Focused Assessment with Sonography in Trauma (FAST) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Focused Assessment with Sonography in Trauma (FAST). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 1: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 2: A 50-year-old male presents to the emergency with abdominal pain. He reports he has had abdominal pain associated with meals for several months and has been taking over the counter antacids as needed, but experienced significant worsening pain one hour ago in the epigastric region. The patient reports the pain radiating to his shoulders. Vital signs are T 38, HR 120, BP 100/60, RR 18, SpO2 98%. Physical exam reveals diffuse abdominal rigidity with rebound tenderness. Auscultation reveals hypoactive bowel sounds. Which of the following is the next best step in management?
- A. Admission and observation
- B. Chest radiograph
- C. 12 lead electrocardiogram
- D. Abdominal CT scan (Correct Answer)
- E. Abdominal ultrasound
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Abdominal CT scan***
- This patient presents with classic signs of a **perforated peptic ulcer**: sudden severe epigastric pain radiating to the shoulders (diaphragmatic irritation), fever, tachycardia, hypotension, and peritoneal signs (rigid abdomen with rebound tenderness).
- While the patient shows signs of **early shock** (BP 100/60, HR 120), he is **conscious and maintaining adequate oxygenation** (SpO2 98%), making him stable enough for rapid CT imaging.
- **Abdominal CT scan** is the **most sensitive and specific** test for detecting free air, identifying the location of perforation, and assessing for complications (abscess, contained perforation).
- CT provides **critical surgical planning information** about the extent and location of perforation, which can guide the surgical approach.
- This should be followed by **immediate surgical consultation** and preparation for emergency laparotomy.
*Chest radiograph*
- While an **upright chest X-ray** can detect free air under the diaphragm (pneumoperitoneum), it has **lower sensitivity** (70-80%) compared to CT scan (>95%).
- In a patient who is stable enough for imaging, **CT is preferred** as it provides more information for surgical planning.
- Chest X-ray would be the appropriate choice only if **CT is unavailable** or if the patient is **too unstable** to be transported to the CT scanner.
*Admission and observation*
- This patient has **acute peritonitis** from a likely perforated viscus, which is a **surgical emergency** requiring operative intervention.
- Observation would be inappropriate and dangerous, leading to **septic shock**, **multi-organ failure**, and death.
*12 lead electrocardiogram*
- While epigastric pain can sometimes be cardiac in origin, the **peritoneal signs** (rigid abdomen, rebound tenderness, hypoactive bowel sounds) clearly indicate an **intra-abdominal pathology**.
- The pain radiation to **both shoulders** (Kehr's sign) suggests diaphragmatic irritation from intraperitoneal air or fluid, not cardiac ischemia.
*Abdominal ultrasound*
- Ultrasound is useful for evaluating **solid organ injury**, **free fluid**, and conditions like **cholecystitis** or **appendicitis**.
- However, it is **poor at detecting free air** due to bowel gas artifact and has limited sensitivity for perforated viscus.
- It would not provide adequate information for this surgical emergency.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 3: A 41-year-old man is admitted to the emergency room after being struck in the abdomen by a large cement plate while transporting it. On initial assessment by paramedics at the scene, his blood pressure was 110/80 mm Hg, heart rate 85/min, with no signs of respiratory distress. On admission, the patient is alert but in distress. He complains of severe, diffuse, abdominal pain and severe weakness. Vital signs are now: blood pressure 90/50 mm Hg, heart rate 96/min, respiratory rate 19/min, temperature 37.4℃ (99.3℉), and oxygen saturation of 95% on room air. His lungs are clear on auscultation. The cardiac exam is significant for a narrow pulse pressure. Abdominal examination reveals a large bruise over the epigastric and periumbilical regions. The abdomen is distended and there is diffuse tenderness to palpation with rebound and guarding, worst in the epigastric region. There is hyperresonance to percussion in the epigastric region and absence of hepatic dullness in the right upper quadrant. Aspiration of the nasogastric tube reveals bloody contents. Focused assessment with sonography for trauma (FAST) shows free fluid in the pelvic region. Evaluation of the perisplenic and perihepatic regions is impossible due to the presence of free air. Aggressive intravenous fluid resuscitation is administered but fails to improve upon the patient’s hemodynamics. Which of the following is the next best step in management?
- A. Emergency laparoscopy
- B. Abdominal ultrasound
- C. Diagnostic peritoneal lavage (DPL)
- D. Emergency laparotomy (Correct Answer)
- E. CT scan
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** unresponsive to fluid resuscitation, coupled with clear signs of **perforation** (hyperresonance, absent hepatic dullness, free air on FAST limited view). This clinical picture is a direct indication for immediate surgical intervention.
- The presence of bloody nasogastric tube contents, diffuse tenderness with rebound and guarding, and a history of significant blunt trauma further support the need for urgent exploratory **laparotomy** to identify and repair the source of injury.
*Emergency laparoscopy*
- While laparoscopy can be used for abdominal exploration, it is **contraindicated in hemodynamically unstable patients** due to the need for pneumoperitoneum, which can further compromise cardiovascular stability.
- In cases of suspected visceral perforation with extensive free air and massive bleeding, **laparoscopy may be technically challenging** and less efficient than open laparotomy for rapid control of hemorrhage and contamination.
*Abdominal ultrasound*
- An abdominal ultrasound (**FAST exam**) has already been partially performed, revealing free fluid and raising suspicion of free air, making further ultrasound redundant.
- While useful for initial trauma assessment, an ultrasound **cannot definitively rule out all abdominal injuries**, especially hollow viscus perforations or retroperitoneal hematomas, and is insufficient for unstable patients with clear signs of peritonitis.
*Diagnostic peritoneal lavage (DPL)*
- **DPL is largely replaced by FAST and CT scans** in most trauma centers, especially given the availability of imaging.
- Although it can detect intraperitoneal bleeding or perforation, it is an **invasive procedure** with potential complications and would only confirm what is already strongly suspected clinically; it does not address the need for immediate therapeutic intervention in an unstable patient.
*CT scan*
- A CT scan would be the imaging modality of choice for a **hemodynamically stable** patient with blunt abdominal trauma.
- However, performing a CT scan on an **unstable patient** would unnecessarily delay definitive surgical management, which is critical given the signs of ongoing internal bleeding and likely perforation.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 4: A 28-year-old man is brought to the emergency department with shortness of breath and chest pain, 35 minutes after he was involved in a high-speed motor vehicle collision. He was the helmeted driver of a scooter hit by a truck. On arrival, he is alert and oriented with a Glasgow Coma Scale rating of 14. His temperature is 37.3°C (99.1°F), pulse is 103/min, respirations are 33/min and blood pressure is 132/88 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Examination shows multiple abrasions over his abdomen and extremities. There is a 2.5-cm (1-in) laceration on the left side of the chest. There are decreased breath sounds over the left base. Cardiac examination shows no abnormalities. The abdomen is soft and there is tenderness to palpation over the left upper quadrant. Bowel sounds are normal. His hemoglobin concentration is 13.6 g/dL, leukocyte count is 9,110/mm3, and platelet count is 190,000/mm3. A chest x-ray is shown. Which of the following is the most likely diagnosis?
- A. Pneumothorax
- B. Phrenic nerve palsy
- C. Esophageal perforation
- D. Diaphragmatic rupture (Correct Answer)
- E. Diaphragmatic eventration
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Diaphragmatic rupture***
- The patient's history of **high-speed motor vehicle collision**, **shortness of breath**, **chest pain**, **decreased breath sounds at the left base**, and **abdominal tenderness in the left upper quadrant** (suggesting possible visceral herniation) are all highly consistent with a diaphragmatic rupture.
- A **chest X-ray** showing an elevated hemidiaphragm, abnormal bowel gas patterns in the chest, or gastric bubble in the thoracic cavity would further support this diagnosis, given the clinical context.
*Pneumothorax*
- While a **pneumothorax** can cause sudden shortness of breath and chest pain and decreased breath sounds, the presence of **left upper quadrant abdominal tenderness** and the mechanism of injury make diaphragmatic rupture more likely as the primary diagnosis.
- A pneumothorax would typically present with a collapsed lung on chest X-ray but would not explain the abdominal symptoms.
*Phrenic nerve palsy*
- **Phrenic nerve palsy** typically causes paralysis of the diaphragm, leading to respiratory compromise and an elevated hemidiaphragm on imaging, but it's usually **atraumatic** or a complication of surgery, not acute trauma.
- It would not explain the acute onset of pain and tenderness after a high-speed collision.
*Esophageal perforation*
- **Esophageal perforation** would cause severe chest pain, often radiating to the back, and can lead to mediastinitis, but it is less likely to present with decreased breath sounds at the base and left upper quadrant tenderness.
- A history of significant **vomiting** or **instrumentation** is often associated with esophageal perforation, which is absent here.
*Diaphragmatic eventration*
- **Diaphragmatic eventration** is a congenital thinning of the diaphragm leading to its elevation, but it is a **chronic condition** and would not present acutely after a high-speed collision.
- It is typically asymptomatic or causes chronic respiratory symptoms, not acute traumatic symptoms.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 5: A 24-year-old man is brought by ambulance to the emergency department after a motor vehicle accident. He was the front seat driver in a head on collision. He is currently unconscious. The patient’s past medical history is only notable for an allergy to amoxicillin as he developed a rash when it was given for a recent upper respiratory infection 1 week ago. Otherwise, he is a college student in good health. The patient is resuscitated. A FAST exam is notable for free fluid in Morrison’s pouch. An initial assessment demonstrates only minor bruises and scrapes on his body. After further resuscitation the patient becomes responsive and begins vomiting. Which of the following is the most likely diagnosis?
- A. Duodenal hematoma
- B. Rupture of the inferior vena cava
- C. No signs of internal trauma
- D. Laceration of the spleen
- E. Laceration of the liver (Correct Answer)
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Laceration of the liver***
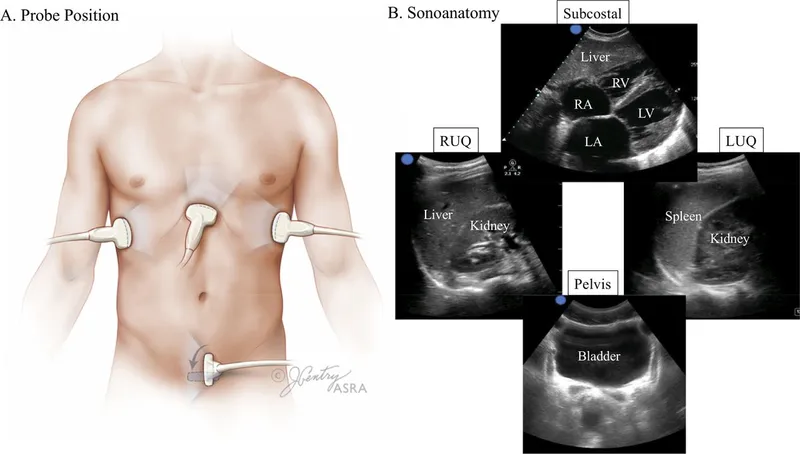
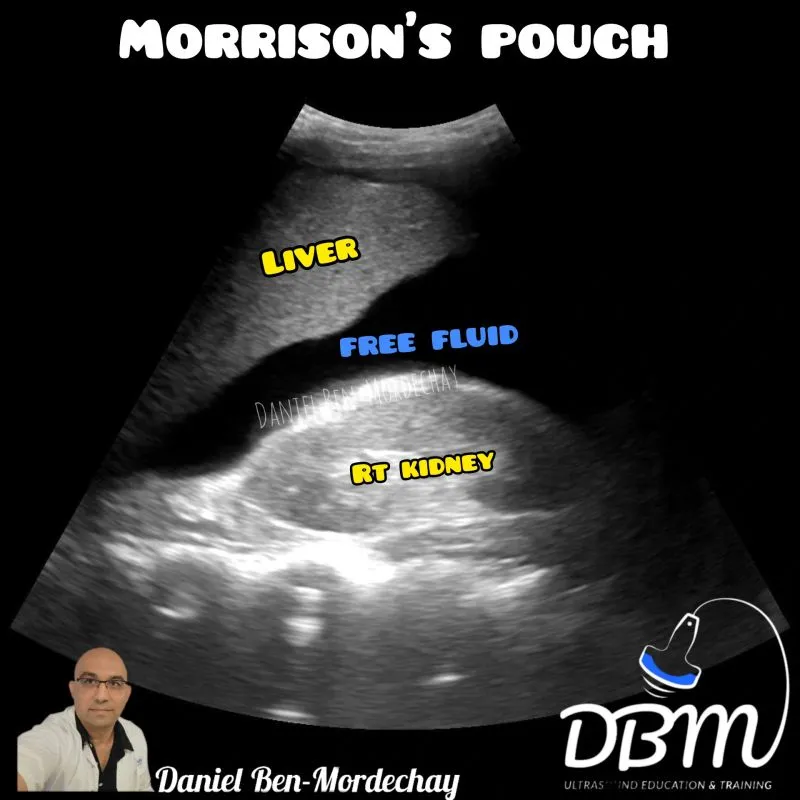
- **Morrison's pouch** (hepatorenal recess) is located between the **liver and right kidney** in the **right upper quadrant**, making it the primary collection site for blood from **liver injuries**.
- The presence of **free fluid in Morrison's pouch** on FAST exam is the classic finding for **hepatic trauma** with intraperitoneal bleeding.
- **Vomiting** after resuscitation can occur with significant abdominal trauma and irritation from blood in the peritoneal cavity.
- Liver lacerations are among the most common solid organ injuries in blunt abdominal trauma from motor vehicle accidents.
*Laceration of the spleen*
- While splenic injuries are common in blunt abdominal trauma, free fluid from splenic laceration typically collects in the **left upper quadrant** (splenorenal recess) or **left paracolic gutter** first, not primarily in Morrison's pouch.
- Morrison's pouch is anatomically distant from the spleen, making this a less likely diagnosis with this specific FAST finding.
*Duodenal hematoma*
- A duodenal hematoma typically presents with **gastric outlet obstruction symptoms** like epigastric pain and persistent vomiting days after injury.
- This injury is **retroperitoneal** and rarely causes significant **intraperitoneal free fluid** that would be detected in Morrison's pouch unless there is an associated perforation.
*Rupture of the inferior vena cava*
- A ruptured IVC would cause **massive retroperitoneal hemorrhage** and result in rapid circulatory collapse with profound shock.
- This is a **retroperitoneal structure**, so bleeding would not typically present as free intraperitoneal fluid in Morrison's pouch.
- The patient's ability to become responsive after resuscitation makes this catastrophic injury unlikely.
*No signs of internal trauma*
- The presence of **free fluid in Morrison's pouch** on FAST exam is definitive evidence of **intraperitoneal bleeding**, indicating significant internal trauma.
- This finding directly contradicts the statement of no internal trauma, making this option clearly incorrect.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 6: A 17-year-old adolescent male is brought to the emergency department by fire and rescue after being struck by a moving vehicle. The patient reports that he was running through his neighborhood when a car struck him while turning right on a red light. He denies any loss of consciousness. His temperature is 99.0°F (37.2°C), blood pressure is 88/56 mmHg, pulse is 121/min, respirations are 12/min, and SpO2 is 95% on room air. The patient is alert and oriented to person, place and time and is complaining of pain in his abdomen. He has lacerations on his face and extremities. On cardiac exam, he is tachycardic with normal S1 and S2. His lungs are clear to auscultation bilaterally, and his abdomen is soft but diffusely tender to palpation. The patient tenses his abdomen when an abdominal exam is performed. Bowel sounds are present, and he is moving all 4 extremities spontaneously. His skin is cool with delayed capillary refill. After the primary survey, 2 large-bore IVs are placed, and the patient is given a bolus of 2 liters of normal saline.
Which of the following is the best next step in management?
- A. Abdominal CT
- B. Diagnostic laparoscopy
- C. Diagnostic peritoneal lavage
- D. Focused Abdominal Sonography for Trauma (FAST) exam (Correct Answer)
- E. Emergency laparotomy
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Focused Abdominal Sonography for Trauma (FAST) exam***
- A **FAST exam** is the most appropriate next step in a hemodynamically unstable blunt trauma patient with suspected intra-abdominal injury after initial fluid resuscitation.
- It is a rapid, non-invasive, and repeatable bedside assessment that can quickly identify the presence of free fluid (blood) in the peritoneal, pericardial, or pleural spaces.
- **ATLS protocol:** In an unstable patient, a positive FAST exam confirms the need for immediate laparotomy without further imaging.
*Abdominal CT*
- An **abdominal CT** scan is generally the imaging modality of choice for hemodynamically stable blunt trauma patients to identify specific organ injuries.
- However, performing a CT on an **unstable patient** like this one would delay critical interventions and further destabilize them due to the need to transport them to the scanner.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a surgical procedure that is more invasive and time-consuming than a FAST exam.
- While it can identify injuries, it is typically reserved for hemodynamically stable patients when other non-invasive diagnostic tests are inconclusive or specific injuries are strongly suspected.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure with a high false-positive rate and has largely been replaced by the FAST exam and CT scans in blunt abdominal trauma.
- It involves inserting a catheter into the peritoneum to aspirate fluid, which is then analyzed for blood or other contents, but it is less specific for organ injury.
*Emergency laparotomy*
- An **emergency laparotomy** is the definitive surgical intervention for life-threatening intra-abdominal hemorrhage or organ injury.
- In this unstable patient, laparotomy would be performed immediately **after** a positive FAST exam confirms hemoperitoneum, or in cases of obvious peritonitis or hemodynamic collapse where the patient cannot wait even for FAST.
- Proceeding directly to laparotomy without FAST would bypass a rapid 2-3 minute diagnostic test that confirms the indication and location of bleeding.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 7: A 33-year-old man is brought to the emergency department because of trauma from a motor vehicle accident. His pulse is 122/min and rapid and thready, the blood pressure is 78/37 mm Hg, the respirations are 26/min, and the oxygen saturation is 90% on room air. On physical examination, the patient is drowsy, with cold and clammy skin. Abdominal examination shows ecchymoses in the right flank. The external genitalia are normal. No obvious external wounds are noted, and the rest of the systemic examination values are within normal limits. Blood is sent for laboratory testing and urinalysis shows 6 RBC/HPF. Hematocrit is 22% and serum creatinine is 1.1 mg/dL. Oxygen supplementation and IV fluid resuscitation are started immediately, but the hypotension persists. The focused assessment with sonography in trauma (FAST) examination shows a retroperitoneal fluid collection. What is the most appropriate next step in management?
- A. Perform an MRI scan of the abdomen and pelvis
- B. CT of the abdomen and pelvis with contrast
- C. Obtain a retrograde urethrogram
- D. Take the patient to the OR for an exploratory laparotomy (Correct Answer)
- E. Perform a diagnostic peritoneal lavage
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Take the patient to the OR for an exploratory laparotomy***
- The patient is **hemodynamically unstable** (BP 78/37 mm Hg, pulse 122/min) with signs of hemorrhagic shock (cold and clammy skin, drowsy, tachycardia) and **hypotension persists despite IV fluid resuscitation**.
- FAST examination shows **retroperitoneal fluid collection** (presumed blood), flank ecchymoses (Grey Turner sign), and hematocrit of 22% indicating **significant blood loss**.
- According to **ATLS (Advanced Trauma Life Support) protocols**, hemodynamically **unstable patients with positive FAST exams require immediate surgical intervention** and should not be delayed for further imaging.
- **Exploratory laparotomy** allows for immediate identification and control of bleeding sources, which is life-saving in this persistently hypotensive patient. The retroperitoneal hematoma can be explored and bleeding vessels ligated or repaired.
*CT of the abdomen and pelvis with contrast*
- CT scan is the **appropriate next step for hemodynamically STABLE trauma patients** or those who **respond to initial resuscitation** to characterize injuries and guide management.
- This patient has **persistent hypotension despite resuscitation**, making him too unstable to safely transport to the CT scanner. Delaying surgery for imaging in an unstable patient increases mortality risk.
- The principle is: **"Blood pressure is better than pictures"** - unstable patients need operative hemorrhage control, not diagnostic imaging.
*Perform an MRI scan of the abdomen and pelvis*
- **MRI has no role in acute trauma evaluation** due to long acquisition time (30-60 minutes), limited availability, and inability to adequately monitor critically ill patients in the MRI suite.
- This would be an inappropriate and potentially fatal delay in a patient with ongoing hemorrhage and hemodynamic instability.
*Perform a diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has been largely replaced by FAST examination for detecting intraperitoneal hemorrhage in the modern trauma algorithm.
- While DPL can detect intra-abdominal blood, the **FAST has already identified retroperitoneal fluid**, and the patient's persistent instability mandates immediate surgical intervention rather than additional diagnostic procedures.
- DPL also does not evaluate the retroperitoneum well and would not change management in this unstable patient.
*Obtain a retrograde urethrogram*
- **Retrograde urethrogram (RUG)** is indicated when urethral injury is suspected (blood at meatus, high-riding prostate, perineal hematoma, inability to void).
- This patient has **normal external genitalia** and only microscopic hematuria (6 RBC/HPF), which is nonspecific in blunt trauma.
- The immediate life-threatening issue is **hemorrhagic shock from retroperitoneal bleeding**, not potential urethral injury. RUG would be an inappropriate delay in management and can be performed later if clinically indicated.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 8: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 9: A 56-year-old man is brought to the emergency department after falling 16 feet from a ladder. He has severe pain in both his legs and his right arm. He appears pale and diaphoretic. His temperature is 37.5°C (99.5°F), pulse is 120/min and weak, respirations are 26/min, and blood pressure is 80/50 mm Hg. He opens his eyes and withdraws in response to painful stimuli and makes incomprehensible sounds. The abdomen is soft and nontender. All extremities are cold, with 1+ pulses distally. Arterial blood gas analysis on room air shows:
pH 7.29
PCO2 33 mm Hg
PO2 65 mm Hg
HCO3- 15 mEq/L
A CT scan shows displaced fractures of the pelvic ring, as well as fractures of both tibiae, the right distal radius, and right proximal humerus. The patient undergoes emergent open reduction and is admitted to the intensive care unit. Which of the following best indicates inadequate fluid resuscitation?
- A. Urine output of 25 mL in 3 hours (Correct Answer)
- B. Capillary refill time of 3 seconds
- C. Base deficit of 1 mmol/L
- D. Glasgow coma score of 8
- E. High pulse pressure
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Urine output of 25 mL in 3 hours***
- A critically low urine output of **less than 0.5 mL/kg/hr** (or <30 mL/hr in an adult) over several hours is a direct and sensitive indicator of **renal hypoperfusion** due to inadequate fluid resuscitation, especially in the context of traumatic shock.
- Oliguria suggests that the kidneys are not receiving sufficient blood flow to maintain normal function, indicating persistent systemic hypovolemia despite initial interventions.
*Capillary refill time of 3 seconds*
- A capillary refill time of 3 seconds, while slightly prolonged (normal <2 seconds), is less definitive for **severe ongoing hypovolemia** compared to oliguria.
- It can be influenced by factors like **ambient temperature** and peripheral vasoconstriction, which are common in trauma but may not solely reflect inadequate fluid volume.
*Base deficit of 1 mmol/L*
- A base deficit of 1 mmol/L is essentially **within the normal range** (typically -2 to +2 mmol/L).
- A normal or low base deficit suggests that **tissue perfusion is adequate** and there's no significant ongoing metabolic acidosis due to anaerobic metabolism, making it an indicator of *adequate* rather than *inadequate* resuscitation.
*Glasgow coma score of 8*
- A Glasgow Coma Scale (GCS) score of 8 (Eyes: 2, Verbal: 2, Motor: 4 from the stem) indicates **moderate head injury** or altered mental status.
- While hypovolemic shock can affect mentation, a GCS of 8 is more indicative of **neurological damage** (e.g., from head trauma sustained in the fall) or other systemic issues rather than being a primary measure of fluid resuscitation status.
*High pulse pressure*
- A high pulse pressure (the difference between systolic and diastolic blood pressure) is typically seen in conditions like **sepsis** or **aortic regurgitation**.
- In a patient with hypovolemic shock, **pulse pressure is usually narrowed** due to increased peripheral vascular resistance and decreased stroke volume.
Focused Assessment with Sonography in Trauma (FAST) US Medical PG Question 10: An 18-year-old man presents to the emergency department after an automobile accident. His vitals have significantly dropped since admission. Upon examination, his abdomen is slightly distended, the ribs on the right side are tender and appear broken, and breath sounds are diminished at the base of the right lung. An abdominal ultrasound and chest X-ray are ordered. Ultrasound shows fluid in the abdominal cavity and trauma to the liver. X-ray confirmed broken ribs and pleural effusion on the right. Based on these findings, the surgeons recommend immediate surgery. Upon entering the abdomen, an exsanguinating hemorrhage is observed. The Pringle maneuver is used to reduce bleeding. What was clamped during this maneuver?
- A. Aorta above celiac axis
- B. Splenic artery only
- C. Hepatic artery only
- D. Hepatic vein only
- E. Hepatoduodenal ligament (Correct Answer)
Focused Assessment with Sonography in Trauma (FAST) Explanation: ***Hepatoduodenal ligament***
- The **Pringle maneuver** involves clamping the **hepatoduodenal ligament** to control bleeding from the liver. This ligament contains the **hepatic artery**, **portal vein**, and **bile duct**.
- Clamping the hepatoduodenal ligament effectively stops blood flow into the liver, allowing for temporary control of hemorrhage during hepatic trauma repair.
*Aorta above celiac axis*
- Clamping the **aorta above the celiac axis** would severely compromise blood flow to multiple vital organs, including the stomach, spleen, and most of the intestines, leading to widespread ischemia.
- This is a much more extensive and dangerous clamping maneuver typically reserved for massive intra-abdominal hemorrhage not controllable by other means, rather than liver-specific bleeding.
*Splenic artery only*
- Clamping the **splenic artery** would only stop blood flow to the spleen and would not significantly impact bleeding from the liver.
- The described trauma is to the liver, so addressing the splenic artery would not be the primary intervention for a liver hemorrhage.
*Hepatic artery only*
- While clamping the **hepatic artery** would reduce arterial blood flow to the liver, the liver also receives a significant blood supply from the portal vein.
- Therefore, clamping only the hepatic artery would not completely stop the blood flow into the liver, making it less effective than the Pringle maneuver (which includes the portal vein).
*Hepatic vein only*
- Clamping the **hepatic vein** would obstruct blood outflow from the liver, leading to **hepatic venous congestion**, but it would not stop the inflow of blood from the hepatic artery and portal vein.
- This would worsen rather than control an exsanguinating hemorrhage from a liver injury.
More Focused Assessment with Sonography in Trauma (FAST) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.