Resuscitative thoracotomy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Resuscitative thoracotomy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
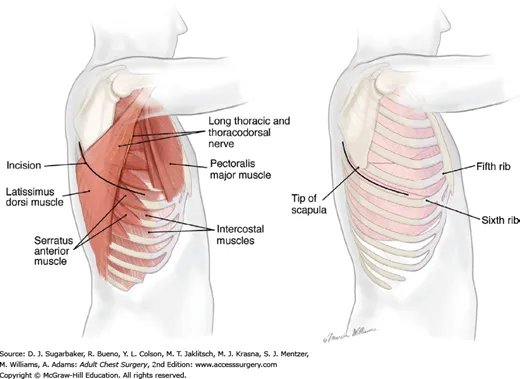
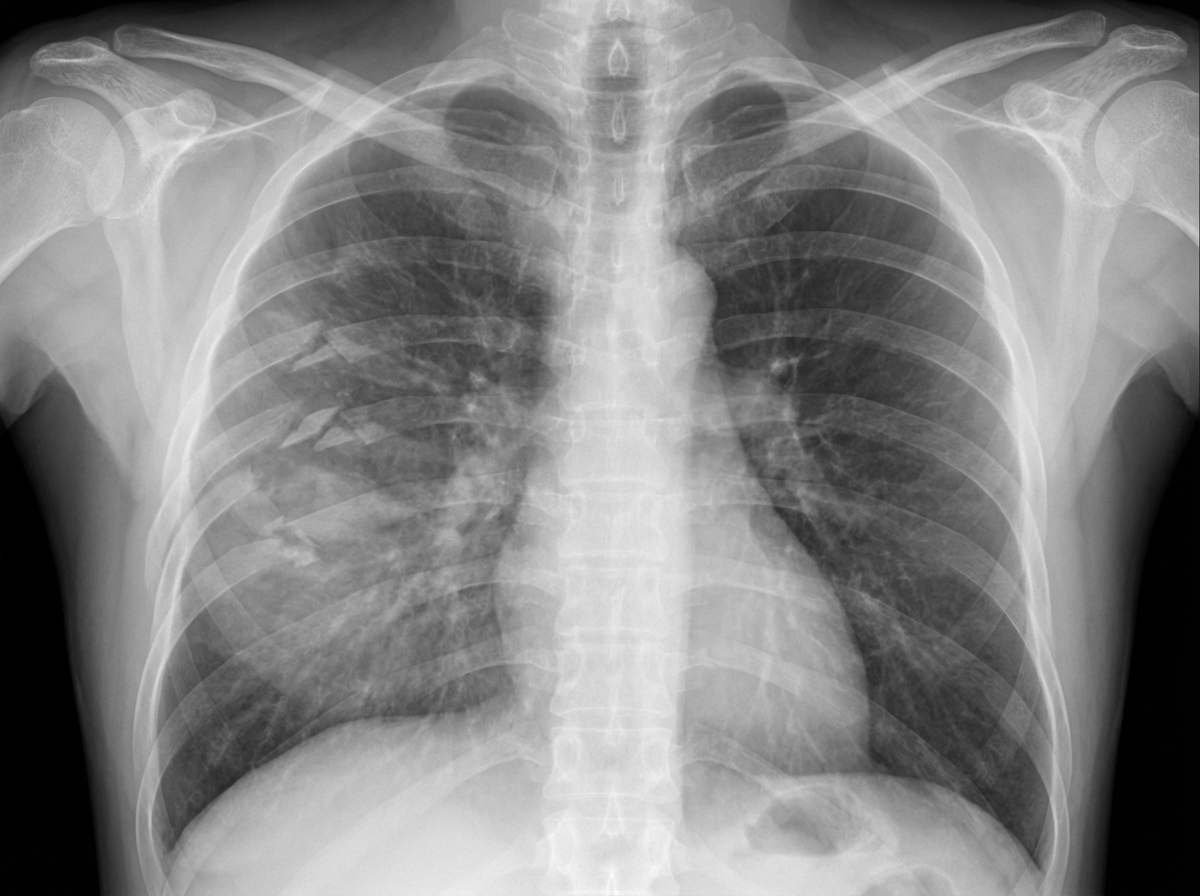
Resuscitative thoracotomy US Medical PG Question 1: A 27-year-old man is brought to the emergency department 45 minutes after being involved in a motor vehicle collision. He is agitated. He has pain in his upper right arm, which he is cradling in his left arm. His temperature is 36.7°C (98°F), pulse is 135/min, respirations are 25/min, and blood pressure is 145/90 mm Hg. His breathing is shallow. Pulse oximetry on 100% oxygen via a non-rebreather face mask shows an oxygen saturation of 83%. He is confused and oriented only to person. Examination shows multiple bruises on the right anterior thoracic wall. The pupils are equal and reactive to light. On inspiration, his right chest wall demonstrates paradoxical inward movement while his left chest wall is expanding. There is pain to palpation and crepitus over his right anterior ribs. The remainder of the examination shows no abnormalities. An x-ray of the chest is shown. Two large-bore IVs are placed. After fluid resuscitation and analgesia, which of the following is the most appropriate next step in management?
- A. Bedside thoracotomy
- B. Surgical fixation of right third to sixth ribs
- C. Intubation with positive pressure ventilation (Correct Answer)
- D. Placement of a chest tube
- E. CT scan of the chest
Resuscitative thoracotomy Explanation: ***Intubation with positive pressure ventilation***
- The patient presents with **flail chest** (paradoxical chest wall movement with pain and crepitus), respiratory distress (tachypnea, shallow breathing), and **hypoxemia** (SpO2 83% on 100% oxygen) despite initial fluid resuscitation and analgesia. These are clear indications for **endotracheal intubation** and mechanical ventilation to stabilize the chest wall, improve oxygenation, and reduce the work of breathing.
- **Positive pressure ventilation** helps to internally splint the flail segment, enabling more effective gas exchange and preventing further atelectasis.
*Bedside thoracotomy*
- **Bedside thoracotomy** is typically reserved for patients in traumatic cardiac arrest who have witnessed signs of life on arrival or are in profound shock unresponsive to other resuscitative measures, making it inappropriate here.
- This patient is **hemodynamically stable** (BP 145/90 mmHg) and does not show signs of massive hemorrhage or cardiac tamponade requiring immediate thoracotomy.
*Surgical fixation of right third to sixth ribs*
- **Surgical fixation of rib fractures** is a more definitive treatment for flail chest but is not an immediate life-saving intervention in the setting of acute respiratory failure and hypoxemia.
- While it can be considered later to reduce pain and improve pulmonary mechanics, the priority is to stabilize the patient's respiratory status through **ventilation**.
*Placement of a chest tube*
- **Placement of a chest tube** is indicated for pneumothorax, hemothorax, or empyema. While a pneumothorax or hemothorax could be present given the trauma and rib fractures, the primary issue driving this patient's acute respiratory failure is the **flail chest leading to inadequate ventilation and oxygenation**.
- There is no mention of diminished breath sounds or hyperresonance/dullness to percussion, which would suggest pneumothorax or hemothorax as the primary and immediate problem after initial resuscitation.
*CT scan of the chest*
- A **CT scan of the chest** is an important diagnostic tool to assess the extent of injuries, but it is not an immediate therapeutic intervention for a patient in acute respiratory failure and severe hypoxemia.
- Delaying definitive airway management for a diagnostic test in an unstable patient is **inappropriate** and could worsen the patient's condition.
Resuscitative thoracotomy US Medical PG Question 2: A 28-year-old man is brought to the emergency department by ambulance after developing an altered mental state following blunt trauma to the head. The patient was competing at a local mixed martial arts competition when he was struck in the head and lost consciousness. A few minutes later, upon regaining consciousness, he had a progressive decline in mental status. Past medical history is noncontributory. Upon arrival at the hospital, the temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the pulse is 66/min, the respiratory rate is 14/min, and the oxygen saturation is 99% on room air. He is alert now. A noncontrast CT scan is performed, and the result is provided in the image. Which of the following structures is most likely affected in this patient?
- A. Subarachnoid space
- B. Suprasellar cistern
- C. Middle Meningeal artery (Correct Answer)
- D. Ventricular system
- E. Bridging veins
Resuscitative thoracotomy Explanation: ***Middle Meningeal artery***
- The CT scan shows a **lenticular** or **biconvex** shaped hemorrhage, characteristic of an **epidural hematoma**. This type of hematoma is typically caused by trauma leading to rupture of the middle meningeal artery.
- The history of blunt head trauma followed by a **lucid interval** and then progressive neurological decline strongly points to an epidural hematoma, which results from arterial bleeding.
*Subarachnoid space*
- Hemorrhage in the subarachnoid space (subarachnoid hemorrhage) typically appears as **blood filling the sulci and basal cisterns** on CT, not a localized collection like seen in the image.
- While subarachnoid hemorrhage can be traumatic, the classic presentation of an epidural hematoma (lucid interval, lenticular shape) is not consistent with primary subarachnoid bleeding.
*Suprasellar cistern*
- The suprasellar cistern is located at the base of the brain, superior to the sella turcica, and typically contains cerebrospinal fluid.
- While it can be affected by subarachnoid hemorrhage, the image clearly shows a hematoma in the temporal-parietal region, not specifically within the suprasellar cistern.
*Ventricular system*
- The ventricular system contains CSF and is an internal structure of the brain. Hemorrhage within the ventricles (intraventricular hemorrhage) would appear as blood filling the ventricular spaces.
- The image shows an extra-axial hematoma, meaning outside the brain parenchyma and ventricles.
*Bridging veins*
- Rupture of bridging veins typically causes a **subdural hematoma**, which appears as a **crescent-shaped** collection of blood along the surface of the brain, conforming to the contours of the cerebral hemisphere.
- The hematoma in the image has a **lenticular (biconvex)** shape, which is characteristic of an epidural hematoma, not a subdural hematoma.
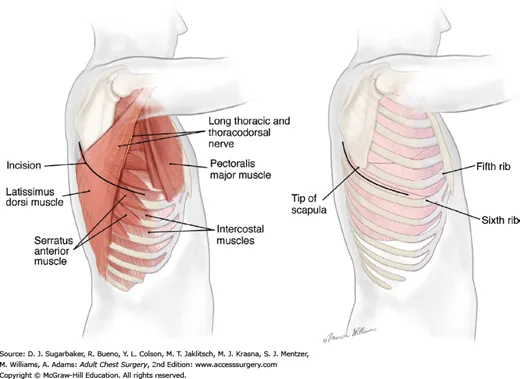
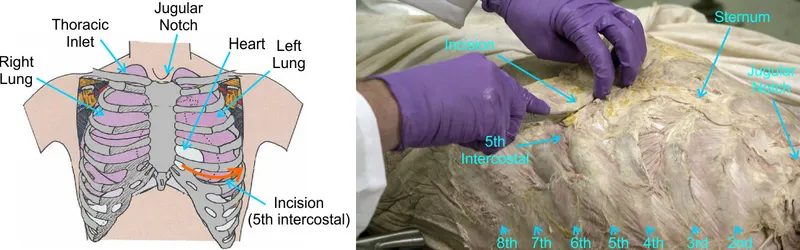
Resuscitative thoracotomy US Medical PG Question 3: A 50-year-old man presents with severe chest pain for a week. His pain increases with breathing and is localized to the right. He has tried over-the-counter medications at home, but they did not help. The patient has a 20-pack-year smoking history and currently smokes 2 packs of cigarettes daily, and he drinks 3 to 4 cans of beer daily before dinner. His temperature is 39.1°C (102.3°F), blood pressure is 127/85 mm Hg, pulse is 109/min, and respirations are 20/min. Respiratory examination shows dullness to percussion from the 7th rib inferiorly at the right midaxillary line, decreased vocal tactile fremitus, and diminished breath sounds in the same area. Chest radiograph is shown in the image. The patient is prepared for thoracocentesis. Which of the following locations would be the most appropriate for insertion of a chest tube?
- A. Below the inferior border of the 7th rib in the midaxillary line
- B. Above the superior border of the 8th rib in the midaxillary line (Correct Answer)
- C. Above the superior border of the 5th rib in the midclavicular line
- D. Below the inferior border of the 5th rib in the midaxillary line
- E. Above the superior border of the 7th rib in the midclavicular line
Resuscitative thoracotomy Explanation: ***Above the superior border of the 8th rib in the midaxillary line***
- The patient presents with symptoms and signs suggestive of a **pleural effusion** (dullness to percussion, decreased fremitus, diminished breath sounds) and potentially an **empyema** given the fever and lung consolidation on the radiograph.
- Thoracocentesis should be performed in the **midaxillary line** between the 6th and 9th ribs to avoid injuring the **diaphragm and abdominal organs**, which can rise as high as the 5th intercostal space during expiration. To prevent damage to the neurovascular bundle that runs along the inferior border of the ribs, the needle should be inserted just **above the superior border** of the rib below the chosen intercostal space.
*Below the inferior border of the 7th rib in the midaxillary line*
- Inserting below the inferior border of the 7th rib increases the risk of injuring the **neurovascular bundle** that runs along the inferior rib margin.
- Such placement might also be too low, increasing the risk of penetrating the **diaphragm** or **abdominal organs**. This location would correspond to the 8th intercostal space, but the 'below inferior border' part is incorrect.
*Above the superior border of the 5th rib in the midclavicular line*
- The **midclavicular line** is typically used for needle decompression of a tension pneumothorax (2nd intercostal space) but is not the preferred site for thoracocentesis due to the risk of striking the lung parenchyma or internal mammary artery.
- Even if considering a pneumothorax, the 5th intercostal space in the midclavicular line is not the standard site, and an effusion is indicated here.
*Below the inferior border of the 5th rib in the midaxillary line*
- Inserting below the inferior border of the 5th rib, similar to option A, risks injury to the **neurovascular bundle**.
- While in the midaxillary line, the 5th rib might be too high for an effusion, and the technique of inserting below the inferior border is incorrect.
*Above the superior border of the 7th rib in the midclavicular line*
- The **midclavicular line** is generally avoided for thoracocentesis of effusions due to the risks mentioned previously and poor drainage if the effusion is posterior.
- The 7th intercostal space in the midclavicular line is also a non-standard and less safe location for this procedure.
Resuscitative thoracotomy US Medical PG Question 4: A 28-year-old woman is brought to the emergency department 1 hour after being involved in a motor vehicle collision. She was riding a bike when she lost control and hit a car on the opposite side of the road. On arrival, she is unconscious. She has a history of intravenous heroin use. Her pulse is 56/min, respirations are 8/min and irregular, and blood pressure is 196/102 mm Hg. Examination shows a 2-cm laceration over the left cheek and a 3-cm laceration over the left chest. There are multiple abrasions over her face and chest. She opens her eyes and flexes her extremities to painful stimuli. The pupils are dilated and react sluggishly to light. There are decreased breath sounds over the left lung. The trachea is central. There is no jugular venous distention. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The left knee and right ankle are swollen; range of motion is limited. Two large-bore peripheral intravenous catheters are inserted. She is intubated and mechanical ventilation is initiated. A focused assessment with sonography in trauma is negative. An occlusive dressing is applied over the left chest wound. She is scheduled for a noncontrast CT scan of the brain. Which of the following is the underlying cause of this patient's hypertension?
- A. Elevated sympathetic response
- B. Increased intrathoracic pressure
- C. Reduced parasympathetic response
- D. Posttraumatic vasospasm
- E. Brainstem compression (Correct Answer)
Resuscitative thoracotomy Explanation: ***Brainstem compression***
- The patient's presentation with **hypertension**, **bradycardia**, and **irregular respirations** (Cushing's triad) in the setting of severe head trauma is highly indicative of **increased intracranial pressure (ICP)** leading to brainstem compression.
- Brainstem compression, often due to a mass effect from hemorrhage or edema, impairs the brainstem's ability to regulate vital functions, resulting in this classic triad.
*Elevated sympathetic response*
- While trauma typically triggers an **elevated sympathetic response** leading to tachycardia and hypertension, the presence of **bradycardia** in this patient makes a purely sympathetic surge less likely to be the underlying cause of her hypertension.
- The elevated blood pressure combined with a low heart rate points away from an unopposed sympathetic activation.
*Increased intrathoracic pressure*
- An increase in intrathoracic pressure, as seen in conditions like **tension pneumothorax**, can impair venous return and cardiac output, typically leading to **hypotension**, not hypertension.
- Although the patient has decreased breath sounds on the left, an occlusive dressing was applied, and a FAST exam was negative for significant fluid, making this less likely the cause of hypertension.
*Reduced parasympathetic response*
- A reduced parasympathetic response would generally lead to **tachycardia** rather than bradycardia, as the vagal tone would be diminished.
- The observed bradycardia, therefore, contradicts a primary issue of reduced parasympathetic activity.
*Posttraumatic vasospasm*
- **Posttraumatic vasospasm** can occur after severe brain injury, but it typically does not directly manifest as immediate, severe hypertension accompanied by bradycardia and respiratory irregularities (Cushing's triad).
- Vasospasm usually contributes to cerebral ischemia and can develop hours to days after the initial injury, not typically as the acute cause of these profound vital sign changes.
Resuscitative thoracotomy US Medical PG Question 5: A 56-year-old man is brought to the emergency department after falling 16 feet from a ladder. He has severe pain in both his legs and his right arm. He appears pale and diaphoretic. His temperature is 37.5°C (99.5°F), pulse is 120/min and weak, respirations are 26/min, and blood pressure is 80/50 mm Hg. He opens his eyes and withdraws in response to painful stimuli and makes incomprehensible sounds. The abdomen is soft and nontender. All extremities are cold, with 1+ pulses distally. Arterial blood gas analysis on room air shows:
pH 7.29
PCO2 33 mm Hg
PO2 65 mm Hg
HCO3- 15 mEq/L
A CT scan shows displaced fractures of the pelvic ring, as well as fractures of both tibiae, the right distal radius, and right proximal humerus. The patient undergoes emergent open reduction and is admitted to the intensive care unit. Which of the following best indicates inadequate fluid resuscitation?
- A. Urine output of 25 mL in 3 hours (Correct Answer)
- B. Capillary refill time of 3 seconds
- C. Base deficit of 1 mmol/L
- D. Glasgow coma score of 8
- E. High pulse pressure
Resuscitative thoracotomy Explanation: ***Urine output of 25 mL in 3 hours***
- A critically low urine output of **less than 0.5 mL/kg/hr** (or <30 mL/hr in an adult) over several hours is a direct and sensitive indicator of **renal hypoperfusion** due to inadequate fluid resuscitation, especially in the context of traumatic shock.
- Oliguria suggests that the kidneys are not receiving sufficient blood flow to maintain normal function, indicating persistent systemic hypovolemia despite initial interventions.
*Capillary refill time of 3 seconds*
- A capillary refill time of 3 seconds, while slightly prolonged (normal <2 seconds), is less definitive for **severe ongoing hypovolemia** compared to oliguria.
- It can be influenced by factors like **ambient temperature** and peripheral vasoconstriction, which are common in trauma but may not solely reflect inadequate fluid volume.
*Base deficit of 1 mmol/L*
- A base deficit of 1 mmol/L is essentially **within the normal range** (typically -2 to +2 mmol/L).
- A normal or low base deficit suggests that **tissue perfusion is adequate** and there's no significant ongoing metabolic acidosis due to anaerobic metabolism, making it an indicator of *adequate* rather than *inadequate* resuscitation.
*Glasgow coma score of 8*
- A Glasgow Coma Scale (GCS) score of 8 (Eyes: 2, Verbal: 2, Motor: 4 from the stem) indicates **moderate head injury** or altered mental status.
- While hypovolemic shock can affect mentation, a GCS of 8 is more indicative of **neurological damage** (e.g., from head trauma sustained in the fall) or other systemic issues rather than being a primary measure of fluid resuscitation status.
*High pulse pressure*
- A high pulse pressure (the difference between systolic and diastolic blood pressure) is typically seen in conditions like **sepsis** or **aortic regurgitation**.
- In a patient with hypovolemic shock, **pulse pressure is usually narrowed** due to increased peripheral vascular resistance and decreased stroke volume.
Resuscitative thoracotomy US Medical PG Question 6: A 35-year-old woman is brought to the emergency department 45 minutes after being rescued from a house fire. On arrival, she appears confused and has shortness of breath. The patient is 165 cm (5 ft 5 in) tall and weighs 55 kg (121 lb); BMI is 20 kg/m2. Her pulse is 125/min, respirations are 29/min, and blood pressure is 105/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Examination shows second and third-degree burns over the anterior surfaces of the chest and abdomen, and the anterior surface of the upper extremities. There is black debris in the mouth and nose. There are coarse breath sounds over the lung bases. Cardiac examination shows no murmurs, rubs, or gallop. Femoral and pedal pulses are palpable bilaterally. Which of the following is the most appropriate fluid regimen for this patient according to the Parkland formula?
- A. Administer 4 liters of intravenous colloids over the next 8 hours
- B. Administer 5 liters of intravenous colloids over the next 6 hours
- C. Administer 5 liters of intravenous crystalloids over the next 6 hours
- D. Administer 8 liters of intravenous colloids over the next 12 hours
- E. Administer 6 liters of intravenous crystalloids over the next 24 hours (Correct Answer)
Resuscitative thoracotomy Explanation: ***Administer 6 liters of intravenous crystalloids over the next 24 hours***
- The **Parkland formula** is 4 mL × weight (kg) × %TBSA burn. The patient's weight is 55 kg. The burns cover the anterior chest (9%), anterior abdomen (9%), and anterior surfaces of both upper extremities (4.5% + 4.5% = 9%), totaling **27% TBSA**.
- Calculation: 4 mL × 55 kg × 27% = **5,940 mL ≈ 6 liters**. Half is given in the first 8 hours (approximately 3 L), and the remaining half over the next 16 hours (approximately 3 L). Total fluid in 24 hours is approximately **6 liters of crystalloids**.
*Administer 4 liters of intravenous colloids over the next 8 hours*
- The Parkland formula primarily uses **crystalloids** (lactated Ringer's solution) for initial fluid resuscitation in burn patients, not colloids.
- Administering only 4 liters would be insufficient given the patient's 27% TBSA burn, and colloids are not first-line.
*Administer 5 liters of intravenous colloids over the next 6 hours*
- **Colloids** are not the first-line fluid for initial burn resuscitation under the Parkland formula; crystalloids are used.
- The timing of 6 hours does not align with the Parkland formula's 24-hour resuscitation period (half in first 8 hours, half in next 16 hours).
*Administer 5 liters of intravenous crystalloids over the next 6 hours*
- While **crystalloids** are appropriate, 5 liters over 6 hours represents an inappropriately rapid infusion rate that does not follow the Parkland formula timing.
- The first 8 hours should receive approximately 3 liters, not 5 liters over 6 hours, which could lead to complications such as **pulmonary edema or compartment syndrome**.
*Administer 8 liters of intravenous colloids over the next 12 hours*
- This option incorrectly specifies **colloids** instead of crystalloids as the primary fluid for burn resuscitation according to the Parkland formula.
- The volume of 8 liters exceeds the calculated requirement of 6 liters for this patient's 27% TBSA burn.
Resuscitative thoracotomy US Medical PG Question 7: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
Resuscitative thoracotomy Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Resuscitative thoracotomy US Medical PG Question 8: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Resuscitative thoracotomy Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Resuscitative thoracotomy US Medical PG Question 9: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Resuscitative thoracotomy Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Resuscitative thoracotomy US Medical PG Question 10: A 28-year-old woman is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which she was the unrestrained driver. On arrival, she is semiconscious and incoherent. She has shortness of breath and is cyanotic. Her pulse is 112/min, respirations are 59/min, and blood pressure is 128/89 mm Hg. Examination shows a 3-cm (1.2-in) laceration on the forehead and multiple abrasions over the thorax and abdomen. There is crepitation on palpation of the thorax on the right. Auscultation of the lung shows decreased breath sounds on the right side. A crunching sound synchronous with the heartbeat is heard best over the precordium. There is dullness on percussion of the right hemithorax. The lips and tongue have a bluish discoloration. There is an open femur fracture on the left. The remainder of the examination shows no abnormalities. Arterial blood gas analysis on room air shows:
pH 7.31
PCO2 55 mm Hg
PO2 42 mm Hg
HCO3- 22 mEq/L
O2 saturation 76%
The patient is intubated and mechanically ventilated. Infusion of 0.9% saline is begun. Which of the following is the most likely diagnosis?
- A. Pulmonary embolism
- B. Flail chest
- C. Tension pneumothorax
- D. Bronchial rupture (Correct Answer)
- E. Hemopneumothorax
Resuscitative thoracotomy Explanation: ***Bronchial rupture***
- The presence of a **mediastinal crunching sound (Hamman's sign)** synchronous with the heartbeat, along with **subcutaneous emphysema (crepitation)** and a significant mechanism of injury (high-speed MVA), points strongly towards a bronchial injury.
- **Decreased breath sounds** and **dullness to percussion** on the right side, combined with severe hypoxemia and hypercapnia, suggest a major airway disruption leading to air trapping and potential collapse of the lung.
*Pulmonary embolism*
- While pulmonary embolism can cause **dyspnea** and **hypoxemia**, it typically presents with clear lung auscultation and does not cause **crepitation** or a **mediastinal crunching sound**.
- The mechanism of injury and immediate onset of symptoms are more consistent with a traumatic injury rather than an embolic event.
*Flail chest*
- **Flail chest** involves paradoxical movement of a segment of the chest wall due to multiple rib fractures, which would lead to respiratory distress and crepitation.
- However, flail chest does not typically cause a **mediastinal crunching sound** or the severe degree of hypoxemia and hypercapnia seen with a major airway injury without other concomitant severe lung injury.
*Tension pneumothorax*
- A **tension pneumothorax** would cause severe respiratory distress, diminished breath sounds, and tracheal deviation (which is not described).
- While it can cause crepitation (subcutaneous emphysema) and hypoxemia, it usually presents with **hyperresonance** to percussion, not dullness, and does not produce a **mediastinal crunching sound** as prominently.
*Hemopneumothorax*
- A **hemopneumothorax** would explain **decreased breath sounds** and **dullness to percussion** due to the presence of blood and air in the pleural space.
- However, it would not typically cause a **mediastinal crunching sound** (Hamman's sign), which is highly specific for pneumomediastinum, often secondary to tracheobronchial injury.
More Resuscitative thoracotomy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.