Kidney stone management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Kidney stone management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Kidney stone management US Medical PG Question 1: A 31-year-old obese Caucasian female presents to the Emergency Department late in the evening for left lower quadrant pain that has progressively worsened over the last several hours. She describes the pain as sharp and shooting, coming and going. Her last bowel movement was this morning. She has also had dysuria and urgency. Her surgical history is notable for gastric bypass surgery 2 years prior and an appendectomy at age 9. She is sexually active with her boyfriend and uses condoms. Her temperature is 99.5 deg F (37.5 deg C), blood pressure is 151/83 mmHg, pulse is 86/min, respirations are 14/minute, BMI 32. On physical exam, she has left lower quadrant tenderness to palpation with pain radiating to the left groin and left flank tenderness on palpation. Her urinalysis shows 324 red blood cells/high power field. Her pregnancy test is negative. What is the next best step in management?
- A. A KUB (kidneys, ureters and bladder) plain film
- B. Noncontrast CT scan (Correct Answer)
- C. Exploratory laparoscopy
- D. Transvaginal ultrasound
- E. Intravenous pyelogram
Kidney stone management Explanation: ***Noncontrast CT scan***
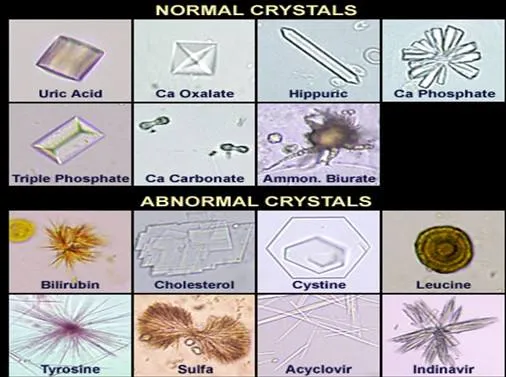
- The patient presents with classic symptoms of **renal colic**, including acute onset, radiating flank and groin pain, dysuria, urgency, and significant hematuria (324 RBCs/HPF) on urinalysis, indicating a likely kidney stone. A **noncontrast CT scan** of the abdomen and pelvis is the most sensitive and specific imaging modality for detecting urinary tract calculi.
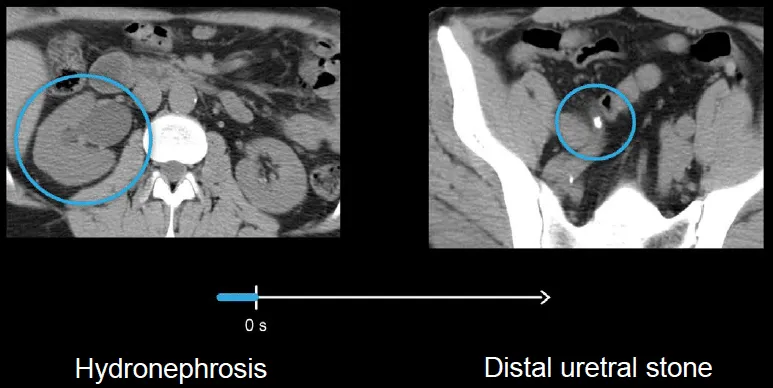
- A noncontrast CT scan can readily identify the size, location, and number of stones, as well as detect complications such as **hydronephrosis**, which is crucial for determining the appropriate management strategy.
*A KUB (kidneys, ureters and bladder) plain film*
- While a KUB plain film can identify some radiopaque stones, it has **limited sensitivity and specificity** compared to CT, especially for radiolucent stones, small stones, or stones obscured by bowel gas.
- **It does not provide information about hydronephrosis** or other renal pathologies, making it less useful for comprehensive evaluation of suspected kidney stones.
*Exploratory laparoscopy*
- This is an **invasive surgical procedure** that is not indicated as a primary diagnostic step for suspected kidney stones.
- Exploratory laparoscopy would only be considered if imaging studies reveal an **acute abdominal emergency** requiring surgical intervention or if the diagnosis remained elusive after less invasive methods.
*Transvaginal ultrasound*
- A transvaginal ultrasound is primarily used to evaluate **pelvic reproductive organs** in females, such as the uterus and ovaries.
- While it can sometimes visualize the distal ureters, it has **poor sensitivity for detecting ureteral stones** and is not the preferred imaging modality for kidney stone diagnosis.
*Intravenous pyelogram*
- An intravenous pyelogram (IVP) involves contrast administration and X-rays and was historically used for kidney stone diagnosis. However, it has been **largely replaced by noncontrast CT** due to its lower sensitivity, slower procedure time, and exposure to intravenous contrast and associated risks.
- CT offers superior anatomical detail and can identify stones more accurately without the need for contrast in the setting of suspected renal colic.
Kidney stone management US Medical PG Question 2: A 37-year-old woman presents to the Emergency Department after 8 hours of left sided flank pain that radiates to her groin and pelvic pain while urinating. Her medical history is relevant for multiple episodes of urinary tract infections, some requiring hospitalization, and intravenous antibiotics. In the hospital, her blood pressure is 125/83 mm Hg, pulse of 88/min, a respiratory rate of 28/min, and a body temperature of 36.5°C (97.7°F). On physical examination, she has left costovertebral tenderness and lower abdominal pain. Laboratory studies include a negative pregnancy test, mild azotemia, and a urinary dipstick that is positive for blood. Which of the following initial tests would be most useful in the diagnosis of this case?
- A. Urine osmolality
- B. Fractional excretion of sodium (FeNa+)
- C. Renal ultrasonography (Correct Answer)
- D. Contrast abdominal computed tomography
- E. Blood urea nitrogen (BUN): serum creatinine (SCr) ratio
Kidney stone management Explanation: ***Renal ultrasonography***
- This is the most appropriate initial imaging test to evaluate for **kidney stones** (given the flank pain radiating to groin and hematuria) and **hydronephrosis** (which can indicate obstruction) and assess for signs of **pyelonephritis** (given the history of recurrent UTIs and CVA tenderness).
- It is **non-invasive**, readily available, and avoids radiation exposure, making it suitable as a first-line diagnostic tool in this setting.
*Urine osmolality*
- This test primarily assesses the kidney's ability to **concentrate urine**, which is more relevant for evaluating fluid balance, diabetes insipidus, or other renal tubular disorders.
- It would not directly diagnose the cause of acute flank pain or urinary tract obstruction.
*Fractional excretion of sodium (FeNa+)*
- FeNa+ is used to differentiate between **prerenal azotemia** and **acute tubular necrosis**, indicating the kidney's response to hypoperfusion.
- While the patient has mild azotemia, FeNa+ would not identify the underlying cause of the flank pain, hematuria, or potential obstruction.
*Contrast abdominal computed tomography*
- While highly sensitive for diagnosing kidney stones and other renal pathologies, **contrast CT** exposes the patient to **ionizing radiation** and risks associated with contrast agents (e.g., contrast-induced nephropathy), especially with pre-existing azotemia.
- It is often reserved for cases where ultrasound is inconclusive or more detailed anatomical information is needed.
*Blood urea nitrogen (BUN): serum creatinine (SCr) ratio*
- This ratio is primarily used to differentiate between **prerenal** causes of acute kidney injury (high ratio, e.g., >20:1) and **intrinsic renal** causes (lower ratio, e.g., <15:1).
- While it can provide insight into the etiology of azotemia, it does not directly identify the cause of the patient's acute flank pain or potential urinary tract obstruction.
Kidney stone management US Medical PG Question 3: Following passage of a calcium oxalate stone, a 55-year-old male visits his physician to learn about nephrolithiasis prevention. Which of the following changes affecting urine composition within the bladder are most likely to protect against crystal precipitation?
- A. Decreased calcium, increased citrate, increased oxalate, increased free water clearance
- B. Increased calcium, increased citrate, increased oxalate, increased free water clearance
- C. Decreased calcium, increased citrate, decreased oxalate, increased free water clearance (Correct Answer)
- D. Decreased calcium, increased citrate, increased oxalate, decreased free water clearance
- E. Decreased calcium, decreased citrate, increased oxalate, increased free water clearance
Kidney stone management Explanation: ***Decreased calcium, increased citrate, decreased oxalate, increased free water clearance***
- **Decreased urinary calcium** and **oxalate** reduce the availability of precursor ions for calcium oxalate crystal formation
- **Increased urinary citrate** acts as a complexing agent with calcium, preventing its binding to oxalate and inhibiting crystal growth
- **Increased free water clearance** leads to dilution of all urinary solutes, reducing supersaturation and preventing crystal precipitation
- All four factors work synergistically to provide maximum protection against nephrolithiasis
*Decreased calcium, increased citrate, increased oxalate, increased free water clearance*
- While decreased calcium, increased citrate, and increased free water clearance are protective, **increased oxalate** significantly increases the risk of calcium oxalate stone formation
- Oxalate is a primary component of calcium oxalate stones, and its increased concentration would counteract other protective mechanisms
*Increased calcium, increased citrate, increased oxalate, increased free water clearance*
- **Increased urinary calcium** and **oxalate** are both risk factors for calcium oxalate stone formation, directly promoting supersaturation
- Although increased citrate and free water clearance are protective, they are unlikely to fully offset the increased risk posed by high calcium and oxalate levels
*Decreased calcium, increased citrate, increased oxalate, decreased free water clearance*
- Although decreased calcium and increased citrate are beneficial, **increased oxalate** and **decreased free water clearance** (leading to more concentrated urine) would both increase the likelihood of crystal precipitation
- The combination of increased oxalate and reduced dilution would outweigh the protective effects
*Decreased calcium, decreased citrate, increased oxalate, increased free water clearance*
- **Decreased urinary citrate** reduces its inhibitory effect on calcium oxalate stone formation, while **increased oxalate** directly promotes crystal precipitation
- These two risk factors would largely negate the preventative effects of decreased calcium and increased free water clearance
Kidney stone management US Medical PG Question 4: A 34-year-old female presents to her primary care physician with complaints of fevers, nausea/vomiting, and severe left flank pain that has developed over the past several hours. She denies any prior episodes similar to her current presentation. Physical examination is significant for a body temperature of 39.1 C and costovertebral angle tenderness. A urinalysis and urine microscopy are ordered. Which of the following findings on kidney histology would be expected in this patient?
- A. Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries
- B. Neutrophils filling the lumens of the renal tubules (Correct Answer)
- C. Scarring of the glomeruli
- D. Interstitial fibrosis and lymphocytic infiltrate
- E. Thickening of the capillaries and glomerular basement membrane
Kidney stone management Explanation: ***Neutrophils filling the lumens of the renal tubules***
- This patient's symptoms (fevers, nausea/vomiting, severe left flank pain, fever, and costovertebral angle tenderness) are highly suggestive of **acute pyelonephritis**, an infection of the kidney parenchyma.
- Histologically, acute pyelonephritis is characterized by an acute inflammatory infiltrate, primarily **neutrophils**, within the **renal tubules** and interstitial tissue, often forming **abscesses**.
*Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries*
- This description is characteristic of **diffuse proliferative glomerulonephritis**, often associated with conditions like **systemic lupus erythematosus (SLE)**.
- The clinical presentation of sudden-onset severe flank pain and fever is not typical for glomerulonephritis, which usually presents with hematuria, proteinuria, and edema.
*Scarring of the glomeruli*
- **Glomerulosclerosis** (scarring of the glomeruli) is a feature of chronic kidney disease and various chronic glomerular disorders, not acute pyelonephritis.
- Patients with glomerular scarring typically present with signs of chronic kidney injury, such as persistent proteinuria and declining renal function, rather than acute infectious symptoms.
*Interstitial fibrosis and lymphocytic infiltrate*
- This is a hallmark of **chronic interstitial nephritis**, which can be caused by long-term drug use, autoimmune diseases, or chronic obstructive uropathy.
- While lymphocytes indicate inflammation, the presence of fibrosis suggests a chronic process, differing from the acute bacterial infection seen in pyelonephritis.
*Thickening of the capillaries and glomerular basement membrane*
- This finding is suggestive of various glomerular diseases, such as **membranous nephropathy** or **diabetic nephropathy**, where the glomerular basement membrane is significantly altered.
- Such conditions typically manifest with proteinuria and nephrotic or nephritic syndromes, not the acute infectious symptoms described.
Kidney stone management US Medical PG Question 5: A 43-year-old man presents with acute-onset left flank pain for the past 6 hours. He describes the pain as severe, intermittent, colicky, and “coming in waves”, and he points to the area of the left costovertebral angle (CVA). He says he recently has been restricting oral liquid intake to only 2 glasses of water per day based on the advice of his healer. He also reports nausea and vomiting. The patient has a history of hypertension, gout, and type 2 diabetes mellitus. He is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. There is exquisite left CVA tenderness. A urinalysis shows gross hematuria. Which of the following is the next best step in the management of this patient?
- A. Non-contrast CT of the abdomen
- B. Contrast CT of the abdomen and pelvis
- C. Supine abdominal radiograph
- D. Renal ultrasound
- E. Non-contrast CT of the abdomen and pelvis (Correct Answer)
Kidney stone management Explanation: **Non-contrast CT of the abdomen and pelvis**
- **Non-contrast CT of the abdomen and pelvis** is the gold standard for diagnosing urolithiasis, providing high sensitivity and specificity for detecting stones, identifying their size and location, and assessing for hydronephrosis.
- The patient's presentation with **acute-onset, severe, colicky flank pain**, nausea, vomiting, gross hematuria, and CVA tenderness is highly suggestive of **renal colic due to a kidney stone**.
*Non-contrast CT of the abdomen*
- This option is **insufficient** as kidney stones can be located in the ureters within the pelvis; a scan of the abdomen alone might miss stones in the distal ureter.
- While a non-contrast CT is appropriate, the scope of only the abdomen is **incomplete** for evaluating the entire urinary tract that might be affected by stones.
*Contrast CT of the abdomen and pelvis*
- **Contrast-enhanced CT is generally not indicated** for the initial evaluation of suspected renal colic due to urolithiasis because it can obscure the visualization of urinary stones.
- The use of contrast also carries risks such as **allergic reaction** and **contrast-induced nephropathy**, which are unnecessary in this acute, non-complicated setting.
*Supine abdominal radiograph*
- A supine abdominal radiograph (KUB) has **limited sensitivity** for detecting kidney stones, especially radiolucent stones (e.g., uric acid stones) or small stones.
- It also provides **poor anatomical detail** and cannot assess for hydronephrosis or other complications as effectively as CT.
*Renal ultrasound*
- Renal ultrasound can detect **hydronephrosis** and some kidney stones but is less sensitive than CT for visualizing smaller stones, especially in the ureters.
- Its diagnostic utility can be **limited by body habitus** and operator dependence, making it less reliable as a primary diagnostic tool for acute renal colic.
Kidney stone management US Medical PG Question 6: A 33-year-old woman comes to the emergency department because of severe right flank pain for 2 hours. The pain is colicky in nature and she describes it as 9 out of 10 in intensity. She has had 2 episodes of vomiting. She has no history of similar episodes in the past. She is 160 cm (5 ft 3 in) tall and weighs 104 kg (229 lb); BMI is 41 kg/m2. Her temperature is 37.3°C (99.1°F), pulse is 96/min, respirations are 16/min and blood pressure is 116/76 mm Hg. The abdomen is soft and there is mild tenderness to palpation in the right lower quadrant. Bowel sounds are reduced. The remainder of the examination shows no abnormalities. Her leukocyte count is 7,400/mm3. A low-dose CT scan of the abdomen and pelvis shows a round 12-mm stone in the distal right ureter. Urine dipstick is mildly positive for blood. Microscopic examination of the urine shows RBCs and no WBCs. 0.9% saline infusion is begun and intravenous ketorolac is administered. Which of the following is the most appropriate next step in management?
- A. Ureteral stenting
- B. Ureteroscopy (Correct Answer)
- C. Observation
- D. Extracorporeal shock wave lithotripsy
- E. Thiazide diuretic therapy
Kidney stone management Explanation: ***Ureteroscopy***
- **Ureteroscopy** is the most appropriate next step for a 12-mm symptomatic distal ureteral stone, especially given its size.
- It allows for direct visualization of the stone and immediate fragmentation or extraction, providing rapid relief of symptoms and addressing the obstruction.
*Ureteral stenting*
- **Ureteral stenting** is primarily used to relieve obstruction and pain, or to bypass the stone, but it does not remove the stone.
- It is often considered a temporary measure to decompress the kidney, particularly in cases of infection or severe obstruction, but definitive treatment for the stone would still be needed.
*Observation*
- **Observation** is generally reserved for smaller ureteral stones (typically <5 mm) that are likely to pass spontaneously.
- A 12-mm stone has a very low chance of spontaneous passage and would likely lead to prolonged pain, obstruction, and potential complications.
*Extracorporeal shock wave lithotripsy*
- **Extracorporeal shock wave lithotripsy (ESWL)** is less effective for larger stones (>10 mm) and stones located in the distal ureter, as successful fragmentation and passage are reduced.
- It is generally more effective for smaller, proximal ureteral or renal stones.
*Thiazide diuretic therapy*
- **Thiazide diuretics** are used as a preventative measure to reduce calcium excretion and thus decrease the risk of new calcium stone formation, but they are not a treatment for an acutely obstructing stone.
- This therapy would not alleviate the current acute pain or obstruction caused by the 12-mm stone.
Kidney stone management US Medical PG Question 7: A 57-year-old man presents with acute-onset nausea and left flank pain. He says his symptoms suddenly started 10 hours ago and have not improved. He describes the pain as severe, colicky, intermittent, and localized to the left flank. The patient denies any fever, chills, or dysuria. His past medical history is significant for nephrolithiasis, incidentally diagnosed 10 months ago on a routine ultrasound, for which he has not been treated. His family history is unremarkable. The patient is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. Severe left costovertebral angle tenderness is noted. Gross hematuria is present on urinalysis. A non-contrast CT of the abdomen and pelvis reveals a 12-mm obstructing calculus at the left ureterovesical junction. Initial management, consisting of IV fluid resuscitation, antiemetics, and analgesia, is administered. Which of the following is the best next step in the management of this patient?
- A. Percutaneous nephrostomy
- B. Percutaneous nephrostolithotomy (PCNL)
- C. Extracorporeal shockwave lithotripsy (ESWL)
- D. 24-hour urine chemistry
- E. Ureteroscopy (Correct Answer)
Kidney stone management Explanation: ***Ureteroscopy***
- Ureteroscopy is the preferred treatment for **prompt stone removal** in patients with a large **ureteral calculus** (e.g., 12 mm) causing obstruction and intractable symptoms, especially when located in the **distal ureter** near the ureterovesical junction.
- This procedure allows for direct visualization of the stone, fragmentation using a **laser**, and removal with a basket, providing immediate relief and preventing potential complications like **hydronephrosis** or infection.
*Percutaneous nephrostomy*
- This procedure is typically reserved for cases where there is **urosepsis** or severe **hydronephrosis** requiring urgent decompression, which is not indicated here as the patient is afebrile and hemodynamically stable.
- While it provides drainage, it does not directly remove the stone and is less definitive for a distal ureteral stone.
*Percutaneous nephrostolithotomy (PCNL)*
- **PCNL** is primarily used for **large kidney stones** (> 2 cm) or complex renal calculi, not for ureteral stones.
- It involves accessing the kidney directly through the skin to remove stones, which is an overly invasive approach for a stone located at the ureterovesical junction.
*Extracorporeal shockwave lithotripsy (ESWL)*
- **ESWL** is less effective for large, **distal ureteral stones**, as the success rate for stones greater than 10 mm and those located distally is lower.
- While it is non-invasive, ureteroscopy offers a higher success rate for immediate clearance in this specific clinical scenario.
*24-hour urine chemistry*
- This is a diagnostic study performed to evaluate the **metabolic causes of stone formation** and to guide preventive strategies.
- It is an important step in preventing future stone recurrence but is not an immediate management step for an acute, obstructing ureteral stone.
Kidney stone management US Medical PG Question 8: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Kidney stone management Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Kidney stone management US Medical PG Question 9: A 50-year-old man is brought to the emergency department because of a 3-day history of left flank pain. The patient has had two episodes of urolithiasis during the last year. He initially had pain with urination that improved with oxycodone. Over the past day, the pain has worsened and he has additionally developed fever and chills. He has hypertension and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 20 years. He does not drink alcohol. His current medications include metformin and lisinopril. The patient appears ill and uncomfortable. His temperature is 39.1°C (102.3°F), pulse is 108/min, respirations are 22/min, and blood pressure is 90/62 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. Examination of the back shows left costovertebral angle tenderness. Physical and neurologic examinations show no other abnormalities. Laboratory studies show:
Hemoglobin 14.2 g/dL
Leukocyte count 13,900/mm3
Hemoglobin A1c 8.2%
Serum
Na+ 138 mEq/L
K+ 3.8 mEq/L
Cl-
98 mEq/L
Calcium 9.3 mg/dL
Glucose 190 mg/dL
Creatinine 2.1 mg/dL
Urine pH 8.3
Urine microscopy
Bacteria moderate
RBC 6–10/hpf
WBC 10–15/hpf
WBC casts numerous
Ultrasound shows enlargement of the left kidney with a dilated pelvis and echogenic debris. CT scan shows a 16-mm stone at the left ureteropelvic junction, dilation of the collecting system, thickening of the wall of the renal pelvis, and signs of perirenal inflammation. Intravenous fluid resuscitation and intravenous ampicillin, gentamicin, and morphine are begun. Which of the following is the most appropriate next step in the management of this patient?
- A. Intravenous pyelography
- B. Tamsulosin therapy
- C. Percutaneous nephrostomy (Correct Answer)
- D. Shock wave lithotripsy
- E. Ureteroscopy and stent placement
Kidney stone management Explanation: ***Percutaneous nephrostomy***
- The patient presents with **obstructive pyelonephritis** due to a large **ureteral stone** (16 mm) and signs of **urosepsis** (fever, chills, hypotension, leukocytosis, elevated creatinine).
- **Urgent decompression** of the obstructed kidney is critical to relieve pressure, improve renal function, and control infection. A percutaneous nephrostomy provides immediate drainage, which is life-saving in this severe context.
*Intravenous pyelography*
- This is an imaging study used to visualize the urinary tract and is **contraindicated** in patients with **renal insufficiency** (creatinine 2.1 mg/dL) due to the risk of contrast-induced nephropathy.
- Furthermore, it would only provide diagnostic information and **would not address the urgent need for renal decompression** in a patient with urosepsis.
*Tamsulosin therapy*
- **Alpha-blockers** like tamsulosin can facilitate the passage of **smaller ureteral stones** (typically <10 mm) by relaxing ureteral smooth muscle.
- However, this patient has a **large stone (16 mm)**, signs of **sepsis**, and **renal obstruction**, making medical expulsive therapy ineffective and dangerous as a primary intervention.
*Shock wave lithotripsy*
- **Extracorporeal shock wave lithotripsy (ESWL)** is a non-invasive procedure for breaking up kidney stones into smaller fragments.
- It is **contraindicated** in patients with active **urinary tract infections** or **sepsis** because of the risk of disseminating the infection.
*Ureteroscopy and stent placement*
- While ureteroscopy with stent placement can relieve obstruction, it is an **invasive procedure** that may be challenging in a patient with severe sepsis and inflammation.
- **Percutaneous nephrostomy** offers a less invasive and more immediate way to achieve **decompression** in an unstable patient, with definitive stone management to follow once the infection is controlled.
Kidney stone management US Medical PG Question 10: A 70-year-old man with metastatic castration-resistant prostate cancer presents to the emergency department with severe back pain, bilateral lower extremity weakness (3/5 strength), and urinary retention that started 8 hours ago. He has known bone metastases and his PSA has been rising despite androgen deprivation therapy. MRI spine shows an epidural mass at T10 with severe spinal cord compression and near-complete canal obliteration. He is neurologically intact above T10. Radiation oncology, neurosurgery, and medical oncology are consulted. Evaluate the optimal management approach.
- A. Corticosteroids, radiation therapy, and switch to next-line systemic therapy
- B. Stereotactic radiosurgery as single-modality treatment
- C. Emergent surgical decompression followed by radiation therapy (Correct Answer)
- D. Palliative care consultation and comfort measures only given metastatic disease
- E. High-dose corticosteroids and emergent radiation therapy alone
Kidney stone management Explanation: ***Emergent surgical decompression followed by radiation therapy***
- For patients with **malignant spinal cord compression (MSCC)** and acute neurologic deficits lasting <48 hours, **decompressive surgery** followed by radiotherapy results in better ambulatory outcomes than radiation alone.
- This patient has a **single level of compression** (T10) and a reasonable functional status above the lesion, making him an ideal candidate for surgery to preserve **quality of life**.
*Corticosteroids, radiation therapy, and switch to next-line systemic therapy*
- While **systemic therapy** is important for managing metastatic disease, it does not address the acute **mechanical compression** currently threatening spinal cord viability.
- Postponing definitive mechanical decompression in favor of systemic treatment would likely result in **permanent paraplegia** given the severe canal obliteration.
*Stereotactic radiosurgery as single-modality treatment*
- **Stereotactic radiosurgery (SRS)** is effective for spinal metastases but is generally not the primary choice when there is **high-grade spinal cord compression** with an associated neurologic deficit.
- Surgery is needed first to provide immediate **mechanical decompression** and create a "separation" distance between the cord and the tumor for safer high-dose radiation.
*Palliative care consultation and comfort measures only given metastatic disease*
- Although the cancer is metastatic, preserving **ambulatory function** and bladder control is a priority for maintaining dignity and independence.
- **MSCC** is an oncologic emergency where intervention is indicated unless the patient's **life expectancy** is very short (typically <3 months), which is not clearly the case here.
*High-dose corticosteroids and emergent radiation therapy alone*
- Radiation therapy alone is typically reserved for patients who are not **surgical candidates**, have multisegmental disease, or have complete paralysis for >48 hours.
- **Direct decompressive surgery** is superior for restoring and maintaining the ability to walk in patients with acute, unstable neurologic symptoms from a **single-level mass**.
More Kidney stone management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.