Trauma in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trauma in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Trauma in pregnancy US Medical PG Question 1: A 35-year-old G3P2 woman currently 39 weeks pregnant presents to the emergency department with painful vaginal bleeding shortly after a motor vehicle accident in which she was a passenger. She had her seat belt on and reports that the airbag deployed immediately upon her car's impact against a tree. She admits that she actively smokes cigarettes. Her prenatal workup is unremarkable. Her previous pregnancies were remarkable for one episode of chorioamnionitis that resolved with antibiotics. Her temperature is 98.6°F (37°C), blood pressure is 90/60 mmHg, pulse is 130/min, and respirations are 20/min. The fetal pulse is 110/min. Her uterus is tender and firm. The remainder of her physical exam is unremarkable. What is the most likely diagnosis?
- A. Placental abruption (Correct Answer)
- B. Eclampsia
- C. Vasa previa
- D. Preterm labor
- E. Preeclampsia
Trauma in pregnancy Explanation: ***Placental abruption***
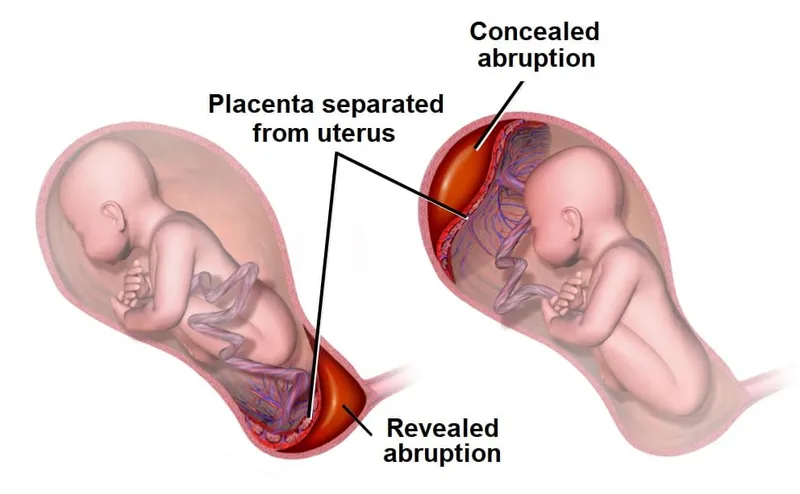
- The patient's presentation with **painful vaginal bleeding** after blunt abdominal trauma (motor vehicle accident), a **tender and firm uterus**, maternal **hypotension** and **tachycardia**, and fetal **bradycardia** is highly characteristic of placental abruption.
- Risk factors like **smoking** and trauma further increase the likelihood of placental abruption.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a pregnant woman with preeclampsia, which is not present in this scenario.
- While the patient's low blood pressure and tachycardia are concerning, they do not point to eclampsia.
*Vasa previa*
- Vasa previa involves **fetal blood vessels** running within the fetal membranes over the internal cervical os, risking rupture during labor or membrane rupture, leading to **painless vaginal bleeding** and **fetal distress**.
- The bleeding in this case is described as painful, and the uterine tenderness and firmness are not typical of vasa previa.
*Preterm labor*
- Preterm labor is defined by **regular uterine contractions** causing cervical changes before 37 weeks of gestation, which is not aligned with the patient being 39 weeks pregnant or her symptoms.
- While trauma can initiate labor, the severity of the bleeding and maternal/fetal distress point away from isolated preterm labor.
*Preeclampsia*
- Preeclampsia is characterized by **new-onset hypertension** (blood pressure ≥140/90 mmHg) and **proteinuria** after 20 weeks of gestation.
- This patient presents with hypotension and no mention of hypertension or proteinuria, making preeclampsia unlikely.
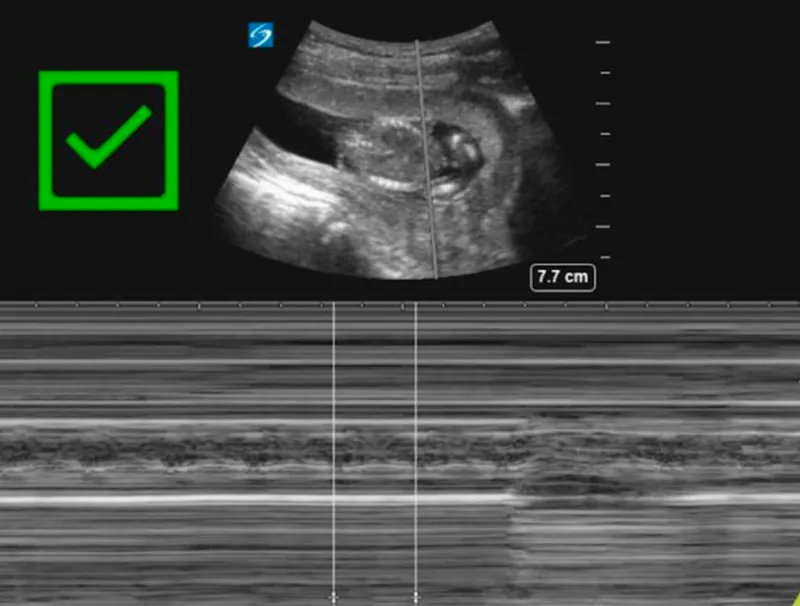
Trauma in pregnancy US Medical PG Question 2: A 26-year-old primigravid woman at 39 weeks' gestation is admitted to the hospital in active labor. Pregnancy was complicated by mild oligohydramnios detected a week ago, which was managed with hydration. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. Pelvic examination shows 100% cervical effacement and 10 cm cervical dilation; the vertex is at 0 station. Cardiotocography is shown. Which of the following is the most appropriate next step in management?
- A. Maternal repositioning and oxygen administration (Correct Answer)
- B. Emergent cesarean section
- C. Elevation of the fetal head
- D. Reassurance
- E. Rapid amnioinfusion
Trauma in pregnancy Explanation: ***Maternal repositioning and oxygen administration***
- The cardiotocography shows **variable decelerations**, which are characterized by an abrupt decrease in fetal heart rate, often U, V, or W shaped, and not consistently related to contractions.
- Initial management for variable decelerations, common in cases of **oligohydramnios**, involves conservative measures like **maternal repositioning** (e.g., left lateral, right lateral, hands and knees) to relieve umbilical cord compression and administering **oxygen** to improve fetal oxygenation.
*Emergent cesarean section*
- While severe, unremitting variable decelerations unresponsive to conservative measures may warrant a cesarean section, the current tracing does not indicate an **immediate obstetric emergency** requiring such an invasive procedure as the first step.
- An emergent cesarean section is reserved for situations of **persistent non-reassuring fetal status** despite intervention.
*Elevation of the fetal head*
- Elevating the fetal head is typically done to **relieve umbilical cord prolapse** during a vaginal examination, a condition that might present with sudden, profound decelerations or bradycardia, which is not clearly depicted as the primary issue here.
- This maneuver is an intervention for a specific obstetric emergency and does not address the underlying pathophysiology of variable decelerations due to cord compression.
*Reassurance*
- The presence of **variable decelerations** indicates **umbilical cord compression** and potential fetal compromise, requiring active intervention rather than passive reassurance.
- Reassurance alone is insufficient and inappropriate when there are signs of **fetal distress** on the cardiotocograph.
*Rapid amnioinfusion*
- **Amnioinfusion** can be considered for **recurrent variable decelerations** due to oligohydramnios that are unresponsive to maternal repositioning and oxygen.
- It is generally not the *first* step, as less invasive measures should be attempted first. Moreover, rapid amnioinfusion carries its own risks and should be carefully considered.
Trauma in pregnancy US Medical PG Question 3: A clinical diagnosis of abruptio placentae is suspected. Which of the following is the most appropriate next step in the management of this patient?
- A. Vaginal delivery
- B. Administration of intravenous oxytocin
- C. Administration of intramuscular betamethasone
- D. Administration of intravenous fluids (Correct Answer)
- E. Administration of intravenous tranexamic acid
Trauma in pregnancy Explanation: ***Administration of intravenous fluids***
- In suspected **abruptio placentae**, significant **blood loss** can occur, leading to maternal **hypotension** and compromise.
- **Intravenous fluids** are crucial for immediate **volume replacement** and maintaining **hemodynamic stability** in both the mother and fetus.
*Vaginal delivery*
- While delivery is often necessary, the **route of delivery** depends on the severity of the abruption, fetal status, and maternal stability; immediate vaginal delivery is not the universal first step before stabilization.
- In cases of severe abruption or fetal distress, an **emergency C-section** might be more appropriate, but **maternal stabilization** with fluids is paramount first.
*Administration of intravenous oxytocin*
- **Oxytocin** is primarily used to **induce labor** or augment contractions, and to prevent or treat **postpartum hemorrhage**.
- It is not indicated as an initial management step for **abruptio placentae**, as it would not address the acute blood loss or fetal compromise.
*Administration of intramuscular betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery.
- While it might be considered if the fetus is preterm and delivery can be delayed for 24-48 hours, **maternal stabilization** and management of acute abruption symptoms take precedence.
*Administration of intravenous tranexamic acid*
- **Tranexamic acid** is an **antifibrinolytic** agent used to reduce bleeding in various settings, including postpartum hemorrhage.
- However, in acute **abruptio placentae**, the immediate concern is **volume resuscitation** rather than directly inhibiting fibrinolysis as the primary first step.
Trauma in pregnancy US Medical PG Question 4: A 36-year-old woman, gravida 3, para 2, at 37 weeks' gestation comes to the emergency department because of sparse vaginal bleeding for 3 hours. She also noticed the bleeding 3 days ago. She has had no prenatal care. Both of her previous children were delivered by lower segment transverse cesarean section. Her temperature is 37.1°C (98.8°F), pulse is 90/min, respirations are 16/min, and blood pressure is 110/80 mm Hg. The abdomen is nontender, and no contractions are felt. Examination shows that the fetus is in a vertex presentation. The fetal heart rate is 160/min and shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Perform cesarean delivery
- B. Perform transvaginal sonography (Correct Answer)
- C. Perform Kleihauer-Betke test
- D. Perform pelvic examination
- E. Conduct contraction stress test
Trauma in pregnancy Explanation: ***Perform transvaginal sonography***
- The history of **previous cesarean sections** and **painless vaginal bleeding** raises suspicion for **placenta previa**.
- **Transvaginal sonography** is the gold standard for diagnosing placenta previa, as it accurately visualizes the relationship between the placenta and the cervical os without increasing bleeding risk.
*Perform cesarean delivery*
- While a cesarean delivery may eventually be necessary if **placenta previa** is confirmed, it is premature to proceed without a definitive diagnosis.
- An immediate cesarean delivery is indicated only in cases of **heavy, uncontrolled bleeding** or fetal distress, neither of which is present here.
*Perform Kleihauer-Betke test*
- The **Kleihauer-Betke test** measures the amount of fetal hemoglobin transferred into the maternal bloodstream for quantifying **fetomaternal hemorrhage**, which is typically performed after a potential placental abruption or trauma.
- This test is not primarily used for diagnosing the **cause of vaginal bleeding** in this context and would not identify placenta previa.
*Perform pelvic examination*
- A **digital pelvic examination** is **contraindicated** in cases of suspected placenta previa due to the risk of exacerbating bleeding and potentially causing **massive hemorrhage**.
- Even a speculum examination should generally be deferred until a sonogram has ruled out placenta previa to avoid disturbing the placenta.
*Conduct contraction stress test*
- A **contraction stress test** assesses **fetal well-being** in response to uterine contractions and is used to evaluate uteroplacental insufficiency.
- It does not help in diagnosing the cause of **vaginal bleeding** and is not the appropriate first step in a patient with suspected placenta previa.
Trauma in pregnancy US Medical PG Question 5: A 24-year-old primigravida presents at 36 weeks gestation with vaginal bleeding, mild abdominal pain, and uterine contractions that appeared after bumping into a handrail. The vital signs are as follows: blood pressure 130/80 mm Hg, heart rate 79/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The fetal heart rate was 145/min. Uterine fundus is at the level of the xiphoid process. Slight uterine tenderness and contractions are noted on palpation. The perineum is bloody. The gynecologic examination shows no vaginal or cervical lesions. The cervix is long and closed. Streaks of bright red blood are passing through the cervix. A transabdominal ultrasound shows the placenta to be attached to the lateral uterine wall with a marginal retroplacental hematoma (an approximate volume of 150 ml). The maternal hematocrit is 36%. What is the next best step in the management of this patient?
- A. Manage as an outpatient with modified rest
- B. Induction of vaginal labor
- C. Corticosteroid administration and schedule a cesarean section after
- D. Admit for maternal and fetal monitoring and observation (Correct Answer)
- E. Urgent cesarean delivery
Trauma in pregnancy Explanation: ***Admit for maternal and fetal monitoring and observation***
- This patient presents with signs of a **mild placental abruption** (vaginal bleeding, contractions, mild abdominal pain, retroplacental hematoma) after trauma, but her **vital signs are stable**, fetal heart rate is reassuring, and the abruption volume is relatively small.
- Expectant management with **close monitoring** for signs of worsening abruption (increasing pain, vital sign changes, fetal distress) is appropriate for a patient at 36 weeks with a non-catastrophic abruption.
*Manage as an outpatient with modified rest*
- Given the presence of **vaginal bleeding, contractions**, and a **retroplacental hematoma** suggesting placental abruption, outpatient management is not safe.
- There is a risk of the abruption progressing, requiring immediate medical intervention, making **hospital admission for close monitoring** essential.
*Induction of vaginal labor*
- While vaginal delivery might be considered for a stable abruption in some cases, **active induction is not the immediate next step** given the patient's stable status and the need for continuous monitoring.
- The **cervix is long and closed**, indicating that she is not in active labor and immediate induction might not be successful or necessary.
*Corticosteroid administration and schedule a cesarean section after*
- **Corticosteroids** are typically administered for fetal lung maturity when delivery is anticipated before **34 weeks of gestation**; at 36 weeks, this is generally not indicated.
- A scheduled cesarean section is premature as the patient is **stable**, and the immediate goal is to monitor for progression or resolution of the abruption, not immediate delivery.
*Urgent cesarean delivery*
- There are no signs of **maternal or fetal distress** (stable vitals, reassuring fetal heart rate) that would necessitate an urgent cesarean delivery.
- An urgent cesarean is reserved for cases of **severe abruption** with significant bleeding, hemodynamic instability, or fetal compromise.
Trauma in pregnancy US Medical PG Question 6: A research group wants to assess the safety and toxicity profile of a new drug. A clinical trial is conducted with 20 volunteers to estimate the maximum tolerated dose and monitor the apparent toxicity of the drug. The study design is best described as which of the following phases of a clinical trial?
- A. Phase 0
- B. Phase III
- C. Phase V
- D. Phase II
- E. Phase I (Correct Answer)
Trauma in pregnancy Explanation: ***Phase I***
- **Phase I clinical trials** involve a small group of healthy volunteers (typically 20-100) to primarily assess **drug safety**, determine a safe dosage range, and identify side effects.
- The main goal is to establish the **maximum tolerated dose (MTD)** and evaluate the drug's pharmacokinetic and pharmacodynamic profiles.
*Phase 0*
- **Phase 0 trials** are exploratory studies conducted in a very small number of subjects (10-15) to gather preliminary data on a drug's **pharmacodynamics and pharmacokinetics** in humans.
- They involve microdoses, not intended to have therapeutic effects, and thus cannot determine toxicity or MTD.
*Phase III*
- **Phase III trials** are large-scale studies involving hundreds to thousands of patients to confirm the drug's **efficacy**, monitor side effects, compare it to standard treatments, and collect information that will allow the drug to be used safely.
- These trials are conducted after safety and initial efficacy have been established in earlier phases.
*Phase V*
- "Phase V" is not a standard, recognized phase in the traditional clinical trial classification (Phase 0, I, II, III, IV).
- This term might be used in some non-standard research contexts or for post-marketing studies that go beyond Phase IV surveillance, but it is not a formal phase for initial drug development.
*Phase II*
- **Phase II trials** involve several hundred patients with the condition the drug is intended to treat, focusing on **drug efficacy** and further evaluating safety.
- While safety is still monitored, the primary objective shifts to determining if the drug works for its intended purpose and at what dose.
Trauma in pregnancy US Medical PG Question 7: A 29-year-old G1P0 female at 32 weeks gestation presents to the emergency department with vaginal bleeding. She has had minimal prenatal care to-date with only an initial visit with an obstetrician after a positive home pregnancy test. She describes minimal spotting that she noticed earlier today that has progressed to larger amounts of blood; she estimates 30 mL of blood loss. She denies any cramping, pain, or contractions, and she reports feeling continued movements of the baby. Ultrasound and fetal heart rate monitoring confirm the presence of a healthy fetus without any evidence of current or impending complications. The consulted obstetrician orders blood testing for Rh-status of both the mother as well as the father, who brought the patient to the hospital. Which of the following represents the best management strategy for this situation?
- A. After 28 weeks gestation, administration of RhoGAM will have no benefit
- B. If mother is Rh-positive and father is Rh-negative then administer RhoGAM
- C. If mother is Rh-negative and father is Rh-negative then administer RhoGAM
- D. If mother is Rh-negative and father is Rh-positive, RhoGAM administration is not needed
- E. If mother is Rh-negative and father is Rh-positive then administer RhoGAM (Correct Answer)
Trauma in pregnancy Explanation: ***If mother is Rh-negative and father is Rh-positive then administer RhoGAM***
- This combination creates a risk for **Rh incompatibility**, meaning the fetus could be Rh-positive and the mother's immune system could form antibodies against fetal red blood cells, which can harm the fetus in future pregnancies.
- **RhoGAM (Rh immunoglobulin)** administration prevents the mother from forming these antibodies when there's a risk of maternal-fetal blood mixing, as indicated by vaginal bleeding.
*After 28 weeks gestation, administration of RhoGAM will have no benefit*
- This statement is incorrect; **RhoGAM is routinely administered around 28 weeks gestation** as prophylaxis in Rh-negative mothers, even without bleeding episodes, to prevent sensitization.
- In cases of potential fetal-maternal hemorrhage, such as vaginal bleeding, RhoGAM is indicated regardless of gestational age beyond the first trimester.
*If mother is Rh-positive and father is Rh-negative then administer RhoGAM*
- This scenario does not pose a risk for **Rh incompatibility hemolytic disease of the newborn**, as the mother already possesses the Rh antigen.
- RhoGAM is specifically given to Rh-negative mothers to prevent their immune system from reacting to an Rh-positive fetus.
*If mother is Rh-negative and father is Rh-negative then administer RhoGAM*
- In this case, both parents are **Rh-negative**, meaning the fetus will also be Rh-negative.
- There is no risk of **Rh incompatibility** or sensitization, so RhoGAM administration is not indicated.
*If mother is Rh-negative and father is Rh-positive, RhoGAM administration is not needed*
- This statement is incorrect and represents a critical misunderstanding of **Rh incompatibility prophylaxis**.
- This specific genetic combination creates the highest risk for **Rh sensitization** during pregnancy, especially with events like vaginal bleeding, making RhoGAM administration essential.
Trauma in pregnancy US Medical PG Question 8: A student health coordinator plans on leading a campus-wide HIV screening program that will be free for the entire undergraduate student body. The goal is to capture as many correct HIV diagnoses as possible with the fewest false positives. The coordinator consults with the hospital to see which tests are available to use for this program. Test A has a sensitivity of 0.92 and a specificity of 0.99. Test B has a sensitivity of 0.95 and a specificity of 0.96. Test C has a sensitivity of 0.98 and a specificity of 0.93. Which of the following testing schemes should the coordinator pursue?
- A. Test A on the entire student body followed by Test B on those who are positive
- B. Test A on the entire student body followed by Test C on those who are positive
- C. Test C on the entire student body followed by Test B on those who are positive
- D. Test C on the entire student body followed by Test A on those who are positive (Correct Answer)
- E. Test B on the entire student body followed by Test A on those who are positive
Trauma in pregnancy Explanation: ***Test C on the entire student body followed by Test A on those who are positive***
- To "capture as many correct HIV diagnoses as possible" (maximize true positives), the initial screening test should have the **highest sensitivity**. Test C has the highest sensitivity (0.98).
- To "capture as few false positives as possible" (maximize true negatives and confirm diagnoses), the confirmatory test should have the **highest specificity**. Test A has the highest specificity (0.99).
*Test A on the entire student body followed by Test B on those who are positive*
- Starting with Test A (sensitivity 0.92) would miss more true positive cases than starting with Test C (sensitivity 0.98), failing the goal of **capturing as many cases as possible**.
- Following with Test B (specificity 0.96) would result in more false positives than following with Test A (specificity 0.99).
*Test A on the entire student body followed by Test C on those who are positive*
- This scheme would miss many true positive cases initially due to Test A's lower sensitivity compared to Test C.
- Following with Test C would introduce more false positives than necessary, as it has a lower specificity (0.93) than Test A (0.99).
*Test C on the entire student body followed by Test B on those who are positive*
- While Test C is a good initial screen for its high sensitivity, following it with Test B (specificity 0.96) is less optimal than Test A (specificity 0.99) for minimizing false positives in the confirmation step.
- This combination would therefore yield more false positives in the confirmatory stage than using Test A.
*Test B on the entire student body followed by Test A on those who are positive*
- Test B has a sensitivity of 0.95, which is lower than Test C's sensitivity of 0.98, meaning it would miss more true positive cases at the initial screening stage.
- While Test A provides excellent specificity for confirmation, the initial screening step is suboptimal for the goal of capturing as many diagnoses as possible.
Trauma in pregnancy US Medical PG Question 9: A 28-year-old woman at 30 weeks gestation is rushed to the emergency room with the sudden onset of vaginal bleeding accompanied by intense abdominopelvic pain and uterine contractions. The intensity and frequency of pain have increased in the past 2 hours. This is her 1st pregnancy and she was diagnosed with gestational diabetes several weeks ago. Her vital signs include a blood pressure of 124/68 mm Hg, a pulse of 77/min, a respiratory rate of 22/min, and a temperature of 37.0°C (98.6°F). The abdominal examination is positive for a firm and tender uterus. An immediate cardiotocographic evaluation reveals a fetal heart rate of 150/min with prolonged and repetitive decelerations and high-frequency and low-amplitude uterine contractions. Your attending physician warns you about delaying the vaginal physical examination until a quick sonographic evaluation is completed. Which of the following is the most likely diagnosis in this patient?
- A. Miscarriage
- B. Vasa previa
- C. Placenta abruption (Correct Answer)
- D. Placenta previa
- E. Uterine rupture
Trauma in pregnancy Explanation: **Placenta abruption**
- The sudden onset of **vaginal bleeding** with **intense abdominopelvic pain**, **uterine contractions**, and a **firm, tender uterus** strongly suggests **placental abruption**.
- **Fetal decelerations** and the physician's warning against immediate vaginal examination (due to potential for exacerbating hemorrhage if it were placenta previa) further support this diagnosis.
*Miscarriage*
- This patient is at **30 weeks gestation**, whereas a miscarriage is defined as pregnancy loss before **20 weeks of gestation**.
- While bleeding and pain occur, the gestational age rules against a diagnosis of miscarriage.
*Vasa previa*
- **Vasa previa** is characterized by rupture of fetal vessels, leading to **fetal bleeding** and **sudden, painless vaginal bleeding**.
- The patient's presentation includes **intense abdominopelvic pain** and **uterine contractions**, which are not typical of vasa previa.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** and usually does not involve intense abdominal pain or a **firm, tender uterus**.
- The patient's symptoms of significant pain and uterine contractions are inconsistent with placenta previa.
*Uterine rupture*
- **Uterine rupture** is a catastrophic event, often preceded by a history of **uterine surgery** or trauma, and presents with sudden, severe pain, **fetal distress**, and a **palpable fetal parts** outside the uterus.
- While there is pain and fetal distress, the presence of a **firm, tender uterus** and the absence of a history of uterine surgery make abruption a more likely diagnosis.
Trauma in pregnancy US Medical PG Question 10: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Trauma in pregnancy Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
More Trauma in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.