Male infertility surgical procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Male infertility surgical procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Male infertility surgical procedures US Medical PG Question 1: A 7-month-old boy is brought to the physician for a well-child examination. He was born at 36 weeks' gestation and has been healthy since. He is at the 60th percentile for length and weight. Vital signs are within normal limits. The abdomen is soft and nontender. The external genitalia appear normal. Examination shows a single palpable testicle in the right hemiscrotum. The scrotum is nontender and not enlarged. There is a palpable mass in the left inguinal canal. Which of the following is the most appropriate next best step in management?
- A. Orchidopexy (Correct Answer)
- B. Gonadotropin therapy
- C. Exploration under anesthesia
- D. Reassurance
- E. Serum testosterone level
Male infertility surgical procedures Explanation: ***Orchidopexy***
- Since the testicle is **palpable in the inguinal canal** at 7 months, it is unlikely to spontaneously descend, making **orchidopexy** the definitive surgical treatment.
- Recommended by 6-12 months of age to prevent complications such as **infertility** and increased risk of **testicular cancer**.
*Gonadotropin therapy*
- **Gonadotropin therapy** is rarely used and has limited efficacy for **cryptorchidism**, especially for palpable undescended testes.
- It's typically reserved for specific cases and has a lower success rate compared to surgery.
*Exploration under anesthesia*
- While exploration is part of any surgical correction for an undescended testicle, **orchidopexy** specifically describes the complete procedure of bringing the testicle into the scrotum and fixing it there.
- **Exploration under anesthesia** alone is not a complete management step; it precedes the definitive repair.
*Reassurance*
- An undescended testicle at 7 months of age is unlikely to descend spontaneously and carries risks if left untreated, so **reassurance** is inappropriate.
- Intervention is necessary to prevent potential long-term complications.
*Serum testosterone level*
- **Serum testosterone level** evaluation is typically reserved for cases of **bilateral non-palpable testes** to assess for anorchia or other endocrine disorders.
- In a case with a palpable inguinal testicle and a normal contralateral testicle, it is not the next best step.
Male infertility surgical procedures US Medical PG Question 2: A 6-month-old boy is brought to the physician because of a right-sided scrotal swelling for the past 2 months. The swelling is intermittent and appears usually after the patient has been taken outdoors in a baby carrier, and disappears the next morning. The patient was born at term without complications and has been healthy. Examination shows a 3-cm, soft, nontender, and fluctuant right scrotal mass that is reducible and does not extend into the inguinal area. A light held behind the scrotum shines through. There are no bowel sounds in the mass. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in the management of this patient?
- A. Reassurance and follow-up (Correct Answer)
- B. Percutaneous drainage
- C. Ligation of the patent processus vaginalis
- D. Bilateral orchidopexy
- E. Surgical excision of the mass
Male infertility surgical procedures Explanation: ***Reassurance and follow-up***
- The presentation of an **intermittent, reducible, transilluminating scrotal swelling** in an infant, particularly one that resolves with rest, is characteristic of a **communicating hydrocele**.
- Most communicating hydroceles in infants resolve spontaneously by **12-18 months of age** as the **processus vaginalis** closes, so watchful waiting is the most appropriate initial management.
*Percutaneous drainage*
- This procedure is generally not recommended for communicating hydroceles due to the **risk of infection**, recurrence, and injury to scrotal structures.
- It does not address the underlying issue of the patent processus vaginalis, making it an ineffective long-term solution.
*Ligation of the patent processus vaginalis*
- This is the surgical treatment for a communicating hydrocele, but it is typically reserved for cases that **persist beyond 12-18 months of age** or those that cause complications.
- Given the patient's age (6 months) and the benign nature of the swelling, immediate surgical intervention is not indicated.
*Bilateral orchidopexy*
- **Orchidopexy** (surgical repositioning of a testis) is performed for **undescended testes**, which is not indicated by the patient's presentation.
- This patient has a scrotal swelling, and the testes are presumed to be in their normal position.
*Surgical excision of the mass*
- This is an overly aggressive and inappropriate intervention for a suspected communicating hydrocele.
- The mass is fluid-filled and caused by a patent processus vaginalis, not a solid tumor requiring excision.
Male infertility surgical procedures US Medical PG Question 3: At postpartum physical examination, a newborn is found to have male external genitalia. Scrotal examination shows a single palpable testicle in the right hemiscrotum. Ultrasound of the abdomen and pelvis shows an undescended left testis, seminal vesicles, uterus, and fallopian tubes. Chromosomal analysis shows a 46, XY karyotype. Which of the following sets of changes is most likely to be found in this newborn?
Legend: Normal = normal levels, ↑ = increased levels, ↓ = decreased levels
SRY-gene activity | Müllerian inhibitory factor (MIF) | Testosterone | Dihydrotestosterone (DHT)
- A. Normal normal normal ↓
- B. ↓ ↓ ↓ ↓
- C. Normal ↓ normal normal (Correct Answer)
- D. ↓ ↓ normal normal
- E. Normal normal ↑ ↑
Male infertility surgical procedures Explanation: ***Normal ↓ Normal Normal***
- A 46, XY karyotype with male external genitalia indicates **normal SRY-gene activity** and normal **testosterone** production, as these are critical for male sexual differentiation.
- The presence of a **uterus and fallopian tubes** in a 46, XY individual is characteristic of persistent **Müllerian duct syndrome**, caused by a **deficiency or insensitivity to Müllerian Inhibiting Factor (MIF)**, leading to a decreased level of MIF.
*Normal Normal Normal ↓*
- This pattern would suggest normal initial male differentiation but an issue downstream, possibly with **5-alpha-reductase deficiency** (leading to decreased DHT) and normal MIF, which would prevent Müllerian structure development.
- The presence of a **uterus and fallopian tubes** contradicts normal MIF levels.
*↓ ↓ ↓ ↓*
- This combination indicates severe defects in all aspects of male sexual development, which would lead to **female external genitalia** or ambiguous genitalia, not male external genitalia.
- Such low levels would also prevent the formation of a palpable testis, and a 46, XY karyotype with female internal structures due to low testosterone and MIF would be highly unlikely to produce male external genitalia.
*↓ ↓ Normal Normal*
- While low MIF would explain the presence of a uterus and fallopian tubes, a **decreased SRY-gene activity** would prevent the development of testes and lead to ambiguous or female external genitalia, rather than male external genitalia.
- Normal testosterone and DHT with decreased SRY gene activity is a contradictory combination, as testosterone production is dependent on the presence of testes.
*Normal Normal ↑ ↑*
- This profile would result in normal male internal and external genitalia, without the presence of **uterus or fallopian tubes**.
- Increased levels of androgens are typically found in conditions like **congenital adrenal hyperplasia** in XX individuals, leading to virilization, but are not consistent with the internal structures seen here.
Male infertility surgical procedures US Medical PG Question 4: After a year of trying to conceive, a young couple in their early twenties decided to try in vitro fertilization. During preliminary testing of fertility, it was found that the male partner had dysfunctional sperm. Past medical history revealed that he had frequent sinus and lung infections throughout his life. The physician noted an abnormal exam finding on palpation of the right fifth intercostal space at the midclavicular line. What would be the most likely diagnosis responsible for this patient's infertility?
- A. Chédiak-Higashi syndrome
- B. Kartagener syndrome (Correct Answer)
- C. Adenosine deaminase deficiency
- D. Williams syndrome
- E. Cystic fibrosis
Male infertility surgical procedures Explanation: ***Kartagener syndrome***
- This syndrome is a subgroup of **primary ciliary dyskinesia** characterized by the triad of **situs inversus**, **chronic sinusitis**, and **bronchiectasis**. The abnormal exam finding on palpation of the right fifth intercostal space at the midclavicular line suggests the apex beat is on the right side, indicating **dextrocardia** (situs inversus) which supports this diagnosis.
- The **dysfunctional sperm** and **frequent respiratory infections** are also classic features, resulting from immotile cilia in the respiratory tract and immotile flagella in sperm.
*Chédiak-Higashi syndrome*
- This is a rare autosomal recessive disorder characterized by **immunodeficiency**, **partial oculocutaneous albinism**, and **peripheral neuropathy**.
- While patients suffer from recurrent infections due to impaired phagolysosome formation, it does not typically cause situs inversus or male infertility due to dysfunctional sperm.
*Adenosine deaminase deficiency*
- This is a severe form of **severe combined immunodeficiency (SCID)**, leading to a profound deficiency of T and B lymphocytes.
- Patients typically present with **recurrent opportunistic infections** and failure to thrive early in life, but it does not cause situs inversus or issues with sperm motility.
*Williams syndrome*
- This is a genetic condition characterized by specific **facial features** (e.g., "elfin" facies), **cardiovascular problems** (especially supravalvular aortic stenosis), unique **cognitive profiles**, and **overly friendly personalities**.
- It does not involve recurrent respiratory infections, situs inversus, or male infertility.
*Cystic fibrosis*
- This genetic disorder primarily affects the **lungs**, **pancreas**, liver, and intestines, causing the production of thick, sticky mucus.
- While it causes **recurrent lung infections** and **male infertility** (due to congenital bilateral absence of the vas deferens, not immotile sperm), it does not cause situs inversus.
Male infertility surgical procedures US Medical PG Question 5: A 38-year-old woman presents to her primary care physician concerned about her inability to get pregnant for the past year. She has regular menstrual cycles and has unprotected intercourse with her husband daily. She is an immigrant from Australia and her past medical history is not known. She is currently taking folic acid and multivitamins. The patient's husband has had a sperm count that was determined to be within the normal range twice. She is very concerned about her lack of pregnancy and that she is too old. Which of the following is the most appropriate next step in management for this patient?
- A. Repeat semen count
- B. Assess ovulation with an ovulation calendar
- C. Perform hysterosalpingogram (Correct Answer)
- D. Advise against pregnancy given the patient's age
- E. Continue regular intercourse for 1 year
Male infertility surgical procedures Explanation: ***Perform hysterosalpingogram***
- Given the patient’s age and duration of infertility (1 year at age 38, typically evaluation starts earlier for those over 35), assessing **tubal patency** with a **hysterosalpingogram (HSG)** is an essential step in the infertility workup.
- HSG can identify structural abnormalities like **blocked fallopian tubes** or **uterine anomalies**, which are common causes of infertility.
*Repeat semen count*
- The husband has already had **two normal semen analyses**, making further repeated testing at this stage less likely to yield new information or be the most appropriate next step.
- While male factor infertility is common, it has been reasonably excluded here, shifting the focus to female factors.
*Assess ovulation with an ovulation calendar*
- The patient reports having **regular menstrual cycles**, which strongly suggests she is **ovulating regularly**.
- Ovulation calendars are often used to identify the fertile window but are less useful for confirming ovulation in someone with regular cycles when investigating infertility causes.
*Advise against pregnancy given the patient's age*
- While **fertility declines with age**, advising against pregnancy is inappropriate and **premature** without a proper infertility workup.
- Many women in their late 30s and early 40s successfully conceive with appropriate management and intervention.
*Continue regular intercourse for 1 year*
- For women aged 35 or older, an infertility evaluation is typically initiated after **6 months of unprotected intercourse** without conception.
- The patient is 38 and has been trying for a year, so further delay is not recommended; an immediate workup is warranted.
Male infertility surgical procedures US Medical PG Question 6: A father brings his 1-year-old son into the pediatrician's office for a routine appointment. He states that his son is well but mentions that he has noticed an intermittent bulge on the right side of his son's groin whenever he cries or strains for bowel movement. Physical exam is unremarkable. The physician suspects a condition that may be caused by incomplete obliteration of the processus vaginalis. Which condition is caused by the same defective process?
- A. Diaphragmatic hernia
- B. Femoral hernia
- C. Testicular torsion
- D. Hydrocele (Correct Answer)
- E. Varicocele
Male infertility surgical procedures Explanation: ***Hydrocele***
- The patient's symptoms (intermittent groin bulge with crying/straining) are classic for an **indirect inguinal hernia**, which, like a hydrocele, results from an **incompletely obliterated processus vaginalis**.
- A **hydrocele** involves the accumulation of **serous fluid** within the persistent processus vaginalis, as opposed to abdominal contents in a hernia.
*Diaphragmatic hernia*
- This condition involves the protrusion of abdominal contents into the chest cavity through a defect in the **diaphragm**.
- It is unrelated to the obliteration of the processus vaginalis but rather to **diaphragmatic development**.
*Femoral hernia*
- A femoral hernia involves protrusion through the **femoral canal**, inferior to the inguinal ligament.
- It does not involve the processus vaginalis and is more common in **multiparous women**.
*Testicular torsion*
- This condition is a surgical emergency caused by the **twisting of the spermatic cord**, compromising blood supply to the testis.
- It is not related to the processus vaginalis but often involves an inadequately fixed testis (bell-clapper deformity).
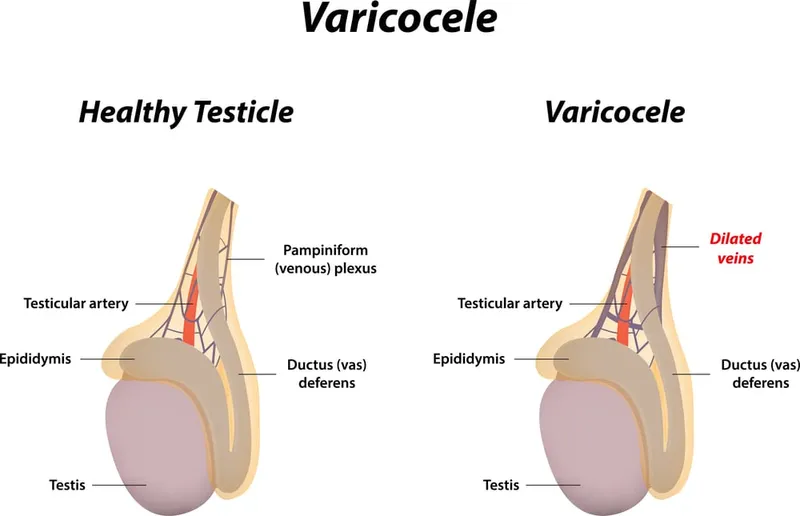
*Varicocele*
- A varicocele is an abnormal dilation of the **pampiniform venous plexus** within the spermatic cord.
- It is caused by incompetent valves in the testicular veins and not by a patent processus vaginalis.
Male infertility surgical procedures US Medical PG Question 7: A 32-year-old man and his wife are sent to a fertility specialist after trying to conceive for several years without success. They have had unprotected sex several times a week. He has no history of a serious illness and does not take any medications. There are no concerns about his libido or erections. His female partner is not on contraceptive medication and has a child from a previous marriage. At the clinic, his vitals are normal. Examination of the scrotum on the right side is normal, but on the left side there are many deep and superficial ducts or vessels that feels like a bag of worms on palpation. The lesion is more apparent when the patient bears down. Semen analysis shows a low sperm count with poor motility and an increased percentage of abnormal sperms. Which of the following is the most appropriate next step in management?
- A. Pulsatile GNRH
- B. Ligation of processus vaginalis
- C. Microsurgical varicocelectomy (Correct Answer)
- D. No therapy at this time
- E. Intracytoplasmic sperm injection
Male infertility surgical procedures Explanation: ***Microsurgical varicocelectomy***
- The clinical presentation of a "bag of worms" on scrotal palpation that becomes more apparent with bearing down is classic for a **varicocele**.
- A varicocele is a common cause of **male infertility** due to impaired spermatogenesis, often leading to low sperm count, poor motility, and abnormal sperm morphology, which are all present in this patient's semen analysis. **Microsurgical varicocelectomy** is the most appropriate next step to improve semen parameters and increase the chances of natural conception.
*Pulsatile GNRH*
- **Pulsatile GnRH** is used to treat **hypogonadotropic hypogonadism**, a condition characterized by low testosterone and low FSH/LH, which is not suggested by the clinical picture or symptoms here.
- This patient's libido and erections are normal, indicating adequate testosterone levels, making pulsatile GnRH an unlikely treatment.
*Ligation of processus vaginalis*
- **Ligation of the processus vaginalis** is a surgical procedure primarily used to treat a **patent processus vaginalis**, which can cause a **communicating hydrocele** or an **indirect inguinal hernia**.
- This procedure is not indicated for the management of varicocele or male infertility directly related to sperm production issues.
*No therapy at this time*
- The patient has been trying to conceive for several years, has a clear diagnosis of varicocele, and significant abnormalities in his **semen analysis**, indicating a need for intervention.
- Delaying therapy would mean a continued inability to conceive naturally, which is the primary concern for the couple.
*Intracytoplasmic sperm injection*
- **Intracytoplasmic sperm injection (ICSI)** is an assisted reproductive technology used in cases of severe male factor infertility or failed IVF rather than a primary treatment for a correctable cause like varicocele.
- It is typically considered when simpler, less invasive, or corrective treatments have failed or are not applicable. Optimizing natural conception through varicocele repair is usually the first-line approach in such cases.
Male infertility surgical procedures US Medical PG Question 8: A 22-year-old man is brought to the emergency department because of progressive left-sided scrotal pain for 4 hours. He describes the pain as throbbing in nature and 6 out of 10 in intensity. He has vomited once on the way to the hospital. He has had pain during urination for the past 4 days. He has been sexually active with 2 female partners over the past year and uses condoms inconsistently. His father was diagnosed with testicular cancer at the age of 51 years. He appears anxious. His temperature is 36.9°C (98.42°F), pulse is 94/min, and blood pressure is 124/78 mm Hg. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and nontender. Examination shows a tender, swollen left testicle and an erythematous left hemiscrotum. Urine dipstick shows leukocyte esterase; urinalysis shows WBCs. Which of the following is the most appropriate next step in management?
- A. Scrotal ultrasonography (Correct Answer)
- B. CT scan of the abdomen and pelvis
- C. Surgical exploration
- D. Measurement of serum mumps IgG titer
- E. Measurement of serum α-fetoprotein level
Male infertility surgical procedures Explanation: ***Scrotal ultrasonography***
- A definitive diagnosis of **epididymitis**, **orchitis**, or **testicular torsion** requires imaging, which can confirm blood flow to the testis.
- Given the symptoms of testicular pain, tenderness, and inflammation in a sexually active young man, **epididymitis** is highly suspected, but **testicular torsion** must be ruled out as it's a surgical emergency.
*CT scan of the abdomen and pelvis*
- This imaging modality is **not indicated** for the initial evaluation of acute scrotal pain.
- While it can identify other intra-abdominal pathology, it does **not provide sufficient detail** of the scrotal contents or blood flow.
*Surgical exploration*
- **Surgical exploration** is the treatment for **testicular torsion**, but it should only be performed after a clinical or ultrasound diagnosis of testicular torsion is made.
- Doing an immediate surgical exploration without imaging may result in unnecessary surgery if the patient has epididymitis.
*Measurement of serum mumps IgG titer*
- While **mumps orchitis** can cause testicular pain, this patient has symptoms more consistent with an infection related to sexual activity or a potential torsion.
- Measuring mumps titers would **delay diagnosis** and management for more urgent conditions like testicular torsion.
*Measurement of serum α-fetoprotein level*
- **Alpha-fetoprotein (AFP)** is a tumor marker primarily used for the diagnosis and monitoring of **testicular cancer**.
- This patient presents with acute pain and inflammatory signs, which are **not typical for testicular cancer**; AFP measurement is not indicated in the acute setting.
Male infertility surgical procedures US Medical PG Question 9: An 11-year-old boy is brought to the emergency department with sudden and severe pain in the left scrotum that started 2 hours ago. He has vomited twice. He has no dysuria or frequency. There is no history of trauma to the testicles. The temperature is 37.7°C (99.9°F). The left scrotum is swollen, erythematous, and tender. The left testis is elevated and swollen with a transverse lie. The cremasteric reflex is absent. Ultrasonographic examination is currently pending. Which of the following is the most likely diagnosis?
- A. Testicular torsion (Correct Answer)
- B. Mumps orchitis
- C. Spermatocele
- D. Epididymitis
- E. Germ cell tumor
Male infertility surgical procedures Explanation: ***Testicular torsion***
- The sudden onset of **severe scrotal pain** with associated **vomiting**, an **elevated testis**, **transverse lie**, and an **absent cremasteric reflex** are classic signs of testicular torsion.
- This condition is a surgical emergency requiring prompt diagnosis and intervention to prevent testicular ischemia and necrosis.
*Mumps orchitis*
- This typically occurs in post-pubertal males with a history of **mumps infection** and presents with testicular swelling and pain, but usually after the onset of parotitis.
- While it can cause pain and swelling, the **acute onset** and specific findings like absent cremasteric reflex and transverse lie are less characteristic.
*Spermatocele*
- A spermatocele is a **painless, fluid-filled cyst** originating from the epididymis, typically found on the superior aspect of the testis.
- It does not present with acute, severe pain, vomiting, or signs of testicular compromise.
*Epididymitis*
- Epididymitis commonly presents with **gradual onset** of scrotal pain, swelling, and tenderness, often associated with a urinary tract infection or sexually transmitted infection.
- The cremasteric reflex is typically **preserved**, and elevation of the testicle (Prehn's sign) may relieve pain.
*Germ cell tumor*
- Testicular tumors usually present as a **painless lump** or mass in the testis, though some may cause a dull ache or sensation of heaviness.
- Acute severe pain, vomiting, and findings like an absent cremasteric reflex are not typical presentations of a testicular tumor.
Male infertility surgical procedures US Medical PG Question 10: A 16-year-old man presents to the emergency department with a 2-hour history of sudden-onset abdominal pain. He was playing football when his symptoms started. The patient’s past medical history is notable only for asthma. Social history is notable for unprotected sex with 4 women in the past month. His temperature is 99.3°F (37.4°C), blood pressure is 120/88 mmHg, pulse is 117/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam is noted for a non-tender abdomen. Testicular exam reveals a right testicle which is elevated with a horizontal lie and the scrotum is neither swollen nor discolored. Which of the following is the most likely diagnosis?
- A. Traumatic urethral injury
- B. Seminoma
- C. Appendicitis
- D. Epididymitis
- E. Testicular torsion (Correct Answer)
Male infertility surgical procedures Explanation: ***Testicular torsion***
- The sudden onset of **unilateral scrotal pain** in an adolescent, accompanied by an **elevated testicle** with a **horizontal lie**, is highly suggestive of testicular torsion. The absence of scrotal swelling or discoloration in the early stages is also consistent.
- Testicular torsion is a **surgical emergency** requiring prompt intervention to preserve testicular viability.
*Traumatic urethral injury*
- This would typically present with **dysuria**, **hematuria**, inability to void, and potentially **blood at the urethral meatus**, none of which are described.
- A traumatic urethral injury often results from falls, straddle injuries, or pelvic fractures, not typically from playing football without direct trauma to the perineum.
*Seminoma*
- Seminoma is a type of **testicular cancer** that typically presents as a **painless testicular mass**.
- It would not cause sudden, acute abdominal pain and would not manifest with an acutely elevated testicle and horizontal lie.
*Appendicitis*
- Although appendicitis can cause abdominal pain, the **non-tender abdomen** on examination and the specific findings on **testicular examination** (elevated testicle, horizontal lie) make appendicitis unlikely.
- Appendicitis pain typically localizes to the right lower quadrant, often associated with fever, nausea, and vomiting.
*Epididymitis*
- Epididymitis causes **scrotal pain** and **swelling**, often with fever and **dysuria**, usually developing over days, not hours.
- It is often associated with the **Prehn's sign** (pain relief with elevation of the testicle), which is usually absent or negative in torsion. The patient's sexual history might suggest an STI, but the acute presentation and examination findings point away from epididymitis.
More Male infertility surgical procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.