Traumatic shock management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Traumatic shock management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Traumatic shock management US Medical PG Question 1: A 45-year-old man was a driver in a motor vehicle collision. The patient is not able to offer a medical history during initial presentation. His temperature is 97.6°F (36.4°C), blood pressure is 104/74 mmHg, pulse is 150/min, respirations are 12/min, and oxygen saturation is 98% on room air. On exam, he does not open his eyes, he withdraws to pain, and he makes incomprehensible sounds. He has obvious signs of trauma to the chest and abdomen. His abdomen is distended and markedly tender to palpation. He also has an obvious open deformity of the left femur. What is the best initial step in management?
- A. Emergency open fracture repair
- B. Packed red blood cells
- C. Exploratory laparotomy
- D. Intubation (Correct Answer)
- E. 100% oxygen
Traumatic shock management Explanation: ***Intubation***
- The patient's **Glasgow Coma Scale (GCS) score is 7** (E=1, V=2, M=4), which is below 8 and indicates a severe head injury needing **airway protection** via intubation.
- A GCS ≤ 8 mandates **definitive airway management** to prevent aspiration and ensure adequate ventilation.
*Emergency open fracture repair*
- While the patient has an open femur fracture, it is not the most immediate life-threatening concern after a major trauma; **airway and breathing** take precedence.
- **Hemorrhage control** and **stabilization** often precede definitive orthopedic repair in polytrauma.
*Packed red blood cells*
- Although the patient is likely in **hemorrhagic shock** (tachycardia, hypotension, obvious trauma), administering blood products without first securing the airway is not the initial priority.
- **Circulation** management, including fluid resuscitation and blood products, follows **airway and breathing** establishment.
*Exploratory laparotomy*
- The patient's distended and tender abdomen strongly suggests intra-abdominal injury, but this is a **diagnostic and therapeutic procedure** that comes after initial resuscitation and stabilization.
- **Emergent laparotomy** for abdominal trauma is considered once the patient's airway, breathing, and circulation are secured.
*100% oxygen*
- Administering 100% oxygen is part of initial resuscitation, but it does not address the fundamental problem of an unsecured airway and the risk of **hypoventilation** or **aspiration** in a patient with a GCS of 7.
- Oxygen supplementation helps improve saturation in spontaneously breathing patients but cannot protect a compromised airway.
Traumatic shock management US Medical PG Question 2: A 35-year-old patient is brought into the emergency department post motor vehicle crash. Stabilization of the patient in the trauma bay requires endotracheal intubation. The patient has a laceration on the femoral artery from shrapnel and seems to have lost large quantities of blood. The patient is transfused with 13 units of packed red blood cells. His vitals are T 96.5, HR 150, BP 90/40. Even with the direct pressure on the femoral artery, the patient continues to bleed. Results of labs drawn within the last hour are pending. Which of the following is most likely to stop the bleeding in this patient?
- A. Normal saline
- B. Fresh frozen plasma and platelets (Correct Answer)
- C. Whole blood
- D. Dextrose
- E. Cryoprecipitate
Traumatic shock management Explanation: ***Fresh frozen plasma and platelets***
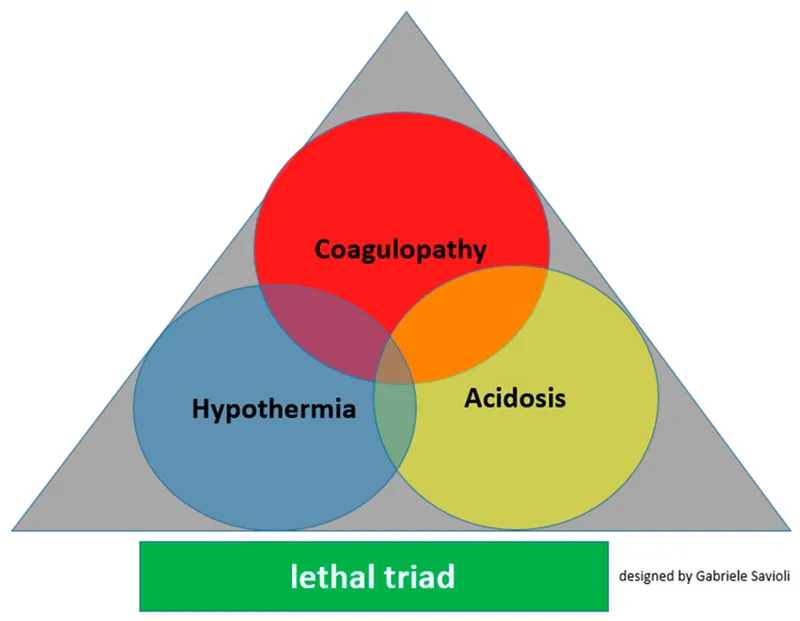
- This patient is experiencing **dilutional coagulopathy** due to massive transfusion of packed red blood cells, which lack clotting factors and platelets.
- **Fresh frozen plasma (FFP)** provides essential clotting factors, while **platelets** directly address thrombocytopenia, both crucial for **hemostasis**.
- This represents **standard component therapy** readily available in emergency departments.
*Normal saline*
- Administering normal saline would further dilute the remaining clotting factors and platelets, potentially **worsening the coagulopathy**.
- While essential for **volume resuscitation**, it does not provide any clotting components needed to stop bleeding.
*Whole blood*
- While **whole blood** contains red blood cells, plasma, and platelets in physiologic ratios, it is **not readily available** in most civilian trauma centers.
- Modern practice uses **component therapy** (FFP + platelets + PRBCs) which is more widely accessible and allows for targeted resuscitation.
- Low-titer O whole blood programs exist in some centers but are not universally available.
*Dextrose*
- **Dextrose solutions** primarily provide free water and glucose, used for hydration and hypoglycemia.
- It has **no hemostatic properties** and would further dilute clotting factors, exacerbating the bleeding.
*Cryoprecipitate*
- **Cryoprecipitate** is rich in **fibrinogen, factor VIII, factor XIII, and von Willebrand factor**.
- While useful for specific factor deficiencies or when fibrinogen is critically low in massive transfusions, it **does not replace all clotting factors or platelets** comprehensively as FFP and platelets would.
- Typically used as **adjunctive therapy** when fibrinogen levels are known to be low.
Traumatic shock management US Medical PG Question 3: A 35-year-old woman with no significant past medical history is brought in by ambulance after a major motor vehicle collision. Temperature is 97.8 deg F (36.5 deg C), blood pressure is 76/40, pulse is 110/min, and respirations are 12/min. She arouses to painful stimuli and makes incomprehensible sounds, but is unable to answer questions. Her abdomen is distended and diffusely tender to palpation. Bedside ultrasound shows blood in the peritoneal cavity. Her husband rushes to the bedside and states she is a Jehovah’s Witness and will refuse blood products. No documentation of blood refusal is available for the patient. What is the most appropriate next step in management?
- A. In accordance with the husband's wishes, do not transfuse any blood products
- B. Observe and reassess mental status in an hour to see if patient can consent for herself
- C. Attempt to contact the patient’s parents for additional collateral information
- D. Consult the hospital ethics committee
- E. Administer blood products (Correct Answer)
Traumatic shock management Explanation: **Administer blood products**
- In emergency situations where a patient is incapacitated and there is no **advance directive** or **legal proxy** explicitly refusing treatment, the principle of **presumed consent** applies, allowing life-saving interventions.
- The patient's husband's statement is not legally binding without a living will or medical power of attorney, especially when the patient's capacity to consent or refuse treatment is compromised due to critical injury.
*In accordance with the husband's wishes, do not transfuse any blood products*
- The husband's stated wishes are not legally sufficient to refuse life-saving treatment for an incapacitated adult unless he holds **durable power of attorney for health care** specifically outlining these wishes, which is not stated here.
- Deferring necessary treatment based solely on the husband's assertion could lead to the patient's death and potentially expose the medical team to **malpractice liability**.
*Observe and reassess mental status in an hour to see if patient can consent for herself*
- The patient presents with **severe hypovolemic shock** (BP 76/40, HR 110/min) and signs of significant hemorrhage, indicating an urgent, life-threatening situation.
- Delaying emergent treatment to wait for a change in mental status would likely result in irreversible harm or death, as her condition is rapidly deteriorating.
*Attempt to contact the patient’s parents for additional collateral information*
- Contacting other family members for more information would cause a **critical delay** in a life-threatening situation.
- Even if parents confirm the patient's faith, their input is still not a legally binding refusal of treatment without proper documentation or court order.
*Consult the hospital ethics committee*
- Ethics committee consultations are appropriate for complex ethical dilemmas that are not immediately life-threatening or when there is sufficient time for deliberation.
- In this **critical emergency** with an actively hemorrhaging patient in shock, consulting the ethics committee would cause an unacceptable delay in life-saving treatment.
Traumatic shock management US Medical PG Question 4: A 57-year-old man is admitted to the burn unit after he was brought to the emergency room following an accidental fire in his house. His past medical history is unknown due to his current clinical condition. Currently, his blood pressure is 75/40 mmHg, pulse rate is 140/min, and respiratory rate is 17/min. The patient is subsequently intubated and started on aggressive fluid resuscitation. A Swan-Ganz catheter is inserted to clarify his volume status. Which of the following hemodynamic parameters would you expect to see in this patient?
- A. Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
- B. Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔
- C. Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔
- D. Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓ (Correct Answer)
- E. Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
Traumatic shock management Explanation: ***Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓***
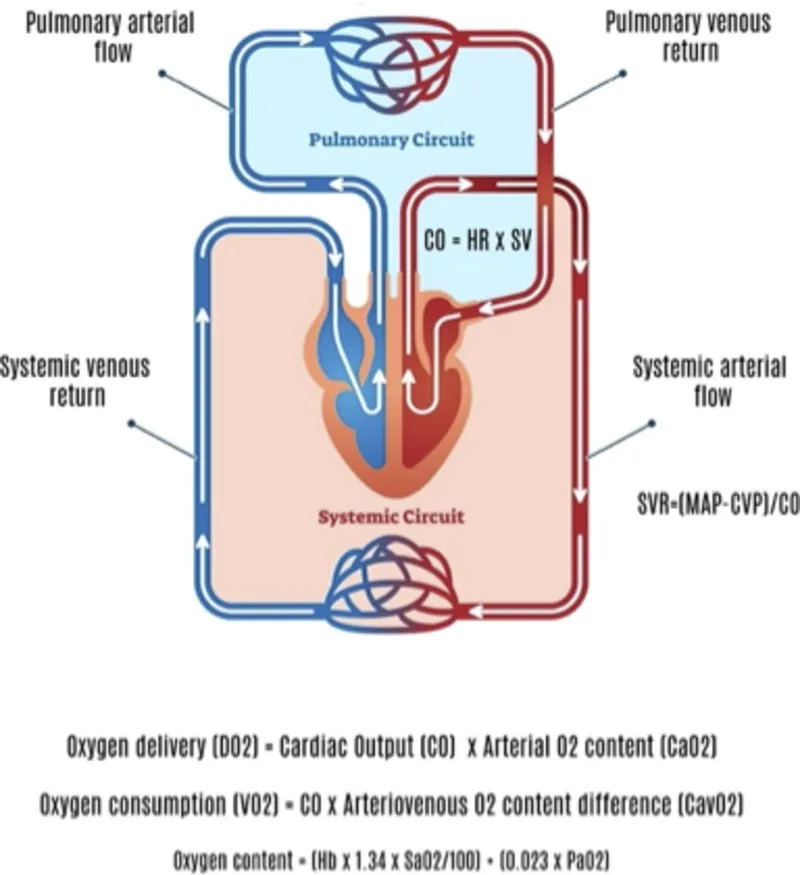
- The patient's **hypotension (75/40 mmHg)** and **tachycardia (140/min)**, combined with severe burns, indicate **hypovolemic shock** due to massive fluid loss from damaged capillaries.
- In response to decreased cardiac output and hypovolemia, the body compensates by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, and **pulmonary artery wedge pressure (PAWP)** will be low due to reduced intravascular volume.
*Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This option incorrectly suggests that systemic vascular resistance and pulmonary artery wedge pressure would be normal, which is inconsistent with **hypovolemic shock**.
- In shock, the body's compensatory mechanisms would lead to significant changes in SVR and PAWP, not maintain them at baseline.
*Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔*
- Increased cardiac output is usually seen in **distributive shock** (e.g., septic shock) where vasodilation leads to reduced SVR, not increased SVR as suggested here.
- An elevated SVR coupled with an increased cardiac output would typically result in a higher blood pressure unless there is a compensatory drop in other parameters.
*Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔*
- This pattern (high cardiac output, low SVR) is characteristic of **distributive shock**, such as **septic shock** or anaphylactic shock, rather than the hypovolemic shock expected in a burn patient.
- Severe burns primarily cause massive fluid shifts, leading to hypovolemia and a reduced cardiac output, not an elevated one.
*Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This scenario represents **normal hemodynamic parameters**, which would not be expected in a patient experiencing severe shock from extensive burns.
- The patient's clinical presentation (hypotension, tachycardia) clearly indicates a state of hemodynamic instability.
Traumatic shock management US Medical PG Question 5: A 34-year-old male is brought to the emergency department by fire and rescue following a motor vehicle accident in which the patient was an unrestrained driver. The paramedics report that the patient was struck from behind by a drunk driver. He was mentating well at the scene but complained of pain in his abdomen. The patient has no known past medical history. In the trauma bay, his temperature is 98.9°F (37.2°C), blood pressure is 86/51 mmHg, pulse is 138/min, and respirations are 18/min. The patient is somnolent but arousable to voice and pain. His lungs are clear to auscultation bilaterally. He is diffusely tender to palpation on abdominal exam with bruising over the left upper abdomen. His distal pulses are thready, and capillary refill is delayed bilaterally. Two large-bore peripheral intravenous lines are placed to bolus him with intravenous 0.9% saline. Chest radiograph shows multiple left lower rib fractures.
Which of the following parameters is most likely to be seen in this patient?
- A. Increased cardiac output
- B. Increased mixed venous oxygen saturation
- C. Decreased pulmonary capillary wedge pressure (Correct Answer)
- D. Decreased systemic vascular resistance
- E. Increased right atrial pressure
Traumatic shock management Explanation: ***Decreased pulmonary capillary wedge pressure***
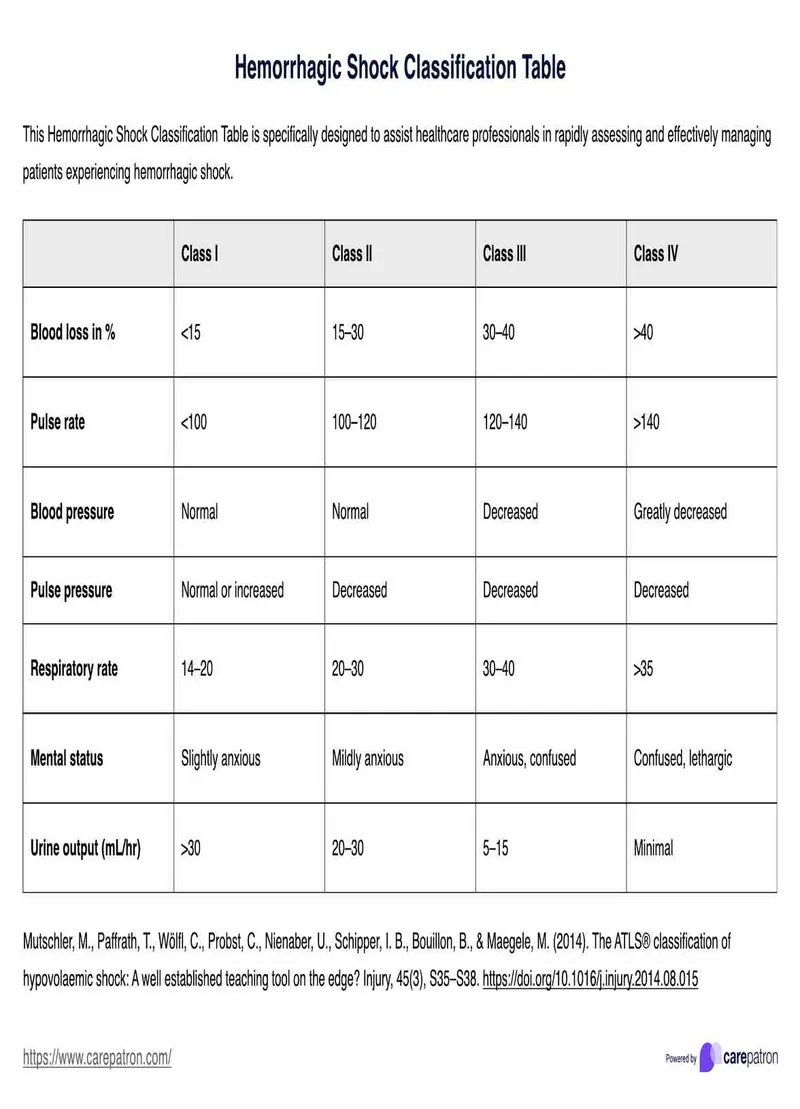
- The patient presents with classic signs of **hemorrhagic shock** (hypotension, tachycardia, somnolence, abdominal bruising, thready pulses) due to trauma, likely involving the spleen or kidney given the left upper abdominal bruising and rib fractures.
- **Decreased pulmonary capillary wedge pressure (PCWP)** is expected in hypovolemic shock because it reflects left atrial and left ventricular end-diastolic pressure, which will be low due to reduced venous return and intravascular volume.
*Increased cardiac output*
- In **hemorrhagic shock**, the body attempts to compensate by increasing heart rate, but overall **cardiac output is typically decreased** due to profound reduction in preload (venous return) from blood loss.
- While heart rate is elevated, the stroke volume is severely diminished, leading to a net decrease in cardiac output despite compensatory efforts.
*Increased mixed venous oxygen saturation*
- **Mixed venous oxygen saturation (SvO2)** is generally **decreased in hemorrhagic shock** due to increased oxygen extraction by tissues.
- Inadequate oxygen delivery to the tissues forces them to extract more oxygen from the blood, leading to a lower SvO2.
*Decreased systemic vascular resistance*
- In **hemorrhagic shock**, the body activates compensatory mechanisms, including generalized **vasoconstriction**, to maintain blood pressure and prioritize blood flow to vital organs.
- This leads to an **increased systemic vascular resistance (SVR)**, not decreased, as reflected by the thready distal pulses and delayed capillary refill.
*Increased right atrial pressure*
- **Right atrial pressure (RAP)**, representing CVP, is typically **decreased in hemorrhagic shock** due to reduced circulating blood volume.
- A lower RAP indicates decreased venous return to the heart, a hallmark of hypovolemia.
Traumatic shock management US Medical PG Question 6: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Traumatic shock management Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Traumatic shock management US Medical PG Question 7: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Traumatic shock management Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Traumatic shock management US Medical PG Question 8: A 65-year-old man presents to the emergency department by ambulance following a motor vehicle accident. He was a restrained passenger. At the hospital, he is bleeding heavily from a large wound in his left leg. A review of medical records reveals a history of atrial fibrillation for which he takes warfarin. His international normalized ratio (INR) 2 days ago was 2.6. On physical exam he is cool and clammy. The vital signs include: heart rate 130/min and blood pressure 96/54 mm Hg. Aggressive resuscitation with intravenous normal saline is begun. Which of the following is the next best step to correct this patient's underlying coagulopathy?
- A. Give platelets
- B. Give intravenous vitamin K
- C. Give fresh frozen plasma (FFP) (Correct Answer)
- D. Give cryoprecipitate
- E. Give packed red blood cells
Traumatic shock management Explanation: ***Give fresh frozen plasma (FFP)***
- This patient is in **hemorrhagic shock** due to severe bleeding while on **warfarin**, evidenced by tachycardia (HR 130), hypotension (BP 96/54), and cool/clammy skin with an INR of 2.6.
- **Fresh frozen plasma (FFP)** contains all vitamin K-dependent clotting factors (II, VII, IX, X) and is the best option **among those listed** to immediately reverse warfarin's effects in this life-threatening hemorrhage.
- FFP provides rapid reversal within minutes to hours, though it requires large volumes (10-15 mL/kg) and carries risk of transfusion-associated circulatory overload (TACO).
- **Note:** In modern practice, **4-factor prothrombin complex concentrate (PCC)** is preferred over FFP for warfarin reversal (faster, smaller volume, fewer complications), but it is not listed among the options here.
*Give intravenous vitamin K*
- **Vitamin K** reverses warfarin by enabling synthesis of vitamin K-dependent clotting factors (II, VII, IX, X).
- However, it takes **6-24 hours** to produce clinical effect, making it unsuitable as monotherapy for **life-threatening acute bleeding**.
- Vitamin K should be given as **adjunct therapy** alongside FFP, but cannot be the sole intervention in hemorrhagic shock.
*Give platelets*
- **Platelets** are indicated for **thrombocytopenia** (typically <50,000 in active bleeding) or **platelet dysfunction**.
- Warfarin affects **clotting factors**, not platelet count or function, so platelets will not reverse the coagulopathy.
- No indication of thrombocytopenia is mentioned in this case.
*Give cryoprecipitate*
- **Cryoprecipitate** contains **fibrinogen, Factor VIII, Factor XIII, von Willebrand factor, and fibronectin**.
- It does **not contain** the vitamin K-dependent factors (II, VII, IX, X) depleted by warfarin.
- Cryoprecipitate is used for **hypofibrinogenemia** (fibrinogen <100 mg/dL) in massive transfusion or DIC, not for warfarin reversal.
*Give packed red blood cells*
- **Packed red blood cells (PRBCs)** replace blood volume and improve oxygen-carrying capacity in hemorrhagic shock.
- While PRBCs are critical for managing hypovolemia, they **do not contain clotting factors** and will not correct the **warfarin-induced coagulopathy**.
- PRBCs should be transfused in this patient, but they must be combined with FFP to address the underlying bleeding disorder.
Traumatic shock management US Medical PG Question 9: A 45-year-old man is brought to the trauma bay by emergency services after a motorbike accident in which the patient, who was not wearing a helmet, hit a pole of a streetlight with his head. When initially evaluated by the paramedics, the patient was responsive, albeit confused, opened his eyes spontaneously, and was able to follow commands. An hour later, upon admission, the patient only opened his eyes to painful stimuli, made incomprehensible sounds, and assumed a flexed posture. The vital signs are as follows: blood pressure 140/80 mm Hg; heart rate 59/min; respiratory rate 11/min; temperature 37.0℃ (99.1℉), and SaO2, 95% on room air. The examination shows a laceration and bruising on the left side of the head. There is anisocoria with the left pupil 3 mm more dilated than the right. Both pupils react sluggishly to light. There is an increase in tone and hyperreflexia in the right upper and lower extremities. The patient is intubated and mechanically ventilated, head elevated to 30°, and sent for a CT scan. Which of the following management strategies should be used in this patient, considering his most probable diagnosis?
- A. Middle meningeal artery embolization
- B. Ventricular drainage
- C. Surgical evacuation (Correct Answer)
- D. Decompressive craniectomy
- E. Conservative management with hyperosmolar solutions
Traumatic shock management Explanation: ***Surgical evacuation***
- This patient presents with a classic picture of **epidural hematoma** (EDH) with signs of herniation, indicated by the rapid neurological decline, **anisocoria**, and contralateral motor deficits. **Urgent surgical evacuation** is the definitive treatment for EDH to relieve mass effect.
- The rapid progression from responsive to severely neurologically compromised, coupled with a history of head trauma and a potential lucid interval, points to an expanding intracranial lesion requiring immediate decompression.
*Middle meningeal artery embolization*
- While the **middle meningeal artery** is often the source of bleeding in EDH, embolization is typically reserved for cases where surgery is contraindicated or as an adjunct for persistent bleeding, not as a primary definitive treatment in an unstable patient.
- It does not immediately relieve the mass effect from a large, established hematoma, which is the acute life-threatening issue.
*Ventricular drainage*
- **Ventricular drainage** is primarily used to reduce **intracranial pressure** (ICP) in cases of **hydrocephalus** or intraventricular hemorrhage.
- It is not the primary treatment for an epidural hematoma, which is an extra-axial collection of blood.
*Decompressive craniectomy*
- **Decompressive craniectomy** involves removing a portion of the skull to allow the brain to swell and reduce ICP, often used in cases of diffuse brain injury and intractable ICP elevation refractory to other measures.
- In cases of an epidural hematoma with a treatable mass, **direct evacuation of the hematoma** and closure is preferred over decompressive craniectomy alone, although craniectomy might be needed if there's underlying brain swelling.
*Conservative management with hyperosmolar solutions*
- **Hyperosmolar solutions** (like mannitol or hypertonic saline) can acutely reduce ICP by drawing fluid from the brain, but they are a temporizing measure.
- They are used to manage ICP while preparing for definitive treatment or in diffuse brain injury, not as a primary treatment for a large, surgically accessible mass lesion causing rapid deterioration and herniation.
Traumatic shock management US Medical PG Question 10: A 35-year-old man is brought to the emergency department 20 minutes after being involved in a motor vehicle collision in which he was a restrained passenger. The patient is confused. His pulse is 140/min and blood pressure is 85/60 mm Hg. Examination shows a hand-sized hematoma on the anterior chest wall. An ECG shows sinus tachycardia. Which of the following structures is most likely injured in this patient?
- A. Papillary muscle
- B. Left main coronary artery
- C. Inferior vena cava
- D. Aortic isthmus (Correct Answer)
- E. Aortic valve
Traumatic shock management Explanation: ***Aortic isthmus***
- The **aortic isthmus** is the most common site of blunt **aortic injury** due to its relative immobility compared to the more mobile ascending aorta and arch. The deceleration forces experienced in a motor vehicle collision can cause a shearing injury at this location.
- The patient's **hypotension** and **tachycardia** are signs of significant hemorrhage, which is a common presentation of aortic injury. The chest wall hematoma also suggests significant trauma to the chest.
*Papillary muscle*
- Injury to the **papillary muscles** typically leads to severe **mitral regurgitation**, presenting with acute heart failure symptoms like pulmonary edema rather than primarily hypovolemic shock.
- While possible in trauma, the primary symptoms would involve a new significant murmur and rapid deterioration of cardiac function due to valve incompetence.
*Left main coronary artery*
- A **left main coronary artery** injury would likely lead to acute **myocardial ischemia** or infarction, manifesting as severe chest pain, ECG changes indicative of ischemia, and potentially cardiogenic shock, not hypovolemic shock.
- While trauma to the chest can cause coronary artery dissection, it is less common for blunt force to directly injure this artery without other, more widespread myocardial damage.
*Inferior vena cava*
- An injury to the **inferior vena cava (IVC)** would primarily cause severe internal bleeding, leading to hypovolemic shock. However, while possible, blunt force trauma to the chest is less likely to directly injure the retroperitoneal IVC without significant associated abdominal or lumbar spine injuries.
- The chest wall hematoma and focus on the chest suggests damage within the thoracic cavity, making an aortic injury more probable given the mechanism.
*Aortic valve*
- An injury to the **aortic valve** could cause acute **aortic regurgitation**, leading to acute heart failure and potentially cardiogenic shock with a new diastolic murmur.
- While possible, pure aortic valve injury from blunt trauma alone, without rupture of the aorta itself, is less common than aortic tear from shearing forces.
More Traumatic shock management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.