Head trauma management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Head trauma management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Head trauma management US Medical PG Question 1: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Head trauma management Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Head trauma management US Medical PG Question 2: A 22-year-old woman comes to the emergency department because of frontal throbbing headaches for 3 weeks. Yesterday, the patient had blurry vision in both eyes and a brief episode of double vision. She has been taking ibuprofen with only mild improvement of her symptoms. She has polycystic ovarian syndrome, type 2 diabetes mellitus, and facial acne. She has not had any trauma, weakness, or changes in sensation. Her current medications include metformin and vitamin A. She is 158 cm (5 ft 2 in) tall and weighs 89 kg (196 lbs); BMI is 36 kg/m2. Vital signs are within normal limits. Examination shows decreased peripheral vision. Fundoscopic examination of both eyes is shown. MRI of the brain shows an empty sella. Which of the following is the most appropriate next step in management?
- A. Emergent craniotomy
- B. Cerebral shunt
- C. Alteplase therapy
- D. Lumbar puncture (Correct Answer)
- E. Acetazolamide therapy
Head trauma management Explanation: ***Lumbar puncture***
- This patient presents with symptoms and signs highly suggestive of **idiopathic intracranial hypertension (IIH)**, including obesity, young female sex, chronic headache, blurry and double vision, and fundoscopic findings consistent with **papilledema**. An **empty sella** on MRI also supports IIH.
- A lumbar puncture is the **definitive diagnostic test** for IIH, as it measures the **opening pressure** of cerebrospinal fluid (CSF) and can provide temporary therapeutic relief by removing CSF. Before a lumbar puncture, it's crucial to rule out mass lesions with imaging (which was done with the MRI).
*Emergent craniotomy*
- This procedure is typically reserved for severe cases of increased intracranial pressure caused by **mass lesions**, large hemorrhages, or severe cerebral edema that are unresponsive to less invasive measures.
- There is no evidence of a space-occupying lesion or acute life-threatening pressure elevation requiring such an invasive and immediate surgical intervention.
*Cerebral shunt*
- A cerebral shunt (e.g., ventriculoperitoneal shunt) is a surgical option used for **refractory IIH** or in cases where there is severe, progressive visual loss despite medical management.
- It is not the initial diagnostic or first-line therapeutic step, especially before confirming the diagnosis and trying medical management.
*Alteplase therapy*
- **Alteplase** is a **thrombolytic agent** used to dissolve blood clots, primarily in acute ischemic stroke, pulmonary embolism, or myocardial infarction.
- There is no indication of a thrombotic event or ischemic stroke in this patient's presentation.
*Acetazolamide therapy*
- **Acetazolamide** is the **first-line medical treatment** for IIH due to its ability to decrease CSF production.
- However, before initiating specific treatment, the diagnosis of IIH must be confirmed by measuring the **elevated CSF opening pressure via lumbar puncture**.
Head trauma management US Medical PG Question 3: A 24-year-old man presents to the emergency department after a motor vehicle collision. He was in the front seat and unrestrained driver in a head on collision. His temperature is 99.2°F (37.3°C), blood pressure is 90/65 mmHg, pulse is 152/min, respirations are 16/min, and oxygen saturation is 100% on room air. Physical exam is notable for a young man who opens his eyes spontaneously and is looking around. He answers questions with inappropriate responses but discernible words. He withdraws from pain but does not have purposeful movement. Which of the following is this patient's Glasgow coma scale?
- A. 9
- B. 15
- C. 7
- D. 11 (Correct Answer)
- E. 13
Head trauma management Explanation: ***11***
- **Eye-opening (E)**: The patient opens his eyes spontaneously, scoring **E4**.
- **Verbal response (V)**: He gives inappropriate responses but discernible words, scoring **V3**.
- **Motor response (M)**: He withdraws from pain but does not have purposeful movement, scoring **M4**.
- Therefore, the total Glasgow Coma Scale (GCS) score is **E4 + V3 + M4 = 11**.
*9*
- This score would imply a lower verbal or motor response, such as **incomprehensible sounds (V2)** or **abnormal flexion (M3)**, which is not consistent with the patient's presentation.
- For example, E4 + V2 + M3 would equal 9.
*15*
- A GCS of 15 indicates **normal neurological function**, meaning the patient would be fully oriented, obey commands, and open eyes spontaneously, which is not the case here.
- This score is for a patient who is fully conscious and responsive.
*7*
- A GCS of 7 suggests a **severe brain injury**, which would typically present with a much poorer response, such as **no verbal response (V1)** or **abnormal extension (M2)**.
- For example, E4 + V1 + M2 would equal 7.
*13*
- This score would mean a higher level of consciousness, such as **confused conversation (V4)** or **localizing pain (M5)**, which is better than the patient's described responses.
- For example, E4 + V4 + M5 would equal 13.
Head trauma management US Medical PG Question 4: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
Head trauma management Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
Head trauma management US Medical PG Question 5: A 3-month-old boy is brought to the emergency department by his mom for breathing difficulty after a recent fall. His parents say that he rolled off of the mattress and landed on the hard wood floor earlier today. After an extensive physical exam, he is found to have many purplish bruises and retinal hemorrhages. A non-contrast head CT scan shows a subdural hemorrhage. He was treated in the hospital with full recovery from his symptoms. Which of the following is the most important follow up plan?
- A. Provide parents with anticipatory guidance
- B. Referral to genetics for further testing
- C. Reassurance that accidents are common
- D. Inform child protective services (Correct Answer)
- E. Provide home nursing visits
Head trauma management Explanation: ***Inform child protective services***
- The combination of **multiple purplish bruises**, **retinal hemorrhages**, and **subdural hemorrhage** in a 3-month-old infant after a minor fall (rolling off a mattress) is highly suggestive of **abusive head trauma** (shaken baby syndrome).
- Healthcare professionals have a **legal and ethical obligation** to report suspected child abuse to Child Protective Services (CPS) to ensure the child's safety and initiate an investigation.
*Provide parents with anticipatory guidance*
- While anticipatory guidance on child safety and development is generally important, it is **insufficient and inappropriate** as the primary follow-up in a case of suspected child abuse.
- Focusing solely on guidance would **neglect the immediate safety concerns** and the need for investigation into the injuries.
*Referral to genetics for further testing*
- While some genetic conditions can predispose to easy bruising or bleeding, the specific pattern of injuries (**retinal hemorrhages, subdural hemorrhage, multiple bruises, and a history inconsistent with the severity of injuries**) overwhelmingly points to trauma, not a genetic disorder.
- Genetic testing would be a secondary consideration, if at all, after abuse has been ruled out or addressed.
*Reassurance that accidents are common*
- Reassuring parents that "accidents are common" would be **medically negligent and dangerous** in this scenario, as the injuries sustained are typically not caused by a simple fall from a mattress in an infant of this age.
- This response would dismiss critical signs of potential abuse and leave the child at risk.
*Provide home nursing visits*
- Home nursing visits might be beneficial for monitoring general health and development, but they do **not address the immediate and grave concern** of potential child abuse.
- The primary need is for an investigation into the cause of the injuries and protection for the child, which falls under the purview of CPS.
Head trauma management US Medical PG Question 6: A 77-year-old man with a history of hypertension and a 46 pack-year smoking history presents to the emergency department from an extended care facility with acute onset of headache, nausea, vomiting, and neck pain which started 6 hours ago and has persisted since. He is alert, but his baseline level of consciousness is slightly diminished per the nursing home staff. His temperature is 99.0°F (37.2°C), blood pressure is 164/94 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 98% on room air. The patient's neurological exam is unremarkable with cranial nerves II-XII grossly intact and with stable gait with a walker. He is immediately sent for a head CT which is normal. What is the most appropriate next step in management?
- A. Ultrasound
- B. Lumbar puncture (Correct Answer)
- C. Alteplase
- D. Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine
- E. MRI
Head trauma management Explanation: ***Lumbar puncture***
- The patient's symptoms (acute severe headache, nausea, vomiting, neck pain) and risk factors (hypertension, smoking history) are highly suggestive of a **subarachnoid hemorrhage (SAH)**, even with a normal initial **non-contrast head CT**.
- A **lumbar puncture (LP)** is the next critical diagnostic step to detect **xanthochromia** (due to bilirubin degradation from red blood cells) or elevated red blood cell count in the cerebrospinal fluid (CSF), which would confirm SAH.
- CT has approximately **95% sensitivity in the first 6 hours**, but sensitivity decreases over time, making LP essential when clinical suspicion remains high.
*Ultrasound*
- **Ultrasound** is not a standard diagnostic tool for acute neurological symptoms like severe headache or suspected SAH.
- It is primarily used for evaluating soft tissues, abdominal organs, and vascular structures like carotid arteries, but offers limited utility for intracranial bleeding.
*Alteplase*
- **Alteplase** (tissue plasminogen activator, tPA) is a thrombolytic agent used in acute ischemic stroke, characterized by focal neurological deficits due to arterial occlusion.
- Administering alteplase in the setting of headache and neck pain without focal deficits, while SAH is suspected, could be fatal as it would worsen bleeding.
*Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine*
- This combination of medications is used for **symptomatic relief** of headache and nausea but does not address the underlying potentially life-threatening cause.
- Treating symptoms without a definitive diagnosis in suspected SAH could lead to delayed intervention and worse outcomes.
*MRI*
- While **MRI with specific sequences (FLAIR, GRE, SWI)** has high sensitivity for detecting SAH and is increasingly used in clinical practice, **lumbar puncture remains the traditional and most widely recommended next step** after a negative CT in suspected SAH.
- LP directly detects **xanthochromia** (present 6-12 hours after bleeding) and RBCs in CSF, providing definitive evidence of SAH.
- MRI may not always be readily available in the emergency setting, takes longer to perform, and requires patient stability and cooperation.
- For standardized exams, **LP is the classic correct answer** when CT is negative but clinical suspicion for SAH remains high.
Head trauma management US Medical PG Question 7: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Head trauma management Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Head trauma management US Medical PG Question 8: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
Head trauma management Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
Head trauma management US Medical PG Question 9: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Head trauma management Explanation: ***Surgical evacuation of the clots***
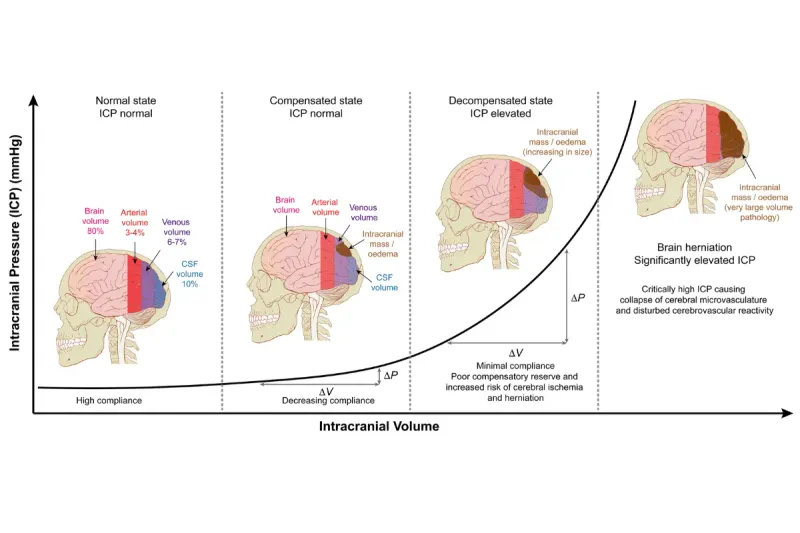
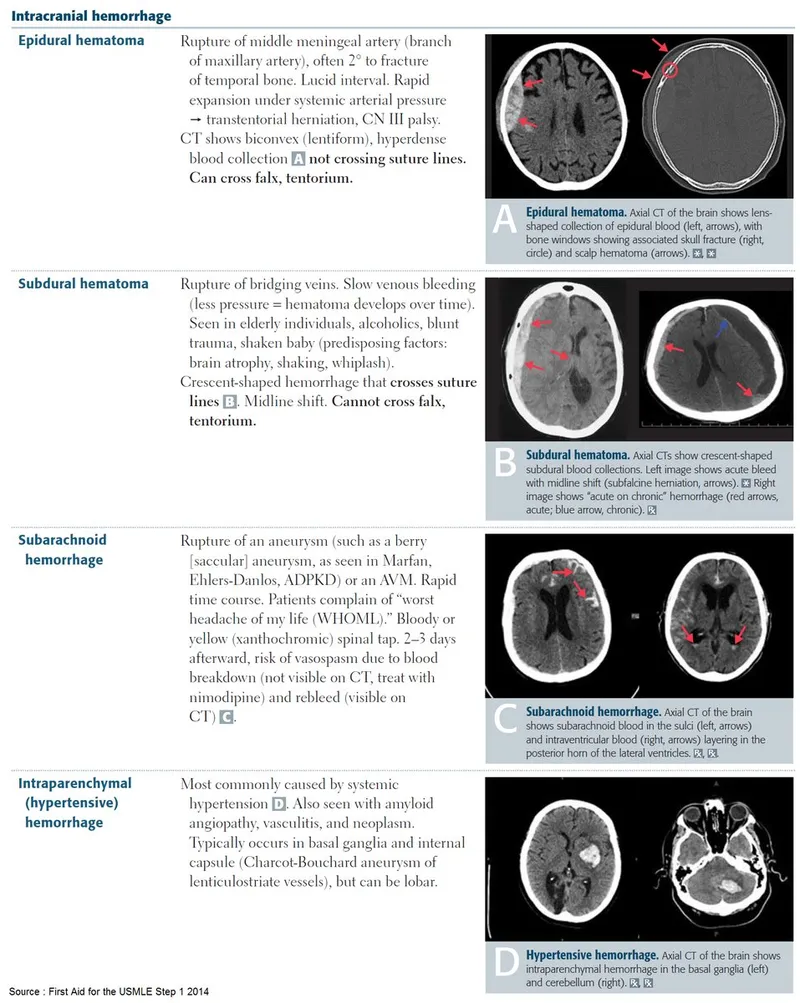
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
Head trauma management US Medical PG Question 10: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Head trauma management Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
More Head trauma management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.