Cystoscopy and urethroscopy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cystoscopy and urethroscopy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cystoscopy and urethroscopy US Medical PG Question 1: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Cystoscopy and urethroscopy Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
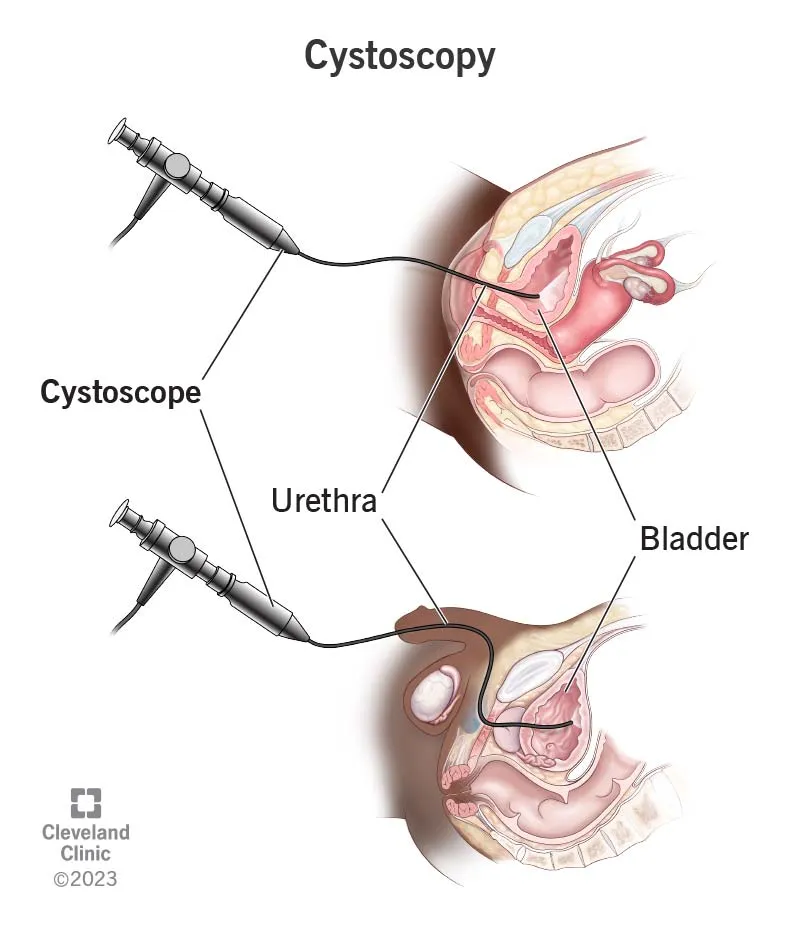
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Cystoscopy and urethroscopy US Medical PG Question 2: A 31-year-old obese Caucasian female presents to the Emergency Department late in the evening for left lower quadrant pain that has progressively worsened over the last several hours. She describes the pain as sharp and shooting, coming and going. Her last bowel movement was this morning. She has also had dysuria and urgency. Her surgical history is notable for gastric bypass surgery 2 years prior and an appendectomy at age 9. She is sexually active with her boyfriend and uses condoms. Her temperature is 99.5 deg F (37.5 deg C), blood pressure is 151/83 mmHg, pulse is 86/min, respirations are 14/minute, BMI 32. On physical exam, she has left lower quadrant tenderness to palpation with pain radiating to the left groin and left flank tenderness on palpation. Her urinalysis shows 324 red blood cells/high power field. Her pregnancy test is negative. What is the next best step in management?
- A. A KUB (kidneys, ureters and bladder) plain film
- B. Noncontrast CT scan (Correct Answer)
- C. Exploratory laparoscopy
- D. Transvaginal ultrasound
- E. Intravenous pyelogram
Cystoscopy and urethroscopy Explanation: ***Noncontrast CT scan***
- The patient presents with classic symptoms of **renal colic**, including acute onset, radiating flank and groin pain, dysuria, urgency, and significant hematuria (324 RBCs/HPF) on urinalysis, indicating a likely kidney stone. A **noncontrast CT scan** of the abdomen and pelvis is the most sensitive and specific imaging modality for detecting urinary tract calculi.
- A noncontrast CT scan can readily identify the size, location, and number of stones, as well as detect complications such as **hydronephrosis**, which is crucial for determining the appropriate management strategy.
*A KUB (kidneys, ureters and bladder) plain film*
- While a KUB plain film can identify some radiopaque stones, it has **limited sensitivity and specificity** compared to CT, especially for radiolucent stones, small stones, or stones obscured by bowel gas.
- **It does not provide information about hydronephrosis** or other renal pathologies, making it less useful for comprehensive evaluation of suspected kidney stones.
*Exploratory laparoscopy*
- This is an **invasive surgical procedure** that is not indicated as a primary diagnostic step for suspected kidney stones.
- Exploratory laparoscopy would only be considered if imaging studies reveal an **acute abdominal emergency** requiring surgical intervention or if the diagnosis remained elusive after less invasive methods.
*Transvaginal ultrasound*
- A transvaginal ultrasound is primarily used to evaluate **pelvic reproductive organs** in females, such as the uterus and ovaries.
- While it can sometimes visualize the distal ureters, it has **poor sensitivity for detecting ureteral stones** and is not the preferred imaging modality for kidney stone diagnosis.
*Intravenous pyelogram*
- An intravenous pyelogram (IVP) involves contrast administration and X-rays and was historically used for kidney stone diagnosis. However, it has been **largely replaced by noncontrast CT** due to its lower sensitivity, slower procedure time, and exposure to intravenous contrast and associated risks.
- CT offers superior anatomical detail and can identify stones more accurately without the need for contrast in the setting of suspected renal colic.
Cystoscopy and urethroscopy US Medical PG Question 3: A 61-year-old G4P3 presents with a 5-year history of involuntary urine loss on coughing, sneezing, and physical exertion. She denies urine leakage at night. She has been menopausal since 51 years of age. She is otherwise healthy and is not on any medications, including hormone replacement therapy. The weight is 78 kg (172 lb) and the height is 156 cm (5.1 ft). The vital signs are within normal limits. The physical examination shows no costovertebral angle tenderness. The neurologic examination is unremarkable. The gynecologic examination revealed pale and thin vulvar and vaginal mucosa. The external urethral opening appears normal; there is urine leakage when the patient is asked to cough. The Q-tip test is positive. The bimanual exam reveals painless bulging of the anterior vaginal wall. Which of the following findings are most likely to be revealed by cystometry?
- A. Increased residual volume, involuntary detrusor contractions on maximal bladder filling
- B. Normal residual volume, no involuntary detrusor contractions (Correct Answer)
- C. Normal residual volume, involuntary detrusor contractions on minimal bladder filling
- D. Normal residual volume, involuntary detrusor contractions on maximal bladder filling
- E. Increased residual volume, no involuntary detrusor contractions
Cystoscopy and urethroscopy Explanation: ***Normal residual volume, no involuntary detrusor contractions***
- The patient's symptoms (involuntary urine loss on coughing, sneezing, and physical exertion, denial of nocturnal leakage) are classic for **stress urinary incontinence (SUI)**. SUI is due to **urethral hypermobility** or intrinsic sphincter deficiency, not detrusor overactivity, hence *no involuntary detrusor contractions*.
- **Normal residual volume** is expected in SUI as the bladder empties appropriately; the issue is with urethral support during increased intra-abdominal pressure.
*Increased residual volume, involuntary detrusor contractions on maximal bladder filling*
- **Increased residual volume** is not typical in pure SUI and might suggest bladder outlet obstruction or an underactive detrusor.
- **Involuntary detrusor contractions** indicate **urge incontinence** or overactive bladder, which is inconsistent with the patient's presentation of leakage only with exertion and no nocturnal symptoms.
*Normal residual volume, involuntary detrusor contractions on minimal bladder filling*
- While **normal residual volume** is consistent, **involuntary detrusor contractions** at *minimal* bladder filling are characteristic of a severely overactive bladder or neurogenic bladder, which is not suggested by the patient's symptoms (leakage only with exertion).
*Normal residual volume, involuntary detrusor contractions on maximal bladder filling*
- **Involuntary detrusor contractions**, even at maximal filling, are a feature of **detrusor overactivity**, leading to **urge incontinence**. This pattern of leakage is unrelated to the patient's reported stress-related symptoms.
*Increased residual volume, no involuntary detrusor contractions*
- **Increased residual volume** without involuntary detrusor contractions could point towards **bladder outlet obstruction** or **detrusor underactivity**. Neither of these conditions typically presents with urine leakage exclusively upon coughing, sneezing, or exertion.
Cystoscopy and urethroscopy US Medical PG Question 4: A 56-year-old man undergoes a cystoscopy for the evaluation of macroscopic hematuria. During the procedure, an opening covered with a mucosal flap is visualized at the base of the trigone. Which of the following best describes this structure?
- A. Ejaculatory duct opening
- B. Ureteric orifice (Correct Answer)
- C. Diverticular opening
- D. Prostatic utricle
- E. Internal urethral orifice
Cystoscopy and urethroscopy Explanation: ***Ureteric orifice***
- The description of an opening covered with a **mucosal flap** specifically at the **base of the trigone** is characteristic of a normal ureteric orifice, which prevents reflux of urine.
- The trigone is a triangular area at the base of the bladder formed by the two ureteric orifices and the internal urethral orifice.
*Ejaculatory duct opening*
- The ejaculatory ducts open into the **prostatic urethra**, not directly into the bladder trigone.
- They are typically located on the **verumontanum** within the prostatic urethra, posterior to the bladder neck.
*Diverticular opening*
- A diverticulum is an **outpouching** of the bladder wall, and its opening can appear anywhere, not specifically at the base of the trigone with a mucosal flap.
- While it's an opening, it would represent a pathological condition, not a normal anatomical structure.
*Prostatic utricle*
- The prostatic utricle is a small blind-ending pouch located in the **prostatic urethra**, often on the verumontanum.
- It is an embryonic remnant and is not found at the base of the bladder trigone.
*Internal urethral orifice*
- This is the opening of the **urethra** from the bladder, located at the **apex of the trigone**, not covered by a mucosal flap in the same way as a ureteric orifice.
- It marks the junction between the bladder and the urethra.
Cystoscopy and urethroscopy US Medical PG Question 5: A 57-year-old man presents with acute-onset nausea and left flank pain. He says his symptoms suddenly started 10 hours ago and have not improved. He describes the pain as severe, colicky, intermittent, and localized to the left flank. The patient denies any fever, chills, or dysuria. His past medical history is significant for nephrolithiasis, incidentally diagnosed 10 months ago on a routine ultrasound, for which he has not been treated. His family history is unremarkable. The patient is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. Severe left costovertebral angle tenderness is noted. Gross hematuria is present on urinalysis. A non-contrast CT of the abdomen and pelvis reveals a 12-mm obstructing calculus at the left ureterovesical junction. Initial management, consisting of IV fluid resuscitation, antiemetics, and analgesia, is administered. Which of the following is the best next step in the management of this patient?
- A. Percutaneous nephrostomy
- B. Percutaneous nephrostolithotomy (PCNL)
- C. Extracorporeal shockwave lithotripsy (ESWL)
- D. 24-hour urine chemistry
- E. Ureteroscopy (Correct Answer)
Cystoscopy and urethroscopy Explanation: ***Ureteroscopy***
- Ureteroscopy is the preferred treatment for **prompt stone removal** in patients with a large **ureteral calculus** (e.g., 12 mm) causing obstruction and intractable symptoms, especially when located in the **distal ureter** near the ureterovesical junction.
- This procedure allows for direct visualization of the stone, fragmentation using a **laser**, and removal with a basket, providing immediate relief and preventing potential complications like **hydronephrosis** or infection.
*Percutaneous nephrostomy*
- This procedure is typically reserved for cases where there is **urosepsis** or severe **hydronephrosis** requiring urgent decompression, which is not indicated here as the patient is afebrile and hemodynamically stable.
- While it provides drainage, it does not directly remove the stone and is less definitive for a distal ureteral stone.
*Percutaneous nephrostolithotomy (PCNL)*
- **PCNL** is primarily used for **large kidney stones** (> 2 cm) or complex renal calculi, not for ureteral stones.
- It involves accessing the kidney directly through the skin to remove stones, which is an overly invasive approach for a stone located at the ureterovesical junction.
*Extracorporeal shockwave lithotripsy (ESWL)*
- **ESWL** is less effective for large, **distal ureteral stones**, as the success rate for stones greater than 10 mm and those located distally is lower.
- While it is non-invasive, ureteroscopy offers a higher success rate for immediate clearance in this specific clinical scenario.
*24-hour urine chemistry*
- This is a diagnostic study performed to evaluate the **metabolic causes of stone formation** and to guide preventive strategies.
- It is an important step in preventing future stone recurrence but is not an immediate management step for an acute, obstructing ureteral stone.
Cystoscopy and urethroscopy US Medical PG Question 6: A 42-year-old woman comes to the physician because of right flank pain that started 3 days following a procedure. Her vital signs are within normal limits. Physical examination shows right costovertebral angle tenderness. An intravenous pyelogram shows a dilated renal pelvis and ureter on the right with a lack of contrast proximal to the ureterovesical junction. This patient most likely recently underwent which of the following procedures?
- A. Hysterectomy (Correct Answer)
- B. Foley catheter insertion
- C. Cesarean delivery
- D. Appendectomy
- E. Inguinal hernia repair
Cystoscopy and urethroscopy Explanation: ***Hysterectomy***
- **Ureteral injury** is a known complication of hysterectomy due to the ureter's close proximity to the uterine arteries and adnexa, especially near the **ureterovesical junction**.
- The presented symptoms of flank pain, CVA tenderness, and hydronephrosis (dilated renal pelvis and ureter with lack of contrast flow) occurring post-procedure strongly indicate **ureteral obstruction** or injury during the surgery.
*Foley catheter insertion*
- While catheterization can cause trauma, it would typically lead to **urethral or bladder injury**, not a ureteral obstruction at the ureterovesical junction causing hydronephrosis.
- The symptoms are more consistent with an injury higher up in the urinary tract that is not usually associated with a Foley catheter.
*Cesarean delivery*
- A C-section involves opening the abdomen to deliver a baby, but it generally does not involve dissection near the ureters to the extent that a hysterectomy does, making ureteral injury less common.
- The primary surgical field during a C-section is the uterus, while ureteral injury is more characteristic of procedures involving extensive pelvic dissection, such as hysterectomy.
*Appendectomy*
- An appendectomy is a procedure to remove the appendix and typically involves the right lower quadrant of the abdomen, away from the course of the ureter and ureterovesical junction.
- Injury to the ureter is a very rare complication of appendectomy and would not typically manifest as this type of obstruction.
*Inguinal hernia repair*
- Inguinal hernia repair involves structures in the groin region, anterior to the peritoneal cavity, and is far removed from the ureters and bladder.
- Ureteral injury is not a recognized complication of inguinal hernia repair.
Cystoscopy and urethroscopy US Medical PG Question 7: Please refer to the summary above to answer this question
Which of the following is the most likely diagnosis?
Patient Information
Age: 66 years
Gender: M, self-identified
Ethnicity: African-American
Site of Care: office
History
Reason for Visit/Chief Concern: "I need to go to the bathroom all the time."
History of Present Illness:
1-year history of frequent urination
urinates every 2–3 hours during the day and wakes up at least 3 times at night to urinate
has had 2 episodes of cystitis treated with antibiotics in the past 4 months
has a weak urinary stream
has not noticed any blood in the urine
does not have any pain with urination or ejaculatory dysfunction
Past Medical History:
type 2 diabetes mellitus
nephrolithiasis, treated with percutaneous nephrolithotomy
essential tremor
Medications:
metformin, canagliflozin, propranolol
Allergies:
sulfa drugs
Social History:
sexually active with his wife; does not use condoms consistently
has smoked one pack of cigarettes daily for 50 years
drinks one to two glasses of beer weekly
Physical Examination
Temp Pulse Resp BP O2 Sat Ht Wt BMI
37°C
(98.6°F)
72/min 16/min 134/81 mm Hg –
183 cm
(6 ft)
105 kg
(231 lb)
31 kg/m2
Appearance: no acute distress
Pulmonary: clear to auscultation
Cardiac: regular rate and rhythm; normal S1, S2; S4 gallop
Abdominal: overweight; no tenderness, guarding, masses, bruits, or hepatosplenomegaly
Extremities: no joint erythema, edema, or warmth; dorsalis pedis, radial, and femoral pulses intact
Genitourinary: no lesions or discharge
Rectal: slightly enlarged, smooth, nontender prostate
Neurologic: alert and oriented; cranial nerves grossly intact; no focal neurologic deficits
- A. Urethral stricture
- B. Prostate cancer
- C. Neurogenic bladder
- D. Acute prostatitis
- E. Benign prostatic hyperplasia (Correct Answer)
Cystoscopy and urethroscopy Explanation: ***Benign prostatic hyperplasia***
- The patient's symptoms of **frequent urination**, **nocturia**, **weak urinary stream**, and a **slightly enlarged, smooth, nontender prostate** on rectal exam are classic for BPH.
- Recurrent **cystitis** can be a complication of BPH due to incomplete bladder emptying.
*Urethral stricture*
- While a urethral stricture can cause a **weak urinary stream** and incomplete emptying, it would typically present with more significant difficulty voiding, possibly **pain** during urination, or a history of instrumentation/trauma.
- The rectal exam finding of an **enlarged prostate** points away from a primary stricture.
*Prostate cancer*
- Although prostate cancer can cause similar urinary symptoms, an enlarged prostate due to cancer is often described as **nodular, firm, or asymmetric** on rectal exam, not smooth.
- The absence of **hematuria** or significant pain also makes cancer less likely as the primary driver of these symptoms.
*Neurogenic bladder*
- A neurogenic bladder would involve neurological deficits affecting bladder control, such as spinal cord injury, stroke, or severe neuropathy, which are not described in this patient beyond an **essential tremor** unlikely to cause these specific lower urinary tract symptoms.
- The patient has no other neurological symptoms like **focal weakness** or sensory loss.
*Acute prostatitis*
- Acute prostatitis typically presents with **fever, chills, perineal pain, dysuria**, and a **tender, swollen prostate** on examination, none of which are present in this patient.
- The symptoms here are **chronic** (1 year history) rather than acute.
Cystoscopy and urethroscopy US Medical PG Question 8: Four hours after undergoing an abdominal hysterectomy, a 43-year-old woman is evaluated in the post-anesthesia care unit because she has only had a urine output of 5 mL of blue-tinged urine since surgery. The operation went smoothly and ureter patency was checked via retrograde injection of methylene blue dye mixed with saline through the Foley catheter. She received 2.4 L of crystalloid fluids intraoperatively and urine output was 1.2 L. She had a history of fibroids with painful and heavy menses. She is otherwise healthy. She underwent 2 cesarean sections 8 and 5 years ago, respectively. Her temperature is 37.4°C (99.3°F), pulse is 75/min, respirations are 16/min, and blood pressure is 122/76 mm Hg. She appears comfortable. Cardiopulmonary examination shows no abnormalities. There is a midline surgical incision with clean and dry dressings. Her abdomen is soft and mildly distended in the lower quadrants. Her bladder is slightly palpable. Extremities are warm and well perfused, and capillary refill is brisk. Laboratory studies show:
Leukocyte count 8,300/mm3
Hemoglobin 10.3 g/dL
Hematocrit 31%
Platelet count 250,000/mm3
Serum
_Na+ 140 mEq/L
_K+ 4.2 mEq/L
_HCO3+ 26 mEq/L
_Urea nitrogen 26 mg/dL
_Creatinine 1.0 mg/dL
Urine
_Blood 1+
_WBC none
_Protein negative
_RBC none
_RBC casts none
A bladder scan shows 250 mL of retained urine. Which of the following is the next best step in the evaluation of this patient?
- A. Check the Foley catheter (Correct Answer)
- B. Return to the operating room for emergency surgery
- C. Perform ultrasound of the kidneys
- D. Administer 20 mg of IV furosemide
- E. Administer bolus 500 mL of Lactated Ringers
Cystoscopy and urethroscopy Explanation: ***Check the Foley catheter***
- This patient presents with signs of **urinary retention** (low urine output, palpable bladder, retained urine on bladder scan) despite methylene blue injection confirming ureter patency. The most common and easily reversible cause of low urine output post-hysterectomy is a **kinked or obstructed Foley catheter**.
- Given the smooth intraoperative course and adequate urine output during surgery, a quick check and potential **repositioning or flushing of the catheter** is the immediate and most appropriate first step before considering more invasive interventions.
*Return to the operating room for emergency surgery*
- This is a drastic step and is not indicated at this stage. There is no evidence of a **surgical complication** requiring emergency intervention, such as a ureteral injury (which was checked intraoperatively) or active hemorrhage.
- The patient's vital signs are stable, and she appears comfortable, which makes an emergency surgical re-exploration highly unlikely as the initial best step.
*Perform ultrasound of the kidneys*
- While a renal ultrasound can assess for **hydronephrosis** or other kidney abnormalities, it is a delayed step. Given the clear evidence of bladder retention and the possibility of a simple catheter malfunction, performing an ultrasound without first addressing the catheter would be premature.
- The patient's **creatinine is normal**, making acute kidney injury due to obstruction less likely as an immediate concern.
*Administer 20 mg of IV furosemide*
- Furosemide is a **loop diuretic** that increases urine production. However, it would be ineffective and potentially harmful if the issue is a mechanical obstruction of urine outflow, as appears to be the case here.
- Administering a diuretic without addressing the outflow problem would only worsen bladder distension and potentially stress the renal system without resolving the underlying issue.
*Administer bolus 500 mL of Lactated Ringers*
- This patient has already received 2.4 L of crystalloid fluids intraoperatively and has stable vital signs, indicating she is likely **euvolemic**.
- Giving another fluid bolus would not address the observed urinary retention and could lead to **fluid overload** if the urine outflow obstruction persists.
Cystoscopy and urethroscopy US Medical PG Question 9: A 33-year-old man is brought to the emergency department 20 minutes after losing control over his bicycle and colliding with a parked car. The handlebar of the bicycle hit his lower abdomen. On arrival, he is alert and oriented. His pulse is 90/min, respirations are 17/min and blood pressure is 110/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. The pupils are equal and reactive to light. There are multiple bruises over his chest and lower extremities. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. There is no pelvic instability. Rectal examination is unremarkable. A complete blood count, prothrombin time, and serum concentrations of glucose, creatinine, and electrolytes are within the reference range. Urine dipstick is mildly positive for blood. Microscopic examination of the urine shows 20 RBCs/hpf. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. Laparotomy
- C. Observation and follow-up
- D. Suprapubic catheterization
- E. CT scan of the abdomen and pelvis (Correct Answer)
Cystoscopy and urethroscopy Explanation: ***CT scan of the abdomen and pelvis***
- This patient has suffered significant trauma to the lower abdomen, as indicated by colliding with a parked car and handlebar impact, along with **hematuria** (urine dipstick positive for blood, 20 RBCs/hpf).
- A CT scan of the abdomen and pelvis is crucial to assess for potential **intra-abdominal organ injury**, particularly to the kidneys, bladder, or bowel, given the mechanism of injury and the presence of hematuria.
*Intravenous pyelography*
- While IVP can visualize the urinary tract, it is generally **less sensitive and specific** than CT scanning for detecting trauma-related urinary tract injuries and concurrent injuries to other abdominal organs.
- Furthermore, modern trauma care primarily utilizes **CT scanning** due to its superior anatomical detail and ability to assess multiple organ systems simultaneously.
*Laparotomy*
- **Exploratory laparotomy** is a surgical procedure indicated for patients with signs of **hemodynamic instability**, peritonitis, or clear evidence of severe intra-abdominal injury, none of which are present in this hemodynamically stable patient.
- Performing a laparotomy without further diagnostic imaging in a stable patient is premature and carries unnecessary risks.
*Observation and follow-up*
- While the patient is currently hemodynamically stable and the abdomen is soft and non-tender, the **mechanism of injury** (handlebar impact to the lower abdomen) combined with **hematuria** suggests a high likelihood of significant internal injury that requires further evaluation.
- **Observation alone** without imaging could lead to delayed diagnosis and treatment of a potentially serious injury to the urinary tract or other abdominal organs.
*Suprapubic catheterization*
- **Suprapubic catheterization** is used to drain the bladder when urethral catheterization is not possible or contraindicated, for example in cases of suspected urethral injury.
- There is no indication of urethral injury here (**unremarkable rectal exam**, no gross blood at the meatus), and the primary concern is evaluation of the organs, not bladder drainage.
Cystoscopy and urethroscopy US Medical PG Question 10: A 65-year-old African American man presents for follow-up examination with a 6-month history of urinary hesitancy, weak stream, and terminal dribbling, which is refractory to a combination therapy of finasteride and tamsulosin. The patient’s past medical history is otherwise unremarkable. His father and brother were diagnosed with prostate cancer at the age of 55 years. His vital signs are within normal limits. The patient has a normal anal sphincter tone and a bulbocavernosus muscle reflex. Digital rectal exam (DRE) reveals a prostate size equivalent to 2 finger pads with a hard nodule and without fluctuance or tenderness. Serum prostate-specific antigen (PSA) level is 5 ng/mL. Which of the following investigations is most likely to establish a definitive diagnosis?
- A. Magnetic resonance imaging (MRI)
- B. 4Kscore test
- C. Prostate Health Index (PHI)
- D. Image-guided needle biopsy (Correct Answer)
- E. PSA in 3 months
Cystoscopy and urethroscopy Explanation: ***Image-guided needle biopsy***
- A definitive diagnosis of **prostate cancer** requires histological confirmation, which is achieved through a **biopsy**.
- The patient's presentation with a **hard nodule** on DRE, elevated PSA, and a strong family history of prostate cancer, despite treatment for BPH, strongly indicates the need for a biopsy.
*Magnetic resonance imaging (MRI)*
- While MRI can help in **staging prostate cancer** and guiding biopsies, it does not provide a definitive diagnosis on its own.
- An MRI may identify suspicious lesions but **cannot confirm malignancy** without tissue sampling.
*4Kscore test*
- The 4Kscore test estimates the **risk of high-grade prostate cancer** but does not provide a definitive diagnosis.
- It uses a panel of four prostate-specific kallikrein proteins, along with patient age, DRE status, and prior biopsy results, to calculate a risk score.
*Prostate Health Index (PHI)*
- The PHI is a blood test that combines total PSA, free PSA, and [-2]proPSA to assess the **probability of prostate cancer**.
- It helps in deciding whether a biopsy is needed, but like the 4Kscore, it is not a diagnostic tool in itself.
*PSA in 3 months*
- Re-checking PSA in 3 months would **delay definitive diagnosis** and treatment for a potentially aggressive cancer, especially given the palpable nodule and family history.
- The current PSA of 5 ng/mL, although not extremely high, combined with the suspicious DRE finding, warrants more immediate action.
More Cystoscopy and urethroscopy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.