2–3 times at night to urinate. He also reports that over the last 2 months, he has difficulty initiating micturition and the urinary stream is weak, with prolonged terminal dribbling. His pulse is 72/min, and blood pressure is 158/105 mm Hg. Rectal exam shows a smooth, symmetrically enlarged prostate without any tenderness or irregularities. Prostate-specific antigen is within the reference range and urinalysis shows no abnormalities. A postvoid ultrasound shows a residual bladder volume of 110 mL. Which of the following is the most appropriate next step in management?
- A. Transurethral resection of the prostate
- B. Terazosin therapy (Correct Answer)
- C. Bladder catheterization
- D. Finasteride therapy
- E. Cystoscopy
Urinary retention management Explanation: ***Terazosin therapy***
- Terazosin is an **alpha-1 adrenergic antagonist** that blocks receptors in the prostate and bladder neck, causing relaxation of the smooth muscle and improving urinary flow. This is a first-line medical treatment for symptomatic **benign prostatic hyperplasia (BPH)**.
- The patient presents with **obstructive and irritative lower urinary tract symptoms (LUTS)**, a symmetrically enlarged prostate, and a postvoid residual volume that indicates bladder outlet obstruction, all consistent with BPH.
- Alpha-blockers provide **rapid symptom relief** (within days to weeks) and may also help with the patient's **elevated blood pressure** (158/105 mm Hg).
*Transurethral resection of the prostate*
- **Transurethral resection of the prostate (TURP)** is a surgical intervention reserved for patients with severe BPH symptoms refractory to medical therapy or those with complications like recurrent urinary retention or renal dysfunction.
- Given that the patient has not yet tried medical therapy, and his symptoms are not immediately life-threatening, surgery is not the most appropriate first step.
*Bladder catheterization*
- **Bladder catheterization** is indicated for acute urinary retention or in cases of severe bladder obstruction leading to renal impairment.
- While the patient has significant LUTS and a postvoid residual volume, he is not in acute urinary retention, so immediate catheterization is not necessary as a long-term management strategy.
*Finasteride therapy*
- **Finasteride** is a **5-alpha reductase inhibitor** that reduces prostate size by inhibiting the conversion of testosterone to dihydrotestosterone. It is more effective in patients with larger prostate volumes and takes several months to show its full effect.
- Though a valid treatment for BPH, alpha-blockers like terazosin provide faster symptomatic relief by addressing dynamic obstruction and are generally preferred as initial therapy, often in combination with 5-alpha reductase inhibitors for larger prostates.
*Cystoscopy*
- **Cystoscopy** is an invasive procedure used to visualize the bladder and urethra directly. It is typically reserved for cases where there is suspicion of other pathologies like bladder stones, strictures, or bladder cancer, or for preoperative planning.
- The patient's symptoms and examination findings are consistent with BPH, and his PSA is normal, so primary cystoscopy is not indicated as the next step in management.
Urinary retention management US Medical PG Question 10: A 65-year-old African American man presents for follow-up examination with a 6-month history of urinary hesitancy, weak stream, and terminal dribbling, which is refractory to a combination therapy of finasteride and tamsulosin. The patient’s past medical history is otherwise unremarkable. His father and brother were diagnosed with prostate cancer at the age of 55 years. His vital signs are within normal limits. The patient has a normal anal sphincter tone and a bulbocavernosus muscle reflex. Digital rectal exam (DRE) reveals a prostate size equivalent to 2 finger pads with a hard nodule and without fluctuance or tenderness. Serum prostate-specific antigen (PSA) level is 5 ng/mL. Which of the following investigations is most likely to establish a definitive diagnosis?
- A. Magnetic resonance imaging (MRI)
- B. 4Kscore test
- C. Prostate Health Index (PHI)
- D. Image-guided needle biopsy (Correct Answer)
- E. PSA in 3 months
Urinary retention management Explanation: ***Image-guided needle biopsy***
- A definitive diagnosis of **prostate cancer** requires histological confirmation, which is achieved through a **biopsy**.
- The patient's presentation with a **hard nodule** on DRE, elevated PSA, and a strong family history of prostate cancer, despite treatment for BPH, strongly indicates the need for a biopsy.
*Magnetic resonance imaging (MRI)*
- While MRI can help in **staging prostate cancer** and guiding biopsies, it does not provide a definitive diagnosis on its own.
- An MRI may identify suspicious lesions but **cannot confirm malignancy** without tissue sampling.
*4Kscore test*
- The 4Kscore test estimates the **risk of high-grade prostate cancer** but does not provide a definitive diagnosis.
- It uses a panel of four prostate-specific kallikrein proteins, along with patient age, DRE status, and prior biopsy results, to calculate a risk score.
*Prostate Health Index (PHI)*
- The PHI is a blood test that combines total PSA, free PSA, and [-2]proPSA to assess the **probability of prostate cancer**.
- It helps in deciding whether a biopsy is needed, but like the 4Kscore, it is not a diagnostic tool in itself.
*PSA in 3 months*
- Re-checking PSA in 3 months would **delay definitive diagnosis** and treatment for a potentially aggressive cancer, especially given the palpable nodule and family history.
- The current PSA of 5 ng/mL, although not extremely high, combined with the suspicious DRE finding, warrants more immediate action.
More Urinary retention management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.