Pelvic fractures and hemorrhage US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic fractures and hemorrhage. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pelvic fractures and hemorrhage US Medical PG Question 1: A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?
- A. Administer hydroxyethyl starch
- B. Transfusion of packed red blood cells (Correct Answer)
- C. Consult hospital ethics committee
- D. Administer high-dose iron dextran
Pelvic fractures and hemorrhage Explanation: ***Transfusion of packed red blood cells***
- This patient is in **hemorrhagic shock** (tachycardia, hypotension, low hemoglobin, and hematocrit with evidence of active bleeding), requiring emergent blood transfusion to prevent irreversible organ damage and death.
- In an **emergency setting** with an **unconscious patient** and **no documented refusal** of blood products, the principle of **presumed consent** for life-saving treatment takes precedence, especially when next of kin cannot be reached.
*Administer hydroxyethyl starch*
- **Colloids** like hydroxyethyl starch can temporarily increase intravascular volume but do not provide oxygen-carrying capacity, which is critically needed for a patient with severe anemia and hemorrhagic shock.
- While useful for volume expansion, it is **not a substitute for blood products** in severe bleeding and can have adverse effects such as kidney injury.
*Consult hospital ethics committee*
- Consulting an ethics committee is appropriate for **complex ethical dilemmas** when there is time for deliberation and the patient's life is not in immediate danger.
- In this acute, life-threatening emergency, **delaying treatment** to consult an ethics committee would jeopardize the patient's life and is not appropriate.
*Administer high-dose iron dextran*
- **Iron dextran** is used to treat iron-deficiency anemia and works by supporting red blood cell production over several days to weeks.
- It is **ineffective in acute hemorrhagic shock** where immediate restoration of oxygen-carrying capacity is required.
Pelvic fractures and hemorrhage US Medical PG Question 2: A 35-year-old patient is brought into the emergency department post motor vehicle crash. Stabilization of the patient in the trauma bay requires endotracheal intubation. The patient has a laceration on the femoral artery from shrapnel and seems to have lost large quantities of blood. The patient is transfused with 13 units of packed red blood cells. His vitals are T 96.5, HR 150, BP 90/40. Even with the direct pressure on the femoral artery, the patient continues to bleed. Results of labs drawn within the last hour are pending. Which of the following is most likely to stop the bleeding in this patient?
- A. Normal saline
- B. Fresh frozen plasma and platelets (Correct Answer)
- C. Whole blood
- D. Dextrose
- E. Cryoprecipitate
Pelvic fractures and hemorrhage Explanation: ***Fresh frozen plasma and platelets***
- This patient is experiencing **dilutional coagulopathy** due to massive transfusion of packed red blood cells, which lack clotting factors and platelets.
- **Fresh frozen plasma (FFP)** provides essential clotting factors, while **platelets** directly address thrombocytopenia, both crucial for **hemostasis**.
- This represents **standard component therapy** readily available in emergency departments.
*Normal saline*
- Administering normal saline would further dilute the remaining clotting factors and platelets, potentially **worsening the coagulopathy**.
- While essential for **volume resuscitation**, it does not provide any clotting components needed to stop bleeding.
*Whole blood*
- While **whole blood** contains red blood cells, plasma, and platelets in physiologic ratios, it is **not readily available** in most civilian trauma centers.
- Modern practice uses **component therapy** (FFP + platelets + PRBCs) which is more widely accessible and allows for targeted resuscitation.
- Low-titer O whole blood programs exist in some centers but are not universally available.
*Dextrose*
- **Dextrose solutions** primarily provide free water and glucose, used for hydration and hypoglycemia.
- It has **no hemostatic properties** and would further dilute clotting factors, exacerbating the bleeding.
*Cryoprecipitate*
- **Cryoprecipitate** is rich in **fibrinogen, factor VIII, factor XIII, and von Willebrand factor**.
- While useful for specific factor deficiencies or when fibrinogen is critically low in massive transfusions, it **does not replace all clotting factors or platelets** comprehensively as FFP and platelets would.
- Typically used as **adjunctive therapy** when fibrinogen levels are known to be low.
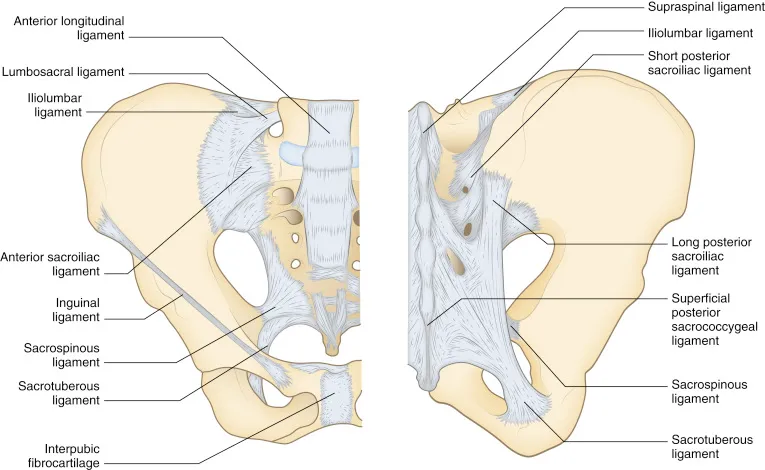
Pelvic fractures and hemorrhage US Medical PG Question 3: A 36-year-old woman comes to the physician for a 2-month history of urinary incontinence and a vaginal mass. She has a history of five full-term normal vaginal deliveries. She gave birth to a healthy newborn 2-months ago. Since then she has felt a sensation of vaginal fullness and a firm mass in the lower vagina. She has loss of urine when she coughs, sneezes, or exercises. Pelvic examination shows an irreducible pink globular mass protruding out of the vagina. A loss of integrity of which of the following ligaments is most likely involved in this patient's condition?
- A. Infundibulopelvic ligament
- B. Broad ligament of the uterus
- C. Cardinal ligament of the uterus (Correct Answer)
- D. Round ligament of uterus
- E. Uterosacral ligament
Pelvic fractures and hemorrhage Explanation: ***Cardinal ligament of the uterus***
- The patient's symptoms, including **vaginal mass**, **urinary incontinence** with coughing/sneezing, and history of **multiple vaginal deliveries**, strongly suggest **uterine prolapse**.
- The cardinal ligaments are crucial in providing **lateral cervical support** and are often damaged during childbirth, leading to uterine descent.
*Infundibulopelvic ligament*
- This ligament primarily supports the **ovaries** and contains the **ovarian artery** and vein.
- Damage to this ligament is associated with ovarian prolapse or complications during oophorectomy, not uterine prolapse.
*Broad ligament of the uterus*
- The broad ligament is a **peritoneal fold** that drapes over the uterus, fallopian tubes, and ovaries.
- While it helps to hold these structures in place, its primary role is not in preventing uterine prolapse; it mainly provides a medium for neurovascular structures.
*Round ligament of uterus*
- The round ligament extends from the uterus to the **labia majora** and primarily helps maintain **anteversion** of the uterus.
- It plays a minor role in uterine support and its laxity is not a primary cause of uterine prolapse.
*Uterosacral ligament*
- The uterosacral ligaments provide **posterior support** to the uterus, particularly by anchoring the cervix to the sacrum.
- While damage to these ligaments contributes to **apical prolapse**, the cardinal ligaments are more critical for lateral support and more commonly implicated in overall uterine prolapse following childbirth.
Pelvic fractures and hemorrhage US Medical PG Question 4: A 25-year-old woman is brought to the emergency department after being involved in a rear-end collision, in which she was the restrained driver of the back car. On arrival, she is alert and active. She reports pain in both knees and severe pain over the right groin. Temperature is 37°C (98.6°F), pulse is 116/min, respirations are 19/min, and blood pressure is 132/79 mm Hg. Physical examination shows tenderness over both knee caps. The right groin is tender to palpation. The right leg is slightly shortened, flexed, adducted, and internally rotated. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Anterior hip dislocation
- B. Posterior hip dislocation (Correct Answer)
- C. Femoral neck fracture
- D. Pelvic fracture
- E. Femoral shaft fracture
Pelvic fractures and hemorrhage Explanation: ***Posterior hip dislocation***
- The classic presentation of **posterior hip dislocation** involves the affected leg being **shortened, flexed, adducted, and internally rotated**, as described in the patient.
- This type of injury commonly occurs in **motor vehicle collisions** where the knee strikes the dashboard (dashboard injury), transmitting force up the femur to the hip joint, often causing the femoral head to dislocate posteriorly.
*Anterior hip dislocation*
- This typically presents with the affected leg in a position of **hip flexion, abduction, and external rotation**, which is contrary to the findings in this patient.
- Anterior dislocations are less common than posterior dislocations and usually result from a traumatic force applied to the hip while it is in **abduction and external rotation**.
*Femoral neck fracture*
- While a **femoral neck fracture** can cause pain and shortening of the leg, the typical presentation is usually one of **external rotation**, not internal rotation.
- The distinct **flexion, adduction, and internal rotation** triad is highly suggestive of hip dislocation, not a fracture of the femoral neck.
*Pelvic fracture*
- A **pelvic fracture** would likely present with more diffuse pelvic pain, potentially instability upon palpation of the pelvis, and possibly lower extremity neurological deficits or genitourinary symptoms depending on the fracture type.
- The specific limb positioning observed (shortened, flexed, adducted, internally rotated) is not a hallmark of an isolated pelvic fracture.
*Femoral shaft fracture*
- A **femoral shaft fracture** would cause severe pain along the shaft of the femur, significant swelling, and obvious deformity of the thigh.
- While the leg might be shortened, the specific combination of **flexion, adduction, and internal rotation** primarily points towards a hip joint issue rather than a mid-shaft fracture.
Pelvic fractures and hemorrhage US Medical PG Question 5: A 14-year-old girl is brought to the physician because of a 10-day history of vaginal bleeding. The flow is heavy with the passage of clots. Since menarche 1 year ago, menses have occurred at irregular 26- to 32-day intervals and last 3 to 6 days. Her last menstrual period was 4 weeks ago. She has no history of serious illness and takes no medications. Her temperature is 37.1°C (98.8°F), pulse is 98/min, and blood pressure is 106/70 mm Hg. Pelvic examination shows vaginal bleeding. The remainder of the examination shows no abnormalities. Her hemoglobin is 13.1 g/dL. A urine pregnancy test is negative. Which of the following is the most appropriate next step in management?
- A. Uterine curettage
- B. Tranexamic acid
- C. Endometrial ablation
- D. Uterine artery embolization
- E. Conjugated estrogen therapy (Correct Answer)
Pelvic fractures and hemorrhage Explanation: ***Conjugated estrogen therapy***
- This patient presents with **acute abnormal uterine bleeding (AUB)**, likely due to anovulation, common in adolescent girls; high-dose estrogen can rapidly stabilize the endometrium and stop acute bleeding.
- The **negative pregnancy test**, stable vital signs, and normal hemoglobin suggest her condition, while concerning, is not immediately life-threatening, making medical management with high-dose estrogen appropriate.
*Uterine curettage*
- This is an **invasive procedure** generally reserved for severe, refractory cases of AUB or in situations where endometrial sampling is required to rule out malignancy, which is unlikely in this adolescent.
- It is often unnecessary as medical management is typically effective and preferred as a **first-line treatment** in young patients.
*Tranexamic acid*
- Tranexamic acid is an **antifibrinolytic agent** that can reduce menstrual blood loss but is typically effective for reducing menorrhagia over time, not for acutely stopping heavy, ongoing bleeding with clots.
- While it can be considered for long-term management of heavy menstrual bleeding, it is **less effective than high-dose estrogen** for an acute, heavy bleeding episode.
*Endometrial ablation*
- This procedure destroys the endometrial lining and is reserved for women who have completed childbearing and have **refractory heavy menstrual bleeding** after failing medical therapies.
- It is **not appropriate for an adolescent** who has just started menstruating and whose condition is likely temporary and treatable with less invasive methods.
*Uterine artery embolization*
- Uterine artery embolization is primarily used to treat **uterine fibroids** or adenomyosis, conditions that are highly unlikely in a 14-year-old girl.
- It is an **invasive radiological procedure** with potential risks to future fertility, making it an inappropriate choice for an adolescent with presumed anovulatory bleeding.
Pelvic fractures and hemorrhage US Medical PG Question 6: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Pelvic fractures and hemorrhage Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Pelvic fractures and hemorrhage US Medical PG Question 7: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Pelvic fractures and hemorrhage Explanation: ***Bulbous urethra***
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
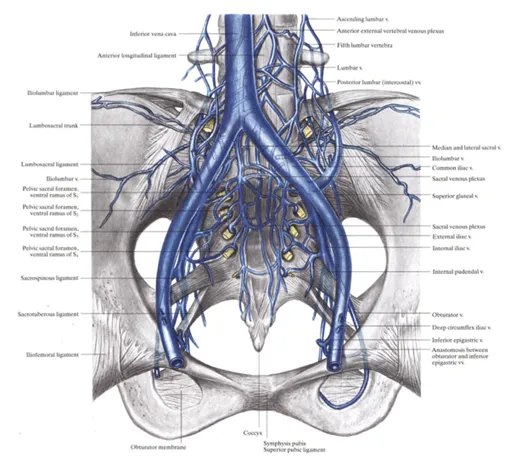
Pelvic fractures and hemorrhage US Medical PG Question 8: A 33-year-old man is brought to the emergency department because of trauma from a motor vehicle accident. His pulse is 122/min and rapid and thready, the blood pressure is 78/37 mm Hg, the respirations are 26/min, and the oxygen saturation is 90% on room air. On physical examination, the patient is drowsy, with cold and clammy skin. Abdominal examination shows ecchymoses in the right flank. The external genitalia are normal. No obvious external wounds are noted, and the rest of the systemic examination values are within normal limits. Blood is sent for laboratory testing and urinalysis shows 6 RBC/HPF. Hematocrit is 22% and serum creatinine is 1.1 mg/dL. Oxygen supplementation and IV fluid resuscitation are started immediately, but the hypotension persists. The focused assessment with sonography in trauma (FAST) examination shows a retroperitoneal fluid collection. What is the most appropriate next step in management?
- A. Perform an MRI scan of the abdomen and pelvis
- B. CT of the abdomen and pelvis with contrast
- C. Obtain a retrograde urethrogram
- D. Take the patient to the OR for an exploratory laparotomy (Correct Answer)
- E. Perform a diagnostic peritoneal lavage
Pelvic fractures and hemorrhage Explanation: ***Take the patient to the OR for an exploratory laparotomy***
- The patient is **hemodynamically unstable** (BP 78/37 mm Hg, pulse 122/min) with signs of hemorrhagic shock (cold and clammy skin, drowsy, tachycardia) and **hypotension persists despite IV fluid resuscitation**.
- FAST examination shows **retroperitoneal fluid collection** (presumed blood), flank ecchymoses (Grey Turner sign), and hematocrit of 22% indicating **significant blood loss**.
- According to **ATLS (Advanced Trauma Life Support) protocols**, hemodynamically **unstable patients with positive FAST exams require immediate surgical intervention** and should not be delayed for further imaging.
- **Exploratory laparotomy** allows for immediate identification and control of bleeding sources, which is life-saving in this persistently hypotensive patient. The retroperitoneal hematoma can be explored and bleeding vessels ligated or repaired.
*CT of the abdomen and pelvis with contrast*
- CT scan is the **appropriate next step for hemodynamically STABLE trauma patients** or those who **respond to initial resuscitation** to characterize injuries and guide management.
- This patient has **persistent hypotension despite resuscitation**, making him too unstable to safely transport to the CT scanner. Delaying surgery for imaging in an unstable patient increases mortality risk.
- The principle is: **"Blood pressure is better than pictures"** - unstable patients need operative hemorrhage control, not diagnostic imaging.
*Perform an MRI scan of the abdomen and pelvis*
- **MRI has no role in acute trauma evaluation** due to long acquisition time (30-60 minutes), limited availability, and inability to adequately monitor critically ill patients in the MRI suite.
- This would be an inappropriate and potentially fatal delay in a patient with ongoing hemorrhage and hemodynamic instability.
*Perform a diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has been largely replaced by FAST examination for detecting intraperitoneal hemorrhage in the modern trauma algorithm.
- While DPL can detect intra-abdominal blood, the **FAST has already identified retroperitoneal fluid**, and the patient's persistent instability mandates immediate surgical intervention rather than additional diagnostic procedures.
- DPL also does not evaluate the retroperitoneum well and would not change management in this unstable patient.
*Obtain a retrograde urethrogram*
- **Retrograde urethrogram (RUG)** is indicated when urethral injury is suspected (blood at meatus, high-riding prostate, perineal hematoma, inability to void).
- This patient has **normal external genitalia** and only microscopic hematuria (6 RBC/HPF), which is nonspecific in blunt trauma.
- The immediate life-threatening issue is **hemorrhagic shock from retroperitoneal bleeding**, not potential urethral injury. RUG would be an inappropriate delay in management and can be performed later if clinically indicated.
Pelvic fractures and hemorrhage US Medical PG Question 9: A 67-year-old man is brought to the emergency room after being involved in a traffic accident. He currently complains of bilateral hip pain. His vital signs are within the normal range, and he is hemodynamically stable. The pelvic compression test is positive. External genitalia appears normal, except there is blood at the urethral meatus and a contusion at the base of the scrotum. Digital rectal examination (DRE) shows a high-riding ballotable prostate. An X-ray reveals the presence of a pelvic fracture. Which of the following initial actions is the most appropriate for this patient?
- A. Insert a Foley catheter
- B. Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine
- C. Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film (Correct Answer)
- D. Obtain a urinalysis to detect microscopic hematuria
- E. Perform a suprapubic cystostomy
Pelvic fractures and hemorrhage Explanation: ***Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film***
- The combination of **blood at the urethral meatus**, a **high-riding ballotable prostate** on DRE, and a **pelvic fracture** are classic signs of a **urethral injury**, specifically a posterior urethral tear.
- A **retrograde urethrogram (RUG)** is the gold standard diagnostic test to confirm urethral injury and determine its location and extent, which is crucial before any attempt at catheterization.
*Insert a Foley catheter*
- **Insertion of a Foley catheter is contraindicated** in suspected urethral injuries, as it can worsen a partial tear into a complete transection or create a false passage.
- Doing so blindly could lead to further damage, stricture formation, and increased morbidity.
*Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine*
- This approach is premature before confirming the diagnosis and extent of urethral injury; **indigo carmine is used to assess ureteral integrity**, not urethral injury.
- Surgical exploration for urethral injury as an initial step is typically reserved for cases where RUG cannot be performed or for severe complex injuries with other indications for immediate surgery.
*Obtain a urinalysis to detect microscopic hematuria*
- While microscopic hematuria would likely be present, it is a **nonspecific finding** and does not provide information about the integrity of the urethra itself.
- It would not change the need for a RUG to assess for urethral injury in the presence of more specific signs.
*Perform a suprapubic cystostomy*
- A **suprapubic cystostomy** is the appropriate method for urinary diversion in a patient with a confirmed urethral injury if a Foley catheter cannot be safely placed.
- However, it is an intervention chosen *after* diagnosing the injury with a RUG, not the initial diagnostic step itself.
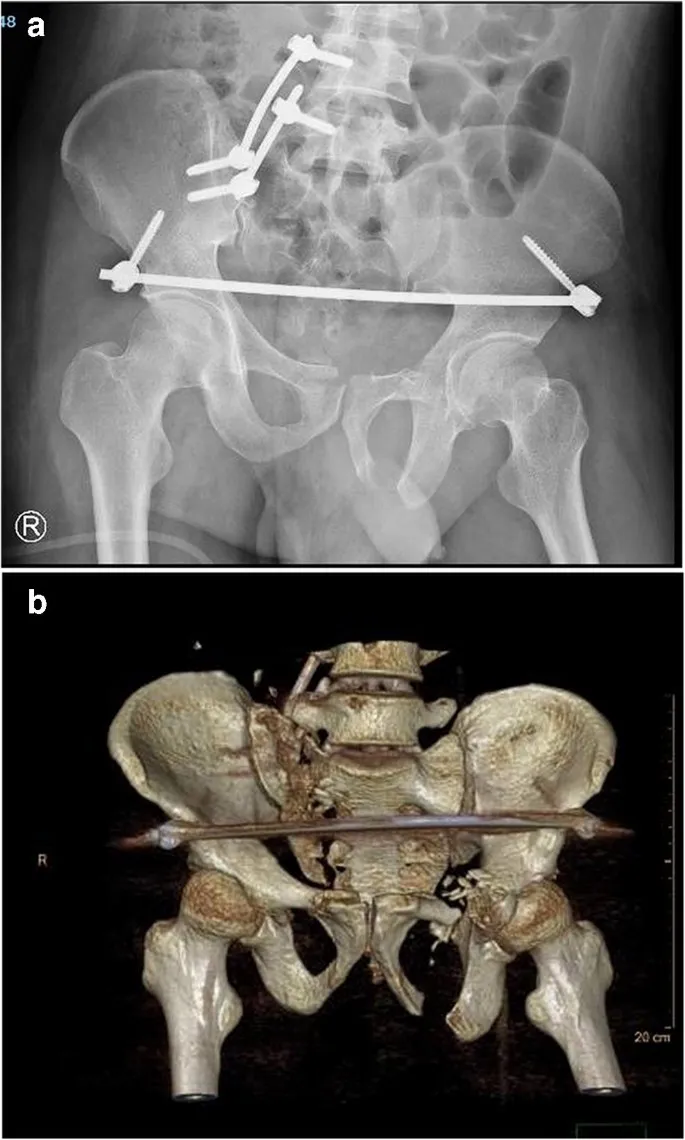
Pelvic fractures and hemorrhage US Medical PG Question 10: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Pelvic fractures and hemorrhage Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
More Pelvic fractures and hemorrhage US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.