Urethral injury management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Urethral injury management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Urethral injury management US Medical PG Question 1: A 79-year-old man with a history of prostate cancer is brought to the emergency department because of lower abdominal pain for 1 hour. He has not urinated for 24 hours. Abdominal examination shows a palpable bladder that is tender to palpation. A pelvic ultrasound performed by the emergency department resident confirms the diagnosis of acute urinary retention. An attempt to perform transurethral catheterization is unsuccessful. A urology consultation is ordered and the urologist plans to attempt suprapubic catheterization. As the urologist is called to see a different emergency patient, she asks the emergency department resident to obtain informed consent for the procedure. The resident recalls a lecture about the different modes of catheterization, but he has never seen or performed a suprapubic catheterization himself. Which of the following statements by the emergency department resident is the most appropriate?
- A. “I would prefer that you obtain informed consent when you become available again.” (Correct Answer)
- B. “Suprapubic catheterization is not the treatment of choice for this patient.”
- C. “I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency.”
- D. “I will make sure the patient reads and signs the informed consent form.”
- E. “I will ask the patient to waive informed consent because this is an urgent procedure.”
Urethral injury management Explanation: ***"I would prefer that you obtain informed consent when you become available again."***
- Informed consent requires that the person obtaining consent be **knowledgeable about the procedure**, its risks, benefits, and alternatives, and be able to answer the patient's questions thoroughly. The resident, having never performed or seen the procedure, cannot fulfill this requirement.
- The urologist, as the attending physician performing the procedure and the expert in suprapubic catheterization, is the most appropriate person to **educate the patient and obtain consent**.
*"Suprapubic catheterization is not the treatment of choice for this patient."*
- **Urethral catheterization is the first-line treatment for acute urinary retention**; however, it was unsuccessful.
- **Suprapubic catheterization is the appropriate next step** when transurethral catheterization fails or is contraindicated.
*"I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency."*
- There is **no legal prohibition** for a resident to obtain informed consent, provided they are competent to do so and have adequate knowledge of the procedure.
- The issue here is the resident's **lack of knowledge and experience** with the particular procedure, not their legal status as a resident.
*"I will make sure the patient reads and signs the informed consent form."*
- Simply having the patient read and sign a form is **insufficient for valid informed consent**.
- Informed consent is a **process of communication** that ensures the patient understands the procedure, not just a signature on a document.
*"I will ask the patient to waive informed consent because this is an urgent procedure."*
- While this is an urgent situation, it is **not an emergency that precludes obtaining informed consent**.
- **Waiving informed consent** is generally reserved for life-threatening emergencies where immediate intervention is required to save a patient's life and there is no time to obtain consent, which is not the case here.
Urethral injury management US Medical PG Question 2: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Urethral injury management Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
Urethral injury management US Medical PG Question 3: A 40-year-old woman was admitted to the surgical service after an uncomplicated appendectomy. She underwent surgery yesterday and had an uneventful postoperative course. However, she now complains that she is unable to completely void. She also complains of pain in the suprapubic area. You examine her and confirm the tenderness and fullness in the suprapubic region. You ask the nurse to perform a bladder scan, which reveals 450cc. What is the next appropriate step in management?
- A. Catheterization (Correct Answer)
- B. Oral bethanechol chloride
- C. Neostigmine methylsulfate injection
- D. Intravenous furosemide
- E. Intravenous neostigmine methylsulfate
Urethral injury management Explanation: **Catheterization**
- The patient is presenting with **acute urinary retention**, confirmed by the inability to void, suprapubic pain, and a bladder scan showing 450cc, which exceeds the typical threshold for intervention (often 200-300cc).
- **Immediate catheterization** (usually Foley catheterization) is necessary to drain the bladder, relieve discomfort, and prevent complications like bladder distension injury or hydronephrosis.
*Oral bethanechol chloride*
- Bethanechol is a **cholinergic agonist** used to stimulate bladder contraction in cases of hypotonic bladder, but it is not appropriate for acute, complete urinary retention requiring immediate drainage.
- Its onset of action is too slow for the urgency of acute retention, and it would not resolve the immediate discomfort or risk of bladder damage.
*Neostigmine methylsulfate injection*
- Neostigmine is an **acetylcholinesterase inhibitor** that increases acetylcholine levels, potentially improving bladder contractility, but it is not typically the first-line treatment for acute postoperative urinary retention.
- Like bethanechol, it doesn't provide the rapid relief of bladder distension that catheterization does and is more often considered for chronic or neurogenic bladder dysfunction once acute retention is managed.
*Intravenous furosemide*
- Furosemide is a **loop diuretic** that increases urine production, which would exacerbate the problem in a patient with acute urinary retention.
- Increasing urine output without the ability to void would worsen bladder distension and patient discomfort, making it a contraindicated intervention.
*Intravenous neostigmine methylsulfate*
- While neostigmine can be given intravenously, its use in acute postoperative urinary retention is **not a primary treatment**.
- Its effect is slower than direct bladder drainage, and the immediate priority is to decompress the bladder to relieve symptoms and prevent complications.
Urethral injury management US Medical PG Question 4: One day after undergoing surgery for a traumatic right pelvic fracture, a 73-year-old man has pain over his buttocks and scrotum and urinary incontinence. Physical examination shows right-sided perineal hypesthesia and absence of anal sphincter contraction when the skin around the anus is touched. This patient is most likely to have which of the following additional neurological deficits?
- A. Impaired hip flexion
- B. Paralysis of hip adductors
- C. Absent cremasteric reflex
- D. Impaired psychogenic erection
- E. Absent reflex erection (Correct Answer)
Urethral injury management Explanation: ***Absent reflex erection***
- The patient's symptoms (buttock/scrotal pain, perineal hypesthesia, urinary incontinence, absent anal sphincter contraction) suggest **damage to the sacral plexus and pudendal nerve**, consistent with a **cauda equina syndrome**.
- **Reflex erections** are primarily mediated by the **sacral parasympathetic outflow (S2-S4)**, which are likely compromised given the other sacral nerve deficits.
*Impaired hip flexion*
- **Hip flexion** is primarily controlled by the **L1-L3 nerve roots** (e.g., iliopsoas muscle), and while a severe pelvic fracture could cause widespread nerve damage, the current symptoms localize more strongly to the sacral region.
- The described symptoms are more indicative of **sacral nerve involvement** rather than higher lumbar segments that govern hip flexion.
*Paralysis of hip adductors*
- **Hip adduction** is mainly innervated by the **obturator nerve (L2-L4)**.
- The patient's symptoms point to **S2-S4 nerve dysfunction** (perineal sensation, anal sphincter, bladder), which are distinct from the obturator nerve's primary innervations.
*Absent cremasteric reflex*
- The **cremasteric reflex** is mediated by the **genitofemoral nerve (L1-L2)**.
- The symptoms presented are more consistent with **sacral nerve damage**, specifically S2-S4, rather than the higher lumbar segments responsible for the cremasteric reflex.
*Impaired psychogenic erection*
- **Psychogenic erections** are initiated by **supraspinal input** descending through the thoracolumbar spinal cord (T10-L2) to activate sympathetic pathways.
- While sacral nerve damage can affect the final efferent pathway for all erections, the direct impairment of psychogenic initiation is linked to higher centers and **thoracolumbar sympathetic outflow**, not purely sacral damage.
Urethral injury management US Medical PG Question 5: A 40-year-old sailor is brought to a military treatment facility 20 minutes after being involved in a navy ship collision. He appears ill. He reports a sensation that he needs to urinate but is unable to void. His pulse is 140/min, respirations are 28/min, and blood pressure is 104/70 mm Hg. Pelvic examination shows ecchymoses over the scrotum and perineum. There is tenderness over the suprapubic region and blood at the urethral meatus. Digital rectal examination shows a high-riding prostate. Abdominal ultrasound shows a moderately distended bladder. X-rays of the pelvis show fractures of all four pubic rami. Which of the following is the most likely cause of this patient's symptoms?
- A. Tearing of the anterior urethra
- B. Rupture of the corpus cavernosum
- C. Tearing of the posterior urethra (Correct Answer)
- D. Tearing of the ureter
- E. Rupture of the bladder
Urethral injury management Explanation: ***Tearing of the posterior urethra***
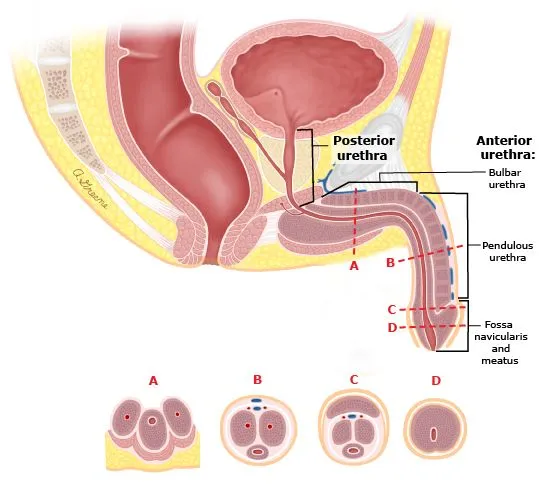
- The combination of **pelvic fractures**, **blood at the urethral meatus**, inability to void despite a sensation to do so, and a **high-riding prostate** are classic signs of posterior urethral injury.
- The posterior urethra, particularly the membranous portion, is vulnerable to shear forces and tearing during severe pelvic trauma.
*Tearing of the anterior urethra*
- Anterior urethral injuries are typically associated with a **straddle injury** or direct trauma to the perineum, not necessarily pelvic fractures.
- While blood at the meatus can occur, the **high-riding prostate** and extensive pelvic fractures point away from an isolated anterior injury.
*Rupture of the corpus cavernosum*
- This is usually a result of "penile fracture" during sexual intercourse and presents with sudden pain, detumescence, and a characteristic "eggplant" deformity, which are not described here.
- It does not explain the inability to void, high-riding prostate, or association with pelvic fractures.
*Tearing of the ureter*
- Ureteral injuries are typically associated with penetrating trauma or iatrogenic injury during surgery; they rarely occur with blunt pelvic trauma of this nature.
- Symptoms would include flank pain, hematuria, or urine leakage into the retroperitoneum, not significant urethral bleeding or a high-riding prostate.
*Rupture of the bladder*
- Bladder rupture can be intra- or extraperitoneal and is often associated with pelvic fractures. However, it typically causes gross hematuria and often free fluid in the peritoneum (intraperitoneal rupture) or extravasation into the space of Retzius (extraperitoneal rupture).
- While a distended bladder is noted, the presence of **blood at the urethral meatus** and a **high-riding prostate** strongly implicate urethral injury rather than primarily bladder rupture.
Urethral injury management US Medical PG Question 6: A 57-year-old woman comes to the physician because of several years of recurrent pelvic pain and constipation. She has increased fecal urgency and a sensation of incomplete evacuation following defecation. She has had no problems associated with urination. Her last menstrual period was 6 years ago. She has had three uncomplicated vaginal deliveries. Physical examination shows normal external genitalia. Speculum examination of the vagina and the cervix shows bulging of the posterior vaginal wall during Valsalva maneuver. Weakness of which of the following structures is the most likely cause of this patient's symptoms?
- A. Cardinal ligament
- B. Uterosacral ligament
- C. Bulbospongiosus muscle
- D. Pubocervical fascia
- E. Rectovaginal fascia (Correct Answer)
Urethral injury management Explanation: ***Rectovaginal fascia***
- The patient's symptoms of recurrent pelvic pain, constipation, increased fecal urgency, and incomplete evacuation, along with **posterior vaginal wall bulging** during Valsalva, are classic signs of a **rectocele**.
- A rectocele results from the weakening or tearing of the **rectovaginal fascia** (also known as the rectovaginal septum), which normally separates the rectum from the vagina and provides support.
*Cardinal ligament*
- The **cardinal ligament** (transverse cervical ligament) primarily provides support to the **cervix and uterus**, preventing uterine prolapse.
- While pelvic organ prolapse is possible, weakness of the cardinal ligament would typically manifest as **uterine prolapse** or anterior vaginal wall bulging (cystocele), not posterior vaginal bulging related to bowel symptoms.
*Uterosacral ligament*
- The **uterosacral ligaments** originate from the cervix and insert into the sacrum, primarily supporting the **uterus and upper vagina**.
- Weakness in these ligaments can contribute to **uterine prolapse** and some forms of vault prolapse after hysterectomy, which are not the primary issues described here.
*Bulbospongiosus muscle*
- The **bulbospongiosus muscle** is part of the superficial perineal pouch and surrounds the vaginal and urethral openings, contributing to **clitoral erection** and tightening the vaginal introitus.
- Weakness of this muscle is not directly associated with rectocele formation or the specific bowel symptoms reported by the patient.
*Pubocervical fascia*
- The **pubocervical fascia** supports the **bladder and urethra**, separating them from the vagina from the front.
- Weakness in this fascia leads to a **cystocele** (prolapse of the bladder into the vagina), which would typically cause urinary symptoms like stress incontinence, not bowel symptoms and posterior vaginal bulging.
Urethral injury management US Medical PG Question 7: A 67-year-old man is brought to the emergency room after being involved in a traffic accident. He currently complains of bilateral hip pain. His vital signs are within the normal range, and he is hemodynamically stable. The pelvic compression test is positive. External genitalia appears normal, except there is blood at the urethral meatus and a contusion at the base of the scrotum. Digital rectal examination (DRE) shows a high-riding ballotable prostate. An X-ray reveals the presence of a pelvic fracture. Which of the following initial actions is the most appropriate for this patient?
- A. Insert a Foley catheter
- B. Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine
- C. Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film (Correct Answer)
- D. Obtain a urinalysis to detect microscopic hematuria
- E. Perform a suprapubic cystostomy
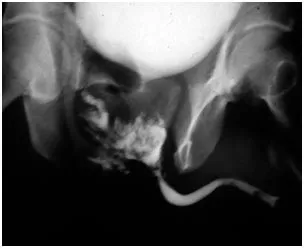
Urethral injury management Explanation: ***Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film***
- The combination of **blood at the urethral meatus**, a **high-riding ballotable prostate** on DRE, and a **pelvic fracture** are classic signs of a **urethral injury**, specifically a posterior urethral tear.
- A **retrograde urethrogram (RUG)** is the gold standard diagnostic test to confirm urethral injury and determine its location and extent, which is crucial before any attempt at catheterization.
*Insert a Foley catheter*
- **Insertion of a Foley catheter is contraindicated** in suspected urethral injuries, as it can worsen a partial tear into a complete transection or create a false passage.
- Doing so blindly could lead to further damage, stricture formation, and increased morbidity.
*Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine*
- This approach is premature before confirming the diagnosis and extent of urethral injury; **indigo carmine is used to assess ureteral integrity**, not urethral injury.
- Surgical exploration for urethral injury as an initial step is typically reserved for cases where RUG cannot be performed or for severe complex injuries with other indications for immediate surgery.
*Obtain a urinalysis to detect microscopic hematuria*
- While microscopic hematuria would likely be present, it is a **nonspecific finding** and does not provide information about the integrity of the urethra itself.
- It would not change the need for a RUG to assess for urethral injury in the presence of more specific signs.
*Perform a suprapubic cystostomy*
- A **suprapubic cystostomy** is the appropriate method for urinary diversion in a patient with a confirmed urethral injury if a Foley catheter cannot be safely placed.
- However, it is an intervention chosen *after* diagnosing the injury with a RUG, not the initial diagnostic step itself.
Urethral injury management US Medical PG Question 8: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Urethral injury management Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Urethral injury management US Medical PG Question 9: A 70-year-old man with metastatic castration-resistant prostate cancer presents to the emergency department with severe back pain, bilateral lower extremity weakness (3/5 strength), and urinary retention that started 8 hours ago. He has known bone metastases and his PSA has been rising despite androgen deprivation therapy. MRI spine shows an epidural mass at T10 with severe spinal cord compression and near-complete canal obliteration. He is neurologically intact above T10. Radiation oncology, neurosurgery, and medical oncology are consulted. Evaluate the optimal management approach.
- A. Corticosteroids, radiation therapy, and switch to next-line systemic therapy
- B. Stereotactic radiosurgery as single-modality treatment
- C. Emergent surgical decompression followed by radiation therapy (Correct Answer)
- D. Palliative care consultation and comfort measures only given metastatic disease
- E. High-dose corticosteroids and emergent radiation therapy alone
Urethral injury management Explanation: ***Emergent surgical decompression followed by radiation therapy***
- For patients with **malignant spinal cord compression (MSCC)** and acute neurologic deficits lasting <48 hours, **decompressive surgery** followed by radiotherapy results in better ambulatory outcomes than radiation alone.
- This patient has a **single level of compression** (T10) and a reasonable functional status above the lesion, making him an ideal candidate for surgery to preserve **quality of life**.
*Corticosteroids, radiation therapy, and switch to next-line systemic therapy*
- While **systemic therapy** is important for managing metastatic disease, it does not address the acute **mechanical compression** currently threatening spinal cord viability.
- Postponing definitive mechanical decompression in favor of systemic treatment would likely result in **permanent paraplegia** given the severe canal obliteration.
*Stereotactic radiosurgery as single-modality treatment*
- **Stereotactic radiosurgery (SRS)** is effective for spinal metastases but is generally not the primary choice when there is **high-grade spinal cord compression** with an associated neurologic deficit.
- Surgery is needed first to provide immediate **mechanical decompression** and create a "separation" distance between the cord and the tumor for safer high-dose radiation.
*Palliative care consultation and comfort measures only given metastatic disease*
- Although the cancer is metastatic, preserving **ambulatory function** and bladder control is a priority for maintaining dignity and independence.
- **MSCC** is an oncologic emergency where intervention is indicated unless the patient's **life expectancy** is very short (typically <3 months), which is not clearly the case here.
*High-dose corticosteroids and emergent radiation therapy alone*
- Radiation therapy alone is typically reserved for patients who are not **surgical candidates**, have multisegmental disease, or have complete paralysis for >48 hours.
- **Direct decompressive surgery** is superior for restoring and maintaining the ability to walk in patients with acute, unstable neurologic symptoms from a **single-level mass**.
Urethral injury management US Medical PG Question 10: A 3-year-old boy is brought to the clinic for evaluation of an undescended left testicle noted since birth. The right testicle is in normal scrotal position. On examination, the left testicle is palpable in the inguinal canal and can be manipulated to the upper scrotum but retracts immediately upon release. The testicle appears smaller than the contralateral side. The parents report they were told to wait and see if it descends spontaneously. What is the most appropriate management at this time?
- A. Immediate orchiopexy given the patient's age (Correct Answer)
- B. Reassurance and follow-up at age 5 years before school entry
- C. Continue observation as the testicle is palpable and may still descend
- D. Orchiectomy given the size discrepancy and malignancy risk
- E. Hormonal therapy with hCG to stimulate testicular descent
Urethral injury management Explanation: ***Immediate orchiopexy given the patient's age***
- Spontaneous descent is highly unlikely after **6 months of age**; surgery is recommended as early as possible after this window to improve **fertility** and facilitate **cancer screening**.
- This patient is **3 years old**, which is well past the recommended management window of **6 to 18 months**, necessitating prompt surgical intervention.
*Continue observation as the testicle is palpable and may still descend*
- Spontaneous descent of a cryptorchid testis rarely occurs after **age 6 months**, making ongoing observation clinically inappropriate.
- Delayed treatment increases the risk of **testicular atrophy**, **germ cell loss**, and potentially **malignant transformation**.
*Hormonal therapy with hCG to stimulate testicular descent*
- **Hormonal therapy** (e.g., hCG or GnRH) is generally not recommended in the US due to poor **long-term efficacy** compared to surgery.
- The success rate of hormonal therapy is notably low for truly **cryptorchid** testes and does not replace the gold standard of **orchiopexy**.
*Reassurance and follow-up at age 5 years before school entry*
- Waiting until age 5 is inappropriate as it significantly increases the risk of **infertility** and **testicular germ cell tumors**.
- The diagnosis of a **retractile testis** (which might be observed) is ruled out here because the testis **retracts immediately** and is smaller than the contralateral side.
*Orchiectomy given the size discrepancy and malignancy risk*
- **Orchiectomy** (removal) is generally reserved for **post-pubertal males** or instances where the testis is found to be **non-viable** or severely dysgenetic during surgery.
- In a **3-year-old**, the primary goal is **orchiopexy** to preserve hormonal function and provide a chance for future fertility.
More Urethral injury management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.