Bladder cancer surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bladder cancer surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bladder cancer surgical management US Medical PG Question 1: A 31-year-old obese Caucasian female presents to the Emergency Department late in the evening for left lower quadrant pain that has progressively worsened over the last several hours. She describes the pain as sharp and shooting, coming and going. Her last bowel movement was this morning. She has also had dysuria and urgency. Her surgical history is notable for gastric bypass surgery 2 years prior and an appendectomy at age 9. She is sexually active with her boyfriend and uses condoms. Her temperature is 99.5 deg F (37.5 deg C), blood pressure is 151/83 mmHg, pulse is 86/min, respirations are 14/minute, BMI 32. On physical exam, she has left lower quadrant tenderness to palpation with pain radiating to the left groin and left flank tenderness on palpation. Her urinalysis shows 324 red blood cells/high power field. Her pregnancy test is negative. What is the next best step in management?
- A. A KUB (kidneys, ureters and bladder) plain film
- B. Noncontrast CT scan (Correct Answer)
- C. Exploratory laparoscopy
- D. Transvaginal ultrasound
- E. Intravenous pyelogram
Bladder cancer surgical management Explanation: ***Noncontrast CT scan***
- The patient presents with classic symptoms of **renal colic**, including acute onset, radiating flank and groin pain, dysuria, urgency, and significant hematuria (324 RBCs/HPF) on urinalysis, indicating a likely kidney stone. A **noncontrast CT scan** of the abdomen and pelvis is the most sensitive and specific imaging modality for detecting urinary tract calculi.
- A noncontrast CT scan can readily identify the size, location, and number of stones, as well as detect complications such as **hydronephrosis**, which is crucial for determining the appropriate management strategy.
*A KUB (kidneys, ureters and bladder) plain film*
- While a KUB plain film can identify some radiopaque stones, it has **limited sensitivity and specificity** compared to CT, especially for radiolucent stones, small stones, or stones obscured by bowel gas.
- **It does not provide information about hydronephrosis** or other renal pathologies, making it less useful for comprehensive evaluation of suspected kidney stones.
*Exploratory laparoscopy*
- This is an **invasive surgical procedure** that is not indicated as a primary diagnostic step for suspected kidney stones.
- Exploratory laparoscopy would only be considered if imaging studies reveal an **acute abdominal emergency** requiring surgical intervention or if the diagnosis remained elusive after less invasive methods.
*Transvaginal ultrasound*
- A transvaginal ultrasound is primarily used to evaluate **pelvic reproductive organs** in females, such as the uterus and ovaries.
- While it can sometimes visualize the distal ureters, it has **poor sensitivity for detecting ureteral stones** and is not the preferred imaging modality for kidney stone diagnosis.
*Intravenous pyelogram*
- An intravenous pyelogram (IVP) involves contrast administration and X-rays and was historically used for kidney stone diagnosis. However, it has been **largely replaced by noncontrast CT** due to its lower sensitivity, slower procedure time, and exposure to intravenous contrast and associated risks.
- CT offers superior anatomical detail and can identify stones more accurately without the need for contrast in the setting of suspected renal colic.
Bladder cancer surgical management US Medical PG Question 2: A 75-year-old man presents to the physician because of bloody urine, which has occurred several times over the past month. He has no dysuria or flank pain. He has no history of serious illness, and he currently takes no medications. He is a 40-pack-year smoker. The vital signs are within normal limits. Physical exam shows no abnormalities except generalized lung wheezing. The laboratory test results are as follows:
Urine:
Blood 3+
RBC > 100/hpf
WBC 1–2/hpf
RBC casts negative
Bacteria not seen
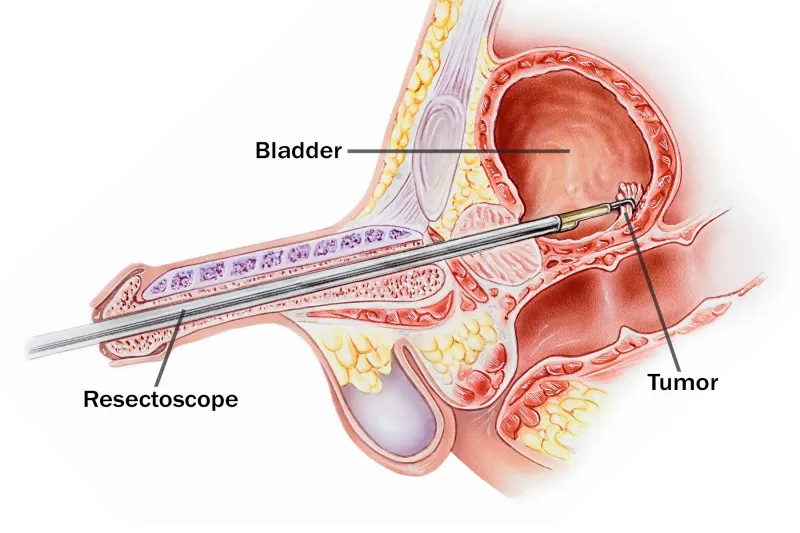
Cystoscopy reveals a solitary tumor in the bladder. Transurethral resection of the bladder tumor is performed. The tumor is 4 cm. Histologic evaluation shows invasion of the immediate epithelium of cells by a high-grade urothelial carcinoma without invasion of the underlying tissue or muscularis propria. Which of the following is the most appropriate next step in management?
- A. No further treatment is needed at this time
- B. Systemic combination chemotherapy
- C. Intravesical Bacille Calmette-Guérin (BCG) (Correct Answer)
- D. Bladder radiation
- E. Bladder-sparing partial cystectomy
Bladder cancer surgical management Explanation: ***Intravesical Bacille Calmette-Guérin (BCG)***
- The patient has a **high-grade urothelial carcinoma** that invaded the immediate epithelium but **not the muscularis propria**, classifying it as **non-muscle-invasive bladder cancer (NMIBC)**.
- **Intravesical BCG immunotherapy** is the gold standard for high-risk NMIBC, including high-grade tumors, to reduce recurrence and progression after transurethral resection of bladder tumor (TURBT).
*No further treatment is needed at this time*
- This option is incorrect because a **high-grade tumor** carries a significant risk of recurrence and progression if left untreated.
- Even after complete TURBT, adjuvant therapy is necessary for high-risk NMIBC to improve outcomes.
*Systemic combination chemotherapy*
- **Systemic chemotherapy** is generally reserved for **muscle-invasive or metastatic bladder cancer**, which is not the case here.
- For NMIBC, local intravesical therapy is preferred over systemic approaches due to lower systemic toxicity and effective local control.
*Bladder radiation*
- **Bladder radiation** is typically used in cases of **muscle-invasive bladder cancer** as an alternative to cystectomy for patients who are not surgical candidates or for bladder preservation protocols.
- It is not the standard primary adjuvant treatment for high-grade NMIBC.
*Bladder-sparing partial cystectomy*
- A **partial cystectomy** might be considered for a **solitary, localized muscle-invasive tumor** in a favorable location, or for very large, intractable high-grade NMIBC.
- However, for non-muscle-invasive disease that has been completely resected, **intravesical therapy** is the less invasive and equally effective first-line adjuvant treatment.
Bladder cancer surgical management US Medical PG Question 3: A 40-year-old man comes to the physician for a follow-up examination. He feels well. He has no urinary urgency, increased frequency, dysuria, or gross hematuria. He has a history of recurrent urinary tract infections. His last urinary tract infection was 3 months ago and was treated with ciprofloxacin. Current medications include a multivitamin. He has smoked one pack of cigarettes daily for 18 years. Vital signs are within normal limits. The abdomen is soft and nontender. There is no costovertebral angle tenderness. Laboratory studies show:
Hemoglobin 11.2 g/dL
Leukocyte count 9,500/mm3
Platelet count 170,000/mm3
Serum
Na+ 135 mEq/L
K+ 4.9 mEq/L
Cl- 101 mEq/L
Urea nitrogen 18 mg/dL
Creatinine 0.6 mg/dL
Urine
Blood 2+
Protein negative
RBC 5–7/hpf, normal shape and size
RBC casts negative
WBC 0–2/hpf
Bacteria negative
Urine cultures are negative. Urine analysis is repeated and shows similar results. A cystoscopy shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Annual urinalysis
- B. Reassurance
- C. CT urography (Correct Answer)
- D. Voided urine cytology
- E. Transrectal ultrasound
Bladder cancer surgical management Explanation: ***CT urography***
- The patient has **microscopic hematuria** with **2+ blood on urinalysis** and **5-7 RBCs/hpf**, in the absence of infection or other identifiable causes, which warrants further investigation for potential malignancy.
- Given the patient's **smoking history** (18 pack-years) and age, which are significant risk factors for **urothelial carcinoma** (bladder, renal pelvis, ureters), imaging with CT urography is crucial to visualize the entire urinary tract for tumors or other structural abnormalities.
*Annual urinalysis*
- This option represents a passive approach to monitoring, which is inadequate given the presence of **unexplained microscopic hematuria** and risk factors for malignancy.
- Delaying definitive investigation could lead to a missed or delayed diagnosis of a potentially treatable condition like **urothelial cancer**.
*Reassurance*
- Reassurance is inappropriate when **microscopic hematuria** is present without a clear benign cause, especially in a patient with risk factors like **smoking history**.
- This could lead to a false sense of security and delay the diagnosis and treatment of a serious underlying condition.
*Voided urine cytology*
- **Urine cytology** has a low sensitivity for detecting low-grade bladder cancers, though it can be useful for high-grade cancers and carcinoma in situ.
- While it may be considered in conjunction with imaging, it is not the most appropriate *initial* next step to identify the source of hematuria throughout the entire urinary tract, especially when imaging can detect other pathologies.
*Transrectal ultrasound*
- A **transrectal ultrasound** is primarily used to evaluate the **prostate gland**, typically in the context of prostate-specific antigen elevation or prostatic symptoms.
- It would not effectively visualize the bladder, ureters, or kidneys, which are the primary concerns for microscopic hematuria in this patient's demographic and risk factors.
Bladder cancer surgical management US Medical PG Question 4: Three hours after undergoing open proctocolectomy for ulcerative colitis, a 42-year-old male complains of abdominal pain. The pain is localized to the periumbilical and hypogastric regions. A total of 20 mL of urine has drained from his urinary catheter since the end of the procedure. Temperature is 37.2°C (98.9°F), pulse is 92/min, respirations are 12/min, and blood pressure is 110/72 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Physical examination shows a 20 cm vertical midline incision and an ileostomy in the right lower quadrant. There is no fluid drainage from the surgical wounds. The urinary catheter flushes easily and is without obstruction. Cardiopulmonary examination shows no abnormalities. Serum studies show a blood urea nitrogen of 30 mg/dL and a creatinine of 1.3 mg/dL. Which of the following is the most appropriate next step in management?
- A. Administer tamsulosin
- B. Administer intravenous furosemide
- C. Obtain an abdominal CT
- D. Start ciprofloxacin
- E. Administer intravenous fluids (Correct Answer)
Bladder cancer surgical management Explanation: ***Administer intravenous fluids***
- The patient's **oliguria** (20 mL urine over 3 hours, ~7 mL/hour) post-surgery, elevated **BUN (30 mg/dL)**, and **creatinine (1.3 mg/dL)** with a **BUN:Cr ratio >20:1** suggest **prerenal acute kidney injury** due to **hypovolemia**.
- Post-operative fluid losses from **third-spacing**, blood loss, and insensible losses commonly cause hypovolemia after major abdominal surgery.
- **Intravenous fluids** are the most appropriate initial step to restore intravascular volume and improve renal perfusion.
*Administer tamsulosin*
- **Tamsulosin** is an alpha-blocker used to relax smooth muscle in the prostate and bladder neck, primarily for **urinary retention** due to benign prostatic hyperplasia.
- This patient's oliguria is due to **prerenal azotemia** from hypovolemia, not prostatic obstruction, and the catheter flushes easily without obstruction.
*Administer intravenous furosemide*
- **Furosemide** is a loop diuretic that increases urine output, but administering it in the context of **prerenal acute kidney injury** can worsen hypovolemia and further compromise renal function.
- Diuretics are generally contraindicated in oliguria due to hypovolemia and should only be considered after volume resuscitation.
*Obtain an abdominal CT*
- While an abdominal CT can diagnose surgical complications, there are no immediate signs of a surgical emergency like **anastomotic leak** or **bowel obstruction**.
- Addressing the likely **hypovolemia** is more urgent and should precede further imaging in this scenario.
*Start ciprofloxacin*
- The patient does not show signs of infection, such as fever or localized signs of bacterial peritonitis, making **antibiotics** like ciprofloxacin inappropriate as the initial management step.
- The elevated BUN and creatinine are more indicative of volume depletion than infection.
Bladder cancer surgical management US Medical PG Question 5: Four hours after undergoing an abdominal hysterectomy, a 43-year-old woman is evaluated in the post-anesthesia care unit because she has only had a urine output of 5 mL of blue-tinged urine since surgery. The operation went smoothly and ureter patency was checked via retrograde injection of methylene blue dye mixed with saline through the Foley catheter. She received 2.4 L of crystalloid fluids intraoperatively and urine output was 1.2 L. She had a history of fibroids with painful and heavy menses. She is otherwise healthy. She underwent 2 cesarean sections 8 and 5 years ago, respectively. Her temperature is 37.4°C (99.3°F), pulse is 75/min, respirations are 16/min, and blood pressure is 122/76 mm Hg. She appears comfortable. Cardiopulmonary examination shows no abnormalities. There is a midline surgical incision with clean and dry dressings. Her abdomen is soft and mildly distended in the lower quadrants. Her bladder is slightly palpable. Extremities are warm and well perfused, and capillary refill is brisk. Laboratory studies show:
Leukocyte count 8,300/mm3
Hemoglobin 10.3 g/dL
Hematocrit 31%
Platelet count 250,000/mm3
Serum
_Na+ 140 mEq/L
_K+ 4.2 mEq/L
_HCO3+ 26 mEq/L
_Urea nitrogen 26 mg/dL
_Creatinine 1.0 mg/dL
Urine
_Blood 1+
_WBC none
_Protein negative
_RBC none
_RBC casts none
A bladder scan shows 250 mL of retained urine. Which of the following is the next best step in the evaluation of this patient?
- A. Check the Foley catheter (Correct Answer)
- B. Return to the operating room for emergency surgery
- C. Perform ultrasound of the kidneys
- D. Administer 20 mg of IV furosemide
- E. Administer bolus 500 mL of Lactated Ringers
Bladder cancer surgical management Explanation: ***Check the Foley catheter***
- This patient presents with signs of **urinary retention** (low urine output, palpable bladder, retained urine on bladder scan) despite methylene blue injection confirming ureter patency. The most common and easily reversible cause of low urine output post-hysterectomy is a **kinked or obstructed Foley catheter**.
- Given the smooth intraoperative course and adequate urine output during surgery, a quick check and potential **repositioning or flushing of the catheter** is the immediate and most appropriate first step before considering more invasive interventions.
*Return to the operating room for emergency surgery*
- This is a drastic step and is not indicated at this stage. There is no evidence of a **surgical complication** requiring emergency intervention, such as a ureteral injury (which was checked intraoperatively) or active hemorrhage.
- The patient's vital signs are stable, and she appears comfortable, which makes an emergency surgical re-exploration highly unlikely as the initial best step.
*Perform ultrasound of the kidneys*
- While a renal ultrasound can assess for **hydronephrosis** or other kidney abnormalities, it is a delayed step. Given the clear evidence of bladder retention and the possibility of a simple catheter malfunction, performing an ultrasound without first addressing the catheter would be premature.
- The patient's **creatinine is normal**, making acute kidney injury due to obstruction less likely as an immediate concern.
*Administer 20 mg of IV furosemide*
- Furosemide is a **loop diuretic** that increases urine production. However, it would be ineffective and potentially harmful if the issue is a mechanical obstruction of urine outflow, as appears to be the case here.
- Administering a diuretic without addressing the outflow problem would only worsen bladder distension and potentially stress the renal system without resolving the underlying issue.
*Administer bolus 500 mL of Lactated Ringers*
- This patient has already received 2.4 L of crystalloid fluids intraoperatively and has stable vital signs, indicating she is likely **euvolemic**.
- Giving another fluid bolus would not address the observed urinary retention and could lead to **fluid overload** if the urine outflow obstruction persists.
Bladder cancer surgical management US Medical PG Question 6: Six hours after near-total thyroidectomy for Graves disease, a 58-year-old man has not had any urine output. The surgery was successful and the patient feels well except for slight neck pain. He has type 2 diabetes mellitus and hypertension. His father had autosomal dominant polycystic kidney disease. Prior to the surgery, the patient was taking metformin and lisinopril regularly and ibuprofen as needed for headaches. His current medications include acetaminophen and codeine. His temperature is 36.2°C (97.2°F), pulse is 82/min, and blood pressure is 122/66 mm Hg. Physical examination shows a 7-cm surgical wound on the anterior neck with mild swelling, but no reddening or warmth. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain renal scintigraphy
- B. Perform bedside bladder scan (Correct Answer)
- C. Administer furosemide
- D. Obtain urinalysis
- E. Obtain renal biopsy
Bladder cancer surgical management Explanation: **Perform bedside bladder scan**
- The absence of urine output post-surgery is concerning for **urinary retention**, especially given the recent surgery and pain medication use. A bedside bladder scan is the quickest and least invasive way to confirm significant bladder distension.
- Postoperative urinary retention can be caused by various factors, including the effects of anesthesia, pain, immobility, and certain medications like opioids, which the patient is currently receiving (codeine).
*Obtain renal scintigraphy*
- **Renal scintigraphy** is used to assess kidney function and blood flow, but it is not the initial test for acute anuria or oligoanuria in the immediate postoperative period.
- This test would be more appropriate if there was suspicion of a vascular compromise to the kidneys or an intrinsic kidney problem, which is not the most likely cause of acute anuria in this clinical context.
*Administer furosemide*
- Administering a loop diuretic like **furosemide** without knowing if the patient has obstructive uropathy or hypovolemia could be harmful.
- If the patient has urinary retention, furosemide would be ineffective and could potentially worsen dehydration if the anuria is due to severe hypovolemia.
*Obtain urinalysis*
- A **urinalysis** evaluates urine sediment and chemical properties, which would be useful for diagnosing intrinsic kidney disease, infection, or nephrolithiasis.
- However, with complete anuria (no urine output), there is no urine to analyze, making this step impractical and unhelpful in determining the immediate cause of no urine output.
*Obtain renal biopsy*
- A **renal biopsy** is an invasive procedure used to diagnose intrinsic kidney diseases. It carries risks and is not an appropriate initial step for acute anuria after surgery.
- It would only be considered if less invasive tests pinpointed a specific intrinsic renal pathology requiring tissue diagnosis, which is far down the diagnostic algorithm for acute anuria.
Bladder cancer surgical management US Medical PG Question 7: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Bladder cancer surgical management Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
Bladder cancer surgical management US Medical PG Question 8: A 63-year-old female with known breast cancer presents with progressive motor weakness in bilateral lower extremities and difficulty ambulating. Physical exam shows 4 of 5 motor strength in her legs and hyper-reflexia in her patellar tendons. Neurologic examination 2 weeks prior was normal. Imaging studies, including an MRI, show significant spinal cord compression by the metastatic lesion and complete erosion of the T12 vertebrae. She has no metastatic disease to the visceral organs and her oncologist reports her life expectancy to be greater than one year. What is the most appropriate treatment?
- A. Palliative pain management consultation
- B. Surgical decompression and postoperative radiotherapy (Correct Answer)
- C. High-dose corticosteroids and clinical observation
- D. Radiation therapy alone
- E. Chemotherapy alone
Bladder cancer surgical management Explanation: ***Surgical decompression and postoperative radiotherapy***
- There is **spinal cord compression** by a metastatic lesion in a patient with a good prognosis (>1 year life expectancy) and rapidly progressive neurological deficits. **Surgical decompression** offers immediate relief of compression, while **postoperative radiotherapy** helps local tumor control.
- This combined approach is superior in preserving neurological function and improving quality of life for patients with **epidural spinal cord compression (ESCC)** in this clinical context.
*Palliative pain management consultation*
- While pain management is important in cancer care, this option alone does not address the **progressive neurological deficits** due to spinal cord compression.
- This patient's condition requires active treatment to prevent further neurological compromise and is not solely focused on comfort measures at this stage given her prognosis.
*Spinal dose corticosteroids and clinical observation*
- **Corticosteroids** can temporarily reduce edema around the spinal cord, but they do not resolve the mechanical compression caused by the eroded T12 vertebrae.
- **Clinical observation** without definitive intervention risks irreversible neurological damage given the rapid progression of symptoms.
*Radiation therapy alone*
- While radiation therapy is effective for local tumor control, it may not provide **rapid enough decompression** for acute or rapidly progressing neurological deficits due to significant mechanical compression.
- In cases of severe compression, such as bone erosion and cord involvement, surgery is usually needed prior to or in combination with radiation.
*Chemotherapy alone*
- **Chemotherapy** for breast cancer is a systemic treatment and may take time to reduce tumor burden, which is not suitable for urgent relief of **spinal cord compression**.
- It does not provide immediate mechanical decompression and is generally not the primary treatment for acute ESCC, especially with bone involvement.
Bladder cancer surgical management US Medical PG Question 9: A 70-year-old man with metastatic castration-resistant prostate cancer presents to the emergency department with severe back pain, bilateral lower extremity weakness (3/5 strength), and urinary retention that started 8 hours ago. He has known bone metastases and his PSA has been rising despite androgen deprivation therapy. MRI spine shows an epidural mass at T10 with severe spinal cord compression and near-complete canal obliteration. He is neurologically intact above T10. Radiation oncology, neurosurgery, and medical oncology are consulted. Evaluate the optimal management approach.
- A. Corticosteroids, radiation therapy, and switch to next-line systemic therapy
- B. Stereotactic radiosurgery as single-modality treatment
- C. Emergent surgical decompression followed by radiation therapy (Correct Answer)
- D. Palliative care consultation and comfort measures only given metastatic disease
- E. High-dose corticosteroids and emergent radiation therapy alone
Bladder cancer surgical management Explanation: ***Emergent surgical decompression followed by radiation therapy***
- For patients with **malignant spinal cord compression (MSCC)** and acute neurologic deficits lasting <48 hours, **decompressive surgery** followed by radiotherapy results in better ambulatory outcomes than radiation alone.
- This patient has a **single level of compression** (T10) and a reasonable functional status above the lesion, making him an ideal candidate for surgery to preserve **quality of life**.
*Corticosteroids, radiation therapy, and switch to next-line systemic therapy*
- While **systemic therapy** is important for managing metastatic disease, it does not address the acute **mechanical compression** currently threatening spinal cord viability.
- Postponing definitive mechanical decompression in favor of systemic treatment would likely result in **permanent paraplegia** given the severe canal obliteration.
*Stereotactic radiosurgery as single-modality treatment*
- **Stereotactic radiosurgery (SRS)** is effective for spinal metastases but is generally not the primary choice when there is **high-grade spinal cord compression** with an associated neurologic deficit.
- Surgery is needed first to provide immediate **mechanical decompression** and create a "separation" distance between the cord and the tumor for safer high-dose radiation.
*Palliative care consultation and comfort measures only given metastatic disease*
- Although the cancer is metastatic, preserving **ambulatory function** and bladder control is a priority for maintaining dignity and independence.
- **MSCC** is an oncologic emergency where intervention is indicated unless the patient's **life expectancy** is very short (typically <3 months), which is not clearly the case here.
*High-dose corticosteroids and emergent radiation therapy alone*
- Radiation therapy alone is typically reserved for patients who are not **surgical candidates**, have multisegmental disease, or have complete paralysis for >48 hours.
- **Direct decompressive surgery** is superior for restoring and maintaining the ability to walk in patients with acute, unstable neurologic symptoms from a **single-level mass**.
Bladder cancer surgical management US Medical PG Question 10: A 3-year-old boy is brought to the clinic for evaluation of an undescended left testicle noted since birth. The right testicle is in normal scrotal position. On examination, the left testicle is palpable in the inguinal canal and can be manipulated to the upper scrotum but retracts immediately upon release. The testicle appears smaller than the contralateral side. The parents report they were told to wait and see if it descends spontaneously. What is the most appropriate management at this time?
- A. Immediate orchiopexy given the patient's age (Correct Answer)
- B. Reassurance and follow-up at age 5 years before school entry
- C. Continue observation as the testicle is palpable and may still descend
- D. Orchiectomy given the size discrepancy and malignancy risk
- E. Hormonal therapy with hCG to stimulate testicular descent
Bladder cancer surgical management Explanation: ***Immediate orchiopexy given the patient's age***
- Spontaneous descent is highly unlikely after **6 months of age**; surgery is recommended as early as possible after this window to improve **fertility** and facilitate **cancer screening**.
- This patient is **3 years old**, which is well past the recommended management window of **6 to 18 months**, necessitating prompt surgical intervention.
*Continue observation as the testicle is palpable and may still descend*
- Spontaneous descent of a cryptorchid testis rarely occurs after **age 6 months**, making ongoing observation clinically inappropriate.
- Delayed treatment increases the risk of **testicular atrophy**, **germ cell loss**, and potentially **malignant transformation**.
*Hormonal therapy with hCG to stimulate testicular descent*
- **Hormonal therapy** (e.g., hCG or GnRH) is generally not recommended in the US due to poor **long-term efficacy** compared to surgery.
- The success rate of hormonal therapy is notably low for truly **cryptorchid** testes and does not replace the gold standard of **orchiopexy**.
*Reassurance and follow-up at age 5 years before school entry*
- Waiting until age 5 is inappropriate as it significantly increases the risk of **infertility** and **testicular germ cell tumors**.
- The diagnosis of a **retractile testis** (which might be observed) is ruled out here because the testis **retracts immediately** and is smaller than the contralateral side.
*Orchiectomy given the size discrepancy and malignancy risk*
- **Orchiectomy** (removal) is generally reserved for **post-pubertal males** or instances where the testis is found to be **non-viable** or severely dysgenetic during surgery.
- In a **3-year-old**, the primary goal is **orchiopexy** to preserve hormonal function and provide a chance for future fertility.
More Bladder cancer surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.