Renal cell carcinoma surgery US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal cell carcinoma surgery. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Renal cell carcinoma surgery US Medical PG Question 1: A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?
- A. Bladder trigone
- B. Uterine artery
- C. Kidney
- D. Ureter (Correct Answer)
Renal cell carcinoma surgery Explanation: ***Ureter***
- The **infundibulopelvic ligament** (also known as the suspensory ligament of the ovary) contains the **ovarian artery and vein** and is in close proximity to the ureter as it crosses the pelvic brim.
- During dissection or clamping of this ligament, especially in an emergency setting or when anatomy is distorted (e.g., by an enlarged ovary or edema), the **ureter** is highly susceptible to injury.
*Bladder trigone*
- The **bladder trigone** is the smooth triangular region at the base of the bladder, formed by the openings of the ureters and the internal urethral orifice.
- It is not directly adjacent to the infundibulopelvic ligament and is therefore at a comparably lower risk of injury during dissection of this ligament.
*Uterine artery*
- The **uterine artery** travels within the cardinal ligament and supplies the uterus; it is located more medially and inferiorly within the broad ligament.
- While important in pelvic surgery, it is not in the immediate vicinity of the infundibulopelvic ligament dissection itself.
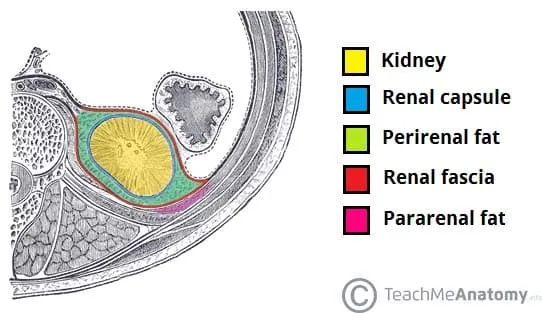
*Kidney*
- The **kidneys** are retroperitoneal organs located much higher in the abdominal cavity, far superior to the pelvis.
- They are not at risk of direct injury during pelvic surgery involving the infundibulopelvic ligament.
Renal cell carcinoma surgery US Medical PG Question 2: During the course of investigation of a suspected abdominal aortic aneurysm in a 57-year-old woman, a solid 6 × 5 cm mass is detected in the right kidney. The abdominal aorta reveals no abnormalities. The patient is feeling well and has no history of any serious illness or medication usage. She is a 25-pack-year smoker. Her vital signs are within normal limits. Physical examination reveals no abnormalities. Biopsy of the mass shows renal cell carcinoma. Contrast-enhanced CT scan indicates no abnormalities involving contralateral kidney, lymph nodes, lungs, liver, bone, or brain. Which of the following treatment options is the most appropriate next step in the management of this patient?
- A. Sunitinib
- B. Radiation
- C. Nephrectomy (Correct Answer)
- D. Interferon-ɑ (IFN-ɑ)
- E. Interleukin 2 (IL-2)
Renal cell carcinoma surgery Explanation: ***Nephrectomy***
- The patient has a **localized renal cell carcinoma (RCC)** without evidence of metastasis, as indicated by the CT scan showing no abnormalities in the contralateral kidney, lymph nodes, lungs, liver, bone, or brain.
- **Surgical removal** of the affected kidney (**nephrectomy**) is the **gold standard** and curative treatment for localized RCC.
*Sunitinib*
- **Sunitinib** is a **tyrosine kinase inhibitor** used for advanced or metastatic RCC, not for localized disease.
- It would be considered if the disease had spread beyond the kidney or if surgical resection was not feasible.
*Radiation*
- **Renal cell carcinoma** is generally considered **radioresistant**, making external beam radiation therapy ineffective as a primary treatment.
- Radiation is sometimes used for **palliative care** in metastatic RCC, for example, to relieve bone pain or brain metastases.
*Interferon-ɑ (IFN-ɑ)*
- **Interferon-ɑ** is an **immunotherapy** agent. Its use in RCC has largely been replaced by newer, more effective agents.
- It was historically used for metastatic RCC but is not indicated for localized disease and has significant side effects.
*Interleukin 2 (IL-2)*
- **High-dose interleukin 2 (IL-2)** is another **immunotherapy** agent effective in a subset of patients with metastatic RCC.
- It is not used for localized RCC and carries a risk of serious toxicity, requiring administration in specialized centers.
Renal cell carcinoma surgery US Medical PG Question 3: Eight hours after undergoing an open right hemicolectomy and a colostomy for colon cancer, a 52-year-old man has wet and bloody surgical dressings. He has had episodes of blood in his stools during the past 6 months, which led to the detection of colon cancer. He has hypertension and ischemic heart disease. His younger brother died of a bleeding disorder at the age of 16. The patient has smoked one pack of cigarettes daily for 36 years and drinks three to four beers daily. Prior to admission, his medications included aspirin, metoprolol, enalapril, and simvastatin. Aspirin was stopped 7 days prior to the scheduled surgery. He appears uncomfortable. His temperature is 36°C (96.8°F), pulse is 98/min, respirations are 14/min, and blood pressure is 118/72 mm Hg. Examination shows a soft abdomen with a 14-cm midline incision that has severe oozing of blood from its margins. The colostomy bag has some blood collected within. Laboratory studies show:
Hemoglobin 12.3 g/dL
Leukocyte count 11,200/mm3
Platelet count 210,000/mm3
Bleeding time 4 minutes
Prothrombin time 15 seconds (INR=1.1)
Activated partial thromboplastin time 36 seconds
Serum
Urea nitrogen 30 mg/dL
Glucose 96 mg/dL
Creatinine 1.1 mg/dL
AST 48 U/L
ALT 34 U/L
γ-Glutamyltransferase 70 U/L (N= 5–50 U/L)
Which of the following is the most likely cause of this patient's bleeding?
- A. Factor VIII deficiency
- B. Liver dysfunction
- C. Erosion of blood vessels
- D. Insufficient mechanical hemostasis (Correct Answer)
- E. Platelet dysfunction
Renal cell carcinoma surgery Explanation: ***Insufficient mechanical hemostasis***
- The patient's **coagulation studies are within normal limits** (normal PT, aPTT, bleeding time, and platelet count), ruling out most common intrinsic bleeding disorders.
- Given the timing (8 hours post-surgery) and the nature of bleeding (oozing from incision margins and colostomy site), **inadequate surgical closure or ligature** is the most probable cause.
*Factor VIII deficiency*
- This would present with a **prolonged activated partial thromboplastin time (aPTT)**, which is normal in this patient (36 seconds). His brother's death from a bleeding disorder is a red herring.
- Congenital factor deficiencies typically manifest earlier in life and cause more severe, spontaneous bleeding, not just post-operative oozing with normal coagulation factors.
*Liver dysfunction*
- Severe liver dysfunction would typically lead to **prolonged PT and aPTT** due to impaired synthesis of clotting factors.
- While the patient has elevated GGT, indicating some liver stress likely from alcohol, his AST and ALT are only mildly elevated, and his coagulation tests are normal.
*Erosion of blood vessels*
- This is less likely to cause widespread oozing and would typically present as a more significant, **pulsatile hemorrhage** or hematoma.
- While possible in a surgical field, the lack of significant hemodynamic compromise and normal coagulation points away from a major vessel erosion.
*Platelet dysfunction*
- This would typically result in a **prolonged bleeding time**, which is normal in this patient (4 minutes).
- Although the patient was on aspirin, it was stopped 7 days prior to surgery, which is typically sufficient for platelet function to recover.
Renal cell carcinoma surgery US Medical PG Question 4: A 59-year-old Caucasian man presents with a one-month history of left flank fullness and pain. The patient has stable angina, which is controlled with medications including atorvastatin, metoprolol, and aspirin. His vital signs are within normal limits. BMI is 32 kg/m2. Clinical examination reveals a 10 x 10-cm palpable mass in the left flank. Testicular examination indicates left varicocele. Laboratory parameters are as follows:
Urine
Blood 3+
WBC none
RBC 65/hpf without dysmorphic features
Abdominal CT scan confirms the presence of a large solid mass originating in the left kidney with impingement on the left renal vein. Based on the most likely diagnosis, which of the following is considered a risk factor in this patient?
- A. Obesity (Correct Answer)
- B. Varicocele
- C. Atorvastatin
- D. Lynch syndrome
- E. Caucasian race
Renal cell carcinoma surgery Explanation: ***Obesity***
- This patient's **BMI of 32 kg/m2** indicates **obesity**, which is a well-established risk factor for **renal cell carcinoma (RCC)**, the most likely diagnosis given the clinical presentation (flank mass, hematuria, varicocele, and CT findings).
- Obesity is thought to increase RCC risk due to associated hormonal changes, such as increased **estrogen** and **insulin-like growth factor 1 (IGF-1)**, and chronic inflammation.
*Varicocele*
- While a **left varicocele** is a clinical finding often associated with **renal cell carcinoma**, particularly on the left side due to impingement on the left renal vein, it is a **symptom/sign** of the disease, not a risk factor for its development.
- The varicocele develops because the tumor obstructs the **left renal vein**, leading to retrograde flow and dilation of the **gonadal vein**.
*Atorvastatin*
- **Atorvastatin**, a statin used to treat hyperlipidemia and prevent cardiovascular disease, has **no known association** with an increased risk of renal cell carcinoma.
- Some studies even suggest a potential **protective effect** of statins against certain cancers, but this is not definitively established for RCC, and certainly not a risk factor.
*Lynch syndrome*
- **Lynch syndrome** (hereditary nonpolyposis colorectal cancer) is primarily associated with an increased risk of **colorectal cancer**, **endometrial cancer**, and other gastrointestinal/genitourinary cancers, but **not renal cell carcinoma**.
- Renal cell carcinoma is more commonly linked to other genetic syndromes like **Von Hippel-Lindau disease** or **hereditary papillary renal carcinoma**.
*Caucasian race*
- While there are some **racial disparities** in certain cancer incidences, the **Caucasian race itself is not considered a primary modifiable risk factor** for renal cell carcinoma.
- **African Americans** may have a slightly higher risk for RCC, but this is often attributed to socioeconomic factors and comorbidities rather than race as an independent biological risk factor.
Renal cell carcinoma surgery US Medical PG Question 5: A 57-year-old man presents with acute-onset nausea and left flank pain. He says his symptoms suddenly started 10 hours ago and have not improved. He describes the pain as severe, colicky, intermittent, and localized to the left flank. The patient denies any fever, chills, or dysuria. His past medical history is significant for nephrolithiasis, incidentally diagnosed 10 months ago on a routine ultrasound, for which he has not been treated. His family history is unremarkable. The patient is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. Severe left costovertebral angle tenderness is noted. Gross hematuria is present on urinalysis. A non-contrast CT of the abdomen and pelvis reveals a 12-mm obstructing calculus at the left ureterovesical junction. Initial management, consisting of IV fluid resuscitation, antiemetics, and analgesia, is administered. Which of the following is the best next step in the management of this patient?
- A. Percutaneous nephrostomy
- B. Percutaneous nephrostolithotomy (PCNL)
- C. Extracorporeal shockwave lithotripsy (ESWL)
- D. 24-hour urine chemistry
- E. Ureteroscopy (Correct Answer)
Renal cell carcinoma surgery Explanation: ***Ureteroscopy***
- Ureteroscopy is the preferred treatment for **prompt stone removal** in patients with a large **ureteral calculus** (e.g., 12 mm) causing obstruction and intractable symptoms, especially when located in the **distal ureter** near the ureterovesical junction.
- This procedure allows for direct visualization of the stone, fragmentation using a **laser**, and removal with a basket, providing immediate relief and preventing potential complications like **hydronephrosis** or infection.
*Percutaneous nephrostomy*
- This procedure is typically reserved for cases where there is **urosepsis** or severe **hydronephrosis** requiring urgent decompression, which is not indicated here as the patient is afebrile and hemodynamically stable.
- While it provides drainage, it does not directly remove the stone and is less definitive for a distal ureteral stone.
*Percutaneous nephrostolithotomy (PCNL)*
- **PCNL** is primarily used for **large kidney stones** (> 2 cm) or complex renal calculi, not for ureteral stones.
- It involves accessing the kidney directly through the skin to remove stones, which is an overly invasive approach for a stone located at the ureterovesical junction.
*Extracorporeal shockwave lithotripsy (ESWL)*
- **ESWL** is less effective for large, **distal ureteral stones**, as the success rate for stones greater than 10 mm and those located distally is lower.
- While it is non-invasive, ureteroscopy offers a higher success rate for immediate clearance in this specific clinical scenario.
*24-hour urine chemistry*
- This is a diagnostic study performed to evaluate the **metabolic causes of stone formation** and to guide preventive strategies.
- It is an important step in preventing future stone recurrence but is not an immediate management step for an acute, obstructing ureteral stone.
Renal cell carcinoma surgery US Medical PG Question 6: A 49-year-old man presents to your clinic with “low back pain”. When asked to point to the area that bothers him the most, he motions to both his left and right flank. He describes the pain as deep, dull, and aching for the past few months. His pain does not change significantly with movement or lifting heavy objects. He noted dark colored urine this morning. He has a history of hypertension managed with hydrochlorothiazide; however, he avoids seeing the doctor whenever possible. He drinks 3-4 beers on the weekends but does not smoke. His father died of a sudden onset brain bleed, and his mother has diabetes. In clinic, his temperature is 99°F (37.2°C), blood pressure is 150/110 mmHg, pulse is 95/min, and respirations are 12/min. Bilateral irregular masses are noted on deep palpation of the abdomen. The patient has full range of motion in his back and has no tenderness of the spine or paraspinal muscles. Urine dipstick in clinic is notable for 3+ blood. Which chromosome is most likely affected by a mutation in this patient?
- A. Chromosome 6
- B. Chromosome 7
- C. Chromosome 4
- D. Chromosome 15
- E. Chromosome 16 (Correct Answer)
Renal cell carcinoma surgery Explanation: ***Chromosome 16***
- This patient's presentation with bilateral flank pain, hypertension, hematuria (dark urine with 3+ blood on dipstick), and palpable bilateral irregular abdominal masses is highly suggestive of **Autosomal Dominant Polycystic Kidney Disease (ADPKD)**.
- The most common form of ADPKD, comprising about 85% of cases, is caused by mutations in the **PKD1 gene** located on **chromosome 16**.
*Chromosome 6*
- Mutations on chromosome 6 are associated with conditions such as **hemochromatosis (HFE gene)** and certain types of **human leukocyte antigen (HLA) linked diseases**, neither of which fits the patient's primary symptoms.
- There is no direct link between chromosome 6 mutations and the classic presentation of ADPKD.
*Chromosome 7*
- Mutations on chromosome 7 are linked to conditions like **Cystic Fibrosis (CFTR gene)** and **Williams-Beuren Syndrome**.
- While CFTR mutations can cause renal cysts in some atypical cases, it does not typically present with the extensive renal manifestations and palpable masses seen in ADPKD.
*Chromosome 4*
- Chromosome 4 harbors the **PKD2 gene**, which is responsible for approximately 15% of ADPKD cases (ADPKD type 2).
- While PKD2 mutations can cause ADPKD, they generally present with a milder phenotype and later onset compared to PKD1 mutations. Given this patient's classic presentation with significant bilateral masses and relatively younger age, PKD1 (chromosome 16) is more likely.
- Chromosome 4 is also associated with **Huntington's disease**.
*Chromosome 15*
- Mutations on chromosome 15 are linked to conditions such as **Marfan syndrome** and **Prader-Willi/Angelman syndromes**.
- These conditions have distinct clinical features that do not align with the patient's symptoms of significant renal pathology.
Renal cell carcinoma surgery US Medical PG Question 7: A 61-year-old man comes to the physician because of several episodes of dark urine over the past 2 weeks. He does not have dysuria or flank pain. He works in a factory that produces dyes. Since an accident at work 5 years ago, he has had moderate hearing loss bilaterally. He takes no medications. He has smoked a pack of cigarettes daily for 29 years and drinks one alcoholic beverage daily. Vital signs are within normal limits. Physical examination shows no abnormalities. His urine is pink; urinalysis shows 80 RBC/hpf but no WBCs. Cystoscopy shows a 3-cm mass in the bladder mucosa. The mass is resected. Pathologic examination shows an urothelial carcinoma with penetration into the muscular layer. An x-ray of the chest and a CT scan of the abdomen and pelvis with contrast show a normal upper urinary tract and normal lymph nodes. Which of the following is the most appropriate next step in management?
- A. Palliative polychemotherapy
- B. Transurethral resection of tumor with intravesical BCG instillation
- C. Radical cystectomy (Correct Answer)
- D. Transurethral resection of tumor with intravesical chemotherapy
- E. Radiation therapy
Renal cell carcinoma surgery Explanation: ***Radical cystectomy***
- The patient has an **urothelial carcinoma** that has **penetrated the muscular layer**. This indicates an **invasive bladder cancer (T2 or greater)**, for which radical cystectomy is the standard of care to achieve cure.
- While imaging showed no distant metastasis, the deep invasion into the muscle requires aggressive surgical removal of the bladder, prostate (in men), and seminal vesicles, along with pelvic lymph node dissection.
*Palliative polychemotherapy*
- This option is typically reserved for patients with widespread **metastatic disease** or those who are not surgical candidates, which is not the case here.
- The patient's initial workup shows no evidence of distant metastasis, making a curative approach like surgery more appropriate.
*Transurethral resection of tumor with intravesical BCG instillation*
- This approach, often used for **high-grade non-muscle invasive bladder cancer**, is insufficient for muscle-invasive disease.
- **BCG instillation** aims to prevent recurrence and progression in superficial disease but cannot eradicate cancer that has invaded the muscularis propria.
*Transurethral resection of tumor with intravesical chemotherapy*
- Similar to BCG, **intravesical chemotherapy** is primarily effective for **non-muscle invasive bladder cancer** to prevent recurrence or treat carcinoma in situ.
- It does not provide adequate treatment for cancer that has invaded the detrusor muscle, as systemic or deeper treatments are required.
*Radiation therapy*
- While radiation therapy can be considered for bladder cancer, it is typically used in specific situations, such as for patients who are **not surgical candidates** or as part of a **bladder-sparing trimodality therapy** (TURBT, chemotherapy, and radiation) for highly selected patients.
- For muscle-invasive disease without clear contraindications for surgery, **radical cystectomy** offers better long-term survival rates.
Renal cell carcinoma surgery US Medical PG Question 8: A 24-year-old African American college student comes to the office for a scheduled visit. He has been healthy, although he reports occasional flank discomfort which comes and goes. He denies any fever, chills, dysuria, or polyuria in the past year. His vaccinations are up to date. His family history is unknown, as he was adopted. He smokes 1 pack of cigarettes every 3 days, drinks socially, and denies any current illicit drug use, although he endorses a history of injection drug use. He currently works as a waiter to afford his college tuition. His physical examination shows a young man with a lean build, normal heart sounds, clear breath sounds, bowel sounds within normal limits, and no lower extremity edema. You order a urinalysis which shows 8 red blood cells (RBCs) per high-power field (HPF). The test is repeated several weeks later and shows 6 RBCs/HPF. What is the most appropriate next step in management?
- A. Plain abdominal X-ray
- B. Repeat urinalysis in 6 months
- C. 24-hour urine collection test
- D. Renal ultrasound (Correct Answer)
- E. Observation
Renal cell carcinoma surgery Explanation: ***Renal ultrasound***
- This patient has **asymptomatic microscopic hematuria** which requires investigation to rule out significant renal or urological pathology, particularly in the context of recurrent flank discomfort and a history of injection drug use which increases risk for certain renal diseases.
- A **renal ultrasound** is the most appropriate initial imaging study to evaluate the kidneys and urinary tract for structural abnormalities, stones, masses, or hydronephrosis.
*Plain abdominal X-ray*
- A plain abdominal X-ray (KUB) is **less sensitive** than ultrasound for detecting many renal pathologies, especially soft tissue masses or early hydronephrosis.
- While it can detect **radio-opaque stones**, it will miss radiolucent stones and other important causes of hematuria.
*Repeat urinalysis in 6 months*
- This approach is too delayed given the **persistent microscopic hematuria** and the patient's reported flank discomfort, which warrants a more immediate workup.
- Delaying investigation could lead to the **progression of underlying pathology** that might be treatable if caught earlier.
*24-hour urine collection test*
- A 24-hour urine collection is useful for assessing **proteinuria** and **creatinine clearance**, and sometimes for quantification of red blood cell excretion, but it is not the initial diagnostic step for identifying the *source* or *cause* of hematuria.
- It would typically be considered **after initial imaging** and further characterization of the hematuria have been performed.
*Observation*
- **Observation alone is insufficient** for unexplained, persistent microscopic hematuria combined with flank discomfort, even if intermittent.
- This approach risks missing a potentially serious underlying condition that could benefit from early diagnosis and intervention, such as **renal cell carcinoma** or significant **nephrolithiasis**.
Renal cell carcinoma surgery US Medical PG Question 9: A 32-year-old man visits his family physician for 10 months of persistent left flank pain, weight loss, and fatigue. Also, he has had hematuria a couple of times in the last month. His mother was diagnosed and treated for a pheochromocytoma when she was 36 years old, and his father died at 45 years due to myocardial infarction. His personal medical history is not relevant. He does not smoke and used to be a varsity athlete in high school and university. Physical examination shows temporal wasting, pale mucous membranes and palms, a palpable mass in the left flank, and a varicocele that does not reduce upon recumbency. His family physician sends the patient to the emergency department for an abdominal computed tomography (CT) scan, which shows a complex left renal mass and a hemangioblastoma in T10. A biopsy of the renal mass is ordered by the oncology team, which demonstrates compact cells with prominent nucleoli, eosinophilic cytoplasm within a network of a small and thin-walled vasculature. What is the most likely type of tumor in this patient?
- A. Collecting duct carcinoma
- B. Clear-cell carcinoma (Correct Answer)
- C. Oncocytic carcinoma
- D. Papillary carcinoma
- E. Chromophobe carcinoma
Renal cell carcinoma surgery Explanation: ***Clear-cell carcinoma***
- This patient's presentation with a **renal mass**, hemangioblastoma, a family history of **pheochromocytoma** (his mother), and an early death of his father (likely from heart disease associated with pheochromocytoma) is highly suggestive of **Von Hippel-Lindau (VHL) syndrome**. **Clear cell renal cell carcinoma** is the most common renal tumor associated with VHL syndrome.
- The biopsy description of **compact cells with prominent nucleoli**, **eosinophilic cytoplasm**, and a **network of small and thin-walled vasculature** is characteristic of clear cell renal cell carcinoma.
*Collecting duct carcinoma*
- This is a rare and aggressive subtype of **renal cell carcinoma** that typically presents with a mass in the renal medulla, often with central necrosis.
- Its histological features involve atypical cells arranged in **tubules or ducts**, which does not match the description of compact cells with eosinophilic cytoplasm.
*Oncocytic carcinoma*
- **Oncocytic carcinoma** is a rare and generally benign tumor. It is characterized histologically by cells with abundant, granular eosinophilic cytoplasm.
- While it has eosinophilic cytoplasm, it lacks the prominent nucleoli and compact cell arrangement seen in the biopsy, and it is not typically associated with VHL syndrome.
*Papillary carcinoma*
- **Papillary carcinoma** is characterized by cells arranged in papillary formations or tubular structures. It is generally associated with different genetic syndromes (e.g., hereditary papillary renal carcinoma).
- The histological description provided, particularly the "compact cells" and vasculature, does not fit the typical papillary architecture.
*Chromophobe carcinoma*
- **Chromophobe carcinoma** is characterized by large cells with distinct cell borders and pale, flocculent cytoplasm. It typically has a good prognosis.
- This type of carcinoma is generally not associated with VHL syndrome and its histological features do not align with the biopsy description of compact cells with eosinophilic cytoplasm and prominent nucleoli.
Renal cell carcinoma surgery US Medical PG Question 10: Three hours after undergoing open proctocolectomy for ulcerative colitis, a 42-year-old male complains of abdominal pain. The pain is localized to the periumbilical and hypogastric regions. A total of 20 mL of urine has drained from his urinary catheter since the end of the procedure. Temperature is 37.2°C (98.9°F), pulse is 92/min, respirations are 12/min, and blood pressure is 110/72 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Physical examination shows a 20 cm vertical midline incision and an ileostomy in the right lower quadrant. There is no fluid drainage from the surgical wounds. The urinary catheter flushes easily and is without obstruction. Cardiopulmonary examination shows no abnormalities. Serum studies show a blood urea nitrogen of 30 mg/dL and a creatinine of 1.3 mg/dL. Which of the following is the most appropriate next step in management?
- A. Administer tamsulosin
- B. Administer intravenous furosemide
- C. Obtain an abdominal CT
- D. Start ciprofloxacin
- E. Administer intravenous fluids (Correct Answer)
Renal cell carcinoma surgery Explanation: ***Administer intravenous fluids***
- The patient's **oliguria** (20 mL urine over 3 hours, ~7 mL/hour) post-surgery, elevated **BUN (30 mg/dL)**, and **creatinine (1.3 mg/dL)** with a **BUN:Cr ratio >20:1** suggest **prerenal acute kidney injury** due to **hypovolemia**.
- Post-operative fluid losses from **third-spacing**, blood loss, and insensible losses commonly cause hypovolemia after major abdominal surgery.
- **Intravenous fluids** are the most appropriate initial step to restore intravascular volume and improve renal perfusion.
*Administer tamsulosin*
- **Tamsulosin** is an alpha-blocker used to relax smooth muscle in the prostate and bladder neck, primarily for **urinary retention** due to benign prostatic hyperplasia.
- This patient's oliguria is due to **prerenal azotemia** from hypovolemia, not prostatic obstruction, and the catheter flushes easily without obstruction.
*Administer intravenous furosemide*
- **Furosemide** is a loop diuretic that increases urine output, but administering it in the context of **prerenal acute kidney injury** can worsen hypovolemia and further compromise renal function.
- Diuretics are generally contraindicated in oliguria due to hypovolemia and should only be considered after volume resuscitation.
*Obtain an abdominal CT*
- While an abdominal CT can diagnose surgical complications, there are no immediate signs of a surgical emergency like **anastomotic leak** or **bowel obstruction**.
- Addressing the likely **hypovolemia** is more urgent and should precede further imaging in this scenario.
*Start ciprofloxacin*
- The patient does not show signs of infection, such as fever or localized signs of bacterial peritonitis, making **antibiotics** like ciprofloxacin inappropriate as the initial management step.
- The elevated BUN and creatinine are more indicative of volume depletion than infection.
More Renal cell carcinoma surgery US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.