Extremity trauma and vascular injuries US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Extremity trauma and vascular injuries. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Extremity trauma and vascular injuries US Medical PG Question 1: A 21-year-old man presents to the emergency department after sustaining a stab wound to the neck at a local farmer's market. The patient is otherwise healthy and is complaining of pain. The patient is able to offer the history himself. His temperature is 97.6°F (36.4°C), blood pressure is 120/84 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam demonstrates a 3 cm laceration 1 cm inferior to the mastoid process on the right side. The patient's breath sounds are clear and he is protecting his airway. No stridor or difficulty breathing is noted. Which of the following is the most appropriate next step in the management of this patient?
- A. Observation and blood pressure monitoring
- B. Intubation
- C. CT angiogram (Correct Answer)
- D. Surgical exploration
Extremity trauma and vascular injuries Explanation: ***CT angiogram***
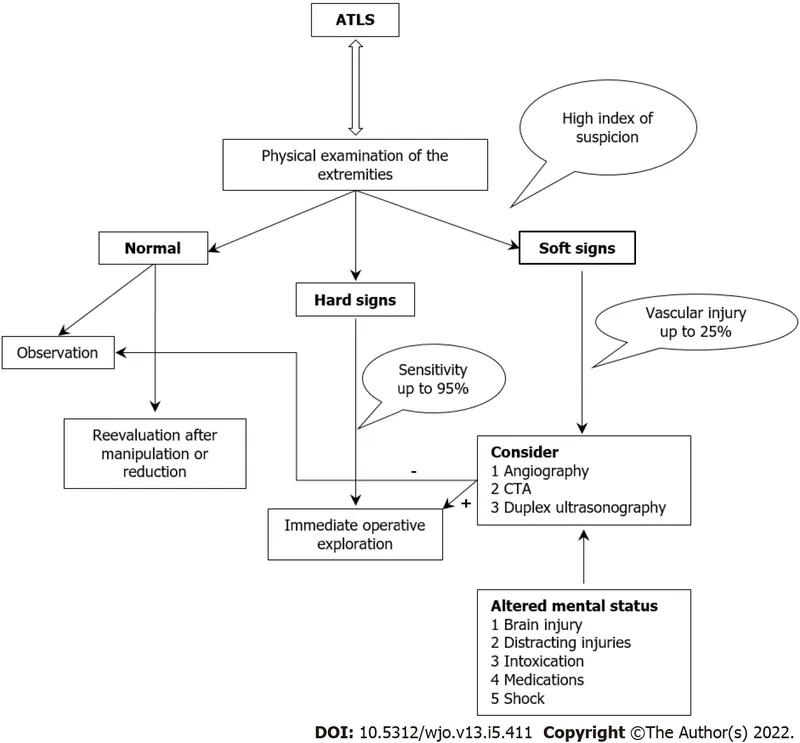
- A **CT angiogram (CTA)** is the most appropriate next step given the location of the stab wound, which is close to vital neurovascular structures, particularly the **carotid and vertebral arteries**.
- CTA is a **non-invasive** and rapid imaging modality that can effectively rule out or confirm vascular injuries, guide further management, and avoid unnecessary surgical exploration.
*Observation and blood pressure monitoring*
- While initial observation is important, relying solely on it for a penetration injury near major vessels is **insufficient** and could lead to delayed diagnosis of potentially life-threatening vascular damage.
- Although the patient is currently **hemodynamically stable**, vascular injuries can present with delayed symptoms and require more definitive diagnostic evaluation.
*Intubation*
- The patient has no signs of airway compromise, such as **stridor, difficulty breathing, or impaired oxygenation**.
- **Prophylactic intubation** is not indicated as it carries risks and is only performed when there is an immediate or impending threat to the airway.
*Surgical exploration*
- **Surgical exploration** is an invasive procedure and should be reserved for cases where there is clear evidence of vascular injury or when less invasive diagnostics like CTA are unavailable or inconclusive.
- In a stable patient, **non-invasive imaging** should precede surgery unless there are hard signs of vascular compromise (e.g., pulsatile bleeding, expanding hematoma, thrill/bruit).
Extremity trauma and vascular injuries US Medical PG Question 2: A 22-year-old man presents to the emergency department after being tackled in a game of football. The patient was hit from behind and fell to the ground. After the event, he complained of severe pain in his knee. The patient has a past medical history of anabolic steroid use. His current medications include whey protein supplements, multivitamins, and fish oil. His temperature is 99.5°F (37.5°C), blood pressure is 137/68 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you see a muscular young man clutching his knee in pain. The knee is inflamed and erythematous. When valgus stress is applied to the leg, there is some laxity when compared to the contralateral leg. The patient is requesting surgery for his injury. Arthrocentesis is performed and demonstrates no abnormalities of the synovial fluid. Which of the following physical exam findings is most likely to be seen in this patient?
- A. Anterior displacement of the femur relative to the tibia
- B. Severe pain with compression of the patella
- C. Anterior displacement of the tibia relative to the femur
- D. A palpable click with passive motion of the knee (Correct Answer)
- E. Laxity to varus stress
Extremity trauma and vascular injuries Explanation: ***A palpable click with passive motion of the knee***
- The patient's presentation with a **football injury**, **severe knee pain**, **inflammation**, and **laxity with valgus stress** (suggesting MCL injury) points towards significant knee trauma. A palpable click can indicate a torn meniscus, which is a common accompanying injury in such forceful knee trauma, particularly with a simultaneous MCL tear.
- While the primary injury might involve ligaments, the absence of synovial fluid abnormalities upon arthrocentesis makes a pure ligamentous tear without associated meniscal damage less likely to produce a palpable click, and given the forceful impact, meniscal injury is highly probable.
*Anterior displacement of the femur relative to the tibia*
- This finding would indicate a **posterior cruciate ligament (PCL) injury**, which typically results from a direct blow to the tibiofemoral joint while the knee is in flexion, or a hyperextension injury.
- The mechanism described (hit from behind with valgus stress) and the laxity to valgus stress are not consistent with a PCL injury.
*Severe pain with compression of the patella*
- Severe pain with patellar compression is characteristic of **patellofemoral pain syndrome** or **chondromalacia patellae**, which are typically overuse injuries or degenerative conditions.
- This finding is less likely to be the primary presentation following acute, forceful traumatic injury to the knee resulting in ligamentous laxity.
*Anterior displacement of the tibia relative to the femur*
- This is the classic sign of an **anterior cruciate ligament (ACL) tear**, which is tested using the **Lachman test** or **anterior drawer test**.
- While an ACL tear can occur in football, the described injury mechanism ("hit from behind" and "valgus stress") is more indicative of MCL damage, and an isolated ACL tear does not directly correlate with the valgus laxity observed.
*Laxity to varus stress*
- Laxity to varus stress indicates an injury to the **lateral collateral ligament (LCL)**.
- The clinical presentation specifically mentions laxity with **valgus stress**, which points to a medial collateral ligament (MCL) injury, not an LCL injury.
Extremity trauma and vascular injuries US Medical PG Question 3: A 45-year-old man was a driver in a motor vehicle collision. The patient is not able to offer a medical history during initial presentation. His temperature is 97.6°F (36.4°C), blood pressure is 104/74 mmHg, pulse is 150/min, respirations are 12/min, and oxygen saturation is 98% on room air. On exam, he does not open his eyes, he withdraws to pain, and he makes incomprehensible sounds. He has obvious signs of trauma to the chest and abdomen. His abdomen is distended and markedly tender to palpation. He also has an obvious open deformity of the left femur. What is the best initial step in management?
- A. Emergency open fracture repair
- B. Packed red blood cells
- C. Exploratory laparotomy
- D. Intubation (Correct Answer)
- E. 100% oxygen
Extremity trauma and vascular injuries Explanation: ***Intubation***
- The patient's **Glasgow Coma Scale (GCS) score is 7** (E=1, V=2, M=4), which is below 8 and indicates a severe head injury needing **airway protection** via intubation.
- A GCS ≤ 8 mandates **definitive airway management** to prevent aspiration and ensure adequate ventilation.
*Emergency open fracture repair*
- While the patient has an open femur fracture, it is not the most immediate life-threatening concern after a major trauma; **airway and breathing** take precedence.
- **Hemorrhage control** and **stabilization** often precede definitive orthopedic repair in polytrauma.
*Packed red blood cells*
- Although the patient is likely in **hemorrhagic shock** (tachycardia, hypotension, obvious trauma), administering blood products without first securing the airway is not the initial priority.
- **Circulation** management, including fluid resuscitation and blood products, follows **airway and breathing** establishment.
*Exploratory laparotomy*
- The patient's distended and tender abdomen strongly suggests intra-abdominal injury, but this is a **diagnostic and therapeutic procedure** that comes after initial resuscitation and stabilization.
- **Emergent laparotomy** for abdominal trauma is considered once the patient's airway, breathing, and circulation are secured.
*100% oxygen*
- Administering 100% oxygen is part of initial resuscitation, but it does not address the fundamental problem of an unsecured airway and the risk of **hypoventilation** or **aspiration** in a patient with a GCS of 7.
- Oxygen supplementation helps improve saturation in spontaneously breathing patients but cannot protect a compromised airway.
Extremity trauma and vascular injuries US Medical PG Question 4: A 27-year-old male presents to the Emergency Room as a code trauma after being shot in the neck. En route, the patient's blood pressure is 127/73 mmHg, pulse is 91/min, respirations are 14/min, and oxygen saturation is 100% on room air with GCS of 15. On physical exam, the patient is in no acute distress; however, there is an obvious entry point with oozing blood near the left lateral neck above the cricoid cartilage with a small hematoma that is non-pulsatile and stable since arrival. The rest of the physical exam is unremarkable. Rapid hemoglobin returns back at 14.1 g/dL. After initial resuscitation, what is the next best step in management?
- A. Bedside neck exploration
- B. Conventional angiography
- C. MRI
- D. Plain radiography films
- E. CT angiography (Correct Answer)
Extremity trauma and vascular injuries Explanation: ***CT angiography***
- **CT angiography** is the most appropriate next step for **stable patients** with penetrating neck trauma, like this patient, to evaluate for vascular and airway injuries.
- It offers **rapid, non-invasive assessment** of the extent of injury and helps guide further management.
*Bedside neck exploration*
- **Bedside neck exploration** is typically reserved for patients with **hard signs** of vascular injury (e.g., active hemorrhage, expanding hematoma, pulsatile hematoma) or **signs of airway compromise**, which are absent here.
- This patient is **hemodynamically stable** and has a non-expanding hematoma.
*Conventional angiography*
- **Conventional angiography** is more **invasive** and time-consuming than CTA, carrying risks such as arterial dissection or stroke.
- It is usually reserved for **diagnostic confirmation** or **therapeutic intervention** (e.g., embolization) after initial imaging, especially when CTA findings are equivocal or reveal treatable lesions.
*MRI*
- **MRI** is generally **contraindicated** in acute trauma situations, especially when the presence of metallic foreign bodies (e.g., bullet fragments) is a concern.
- Its **longer acquisition time** and **lack of immediate availability** in the emergency setting make it less suitable for initial evaluation of penetrating neck trauma.
*Plain radiography films*
- **Plain radiographs** can identify **bony fractures** and the general location of foreign bodies, but they offer **limited information** regarding soft tissue and vascular structures.
- They are insufficient for comprehensively evaluating potential vascular or airway injuries in penetrating neck trauma.
Extremity trauma and vascular injuries US Medical PG Question 5: A 50-year-old man presents to the emergency department with pain and swelling of his right leg for the past 2 days. Three days ago he collapsed on his leg after tripping on a rug. It was a hard fall and left him with bruising of his leg. Since then the pain and swelling of his leg have been gradually increasing. Past medical history is noncontributory. He lives a rather sedentary life and smokes two packs of cigarettes per day. The vital signs include heart rate 98/min, respiratory rate 15/min, temperature 37.8°C (100.1°F), and blood pressure 100/60 mm Hg. On physical examination, his right leg is visibly swollen up to the mid-calf with pitting edema and moderate erythema. Peripheral pulses in the right leg are weak and the leg is tender. Manipulation of the right leg is negative for Homan’s sign. What is the next best step in the management of this patient?
- A. Send the patient to surgery for an emergency fasciotomy
- B. Start intravenous heparin therapy immediately
- C. Make a diagnosis of deep vein thrombosis based on history and physical
- D. Perform a venous ultrasound (Correct Answer)
- E. Perform intravenous venography within 24 hours
Extremity trauma and vascular injuries Explanation: ***Perform a venous ultrasound***
- The patient's presentation with acute unilateral leg swelling, pain, erythema, and weak peripheral pulses following trauma, along with **risk factors for venous thromboembolism (sedentary lifestyle, smoking)**, strongly suggests the possibility of a **deep vein thrombosis (DVT)**.
- **Venous ultrasound** is the **most appropriate and preferred initial diagnostic test** for suspected DVT due to its **non-invasiveness, accessibility, and high sensitivity and specificity**.
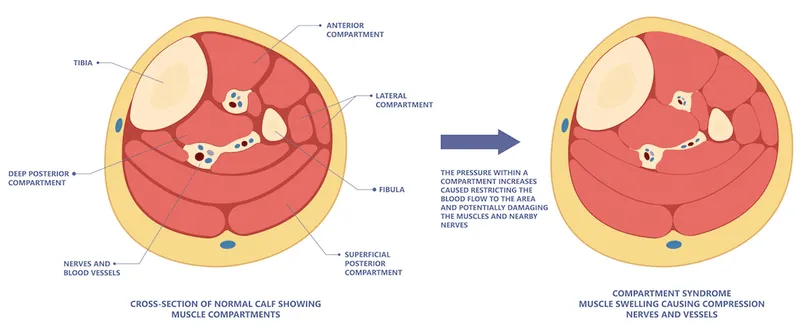
*Send the patient to surgery for an emergency fasciotomy*
- **Fasciotomy** is indicated for **acute compartment syndrome**, which typically presents with severe pain out of proportion to injury, pain on passive stretch, paresthesia, and tense compartments.
- While the patient has swelling and tenderness, the weak pulses are concerning, but the overall picture does not definitively point to compartment syndrome needing immediate fasciotomy without further diagnostic workup.
*Start intravenous heparin therapy immediately*
- Though DVT is suspected, **heparin therapy should not be initiated empirically without definitive diagnostic confirmation** due to the risk of bleeding complications.
- A **venous ultrasound is crucial to confirm the diagnosis** before starting anticoagulation.
*Make a diagnosis of deep vein thrombosis based on history and physical*
- While the clinical picture is highly suggestive of DVT, **clinical diagnosis alone is not sufficiently accurate** to initiate potentially risky treatments like anticoagulation.
- **Objective diagnostic testing (like ultrasound)** is essential to confirm the presence of a DVT.
*Perform intravenous venography within 24 hours*
- **Intravenous venography** is considered the **gold standard** for diagnosing DVT, but it is an **invasive procedure** with risks (e.g., contrast nephropathy, allergic reactions, radiation exposure).
- It is **rarely used as a first-line diagnostic test** and is usually reserved for cases where ultrasound results are inconclusive or discordant with clinical suspicion.
Extremity trauma and vascular injuries US Medical PG Question 6: A 19-year-old man comes to the emergency department for right wrist pain and swelling 2 hours after falling on an outstretched hand while playing softball. The pain worsened when he attempted to pitch after the fall. He has eczema and type 1 diabetes mellitus. Current medications include insulin and topical clobetasol. He appears uncomfortable. Examination shows multiple lichenified lesions over his forearms. The right wrist is swollen and tender; range of motion is limited by pain. There is tenderness to palpation in the area between the tendons of the abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus muscle. The thumb can be opposed actively towards the other fingers. Muscle strength of the right hand is decreased. Which of the following is the most likely diagnosis?
- A. De Quervain's tenosynovitis
- B. Colles' fracture
- C. Transscaphoid perilunate dislocation
- D. Scaphoid fracture (Correct Answer)
- E. Lunate dislocation
Extremity trauma and vascular injuries Explanation: ***Scaphoid fracture***
- The history of a **fall on an outstretched hand (FOOSH)**, especially when attempting to pitch again, combined with **tenderness in the anatomical snuffbox** (area between the tendons of the abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus muscle), is highly indicative of a **scaphoid fracture**.
- **Limited range of motion** and decreased muscle strength due to pain, even with active thumb opposition, further supports this diagnosis.
*De Quervain's tenosynovitis*
- This is an **inflammatory condition** affecting the tendons on the thumb side of the wrist, typically exacerbated by repetitive thumb movements.
- While it can cause pain in a similar area, it usually develops gradually and is not immediately precipitated by an acute **FOOSH injury**.
*Colles' fracture*
- A **Colles' fracture** involves a fracture of the **distal radius** with dorsal displacement, often presenting with a "dinner fork" deformity.
- While it also results from a **FOOSH injury**, the key finding of **anatomical snuffbox tenderness** points away from a Colles' fracture and towards a scaphoid injury.
*Transscaphoid perilunate dislocation*
- This severe injury involves a **dislocation of the carpal bones** around the lunate, often with an associated scaphoid fracture.
- While a scaphoid fracture is part of this, the primary presentation would involve more obvious **carpal instability** and significant radiographic abnormalities beyond a simple scaphoid fracture.
*Lunate dislocation*
- A **lunate dislocation** involves the displacement of the lunate bone, typically volarly, and often presents with a characteristic "spilled teacup" sign on radiographs.
- Although it can result from a **FOOSH injury**, the specific finding of **anatomical snuffbox tenderness** is more indicative of a scaphoid fracture.
Extremity trauma and vascular injuries US Medical PG Question 7: A 53-year-old Asian woman comes to the physician because of a 2-month history of severe pain in her right leg while walking. She used to be able to walk a half-mile (800-m) to the grocery store but has been unable to walk 200 meters without stopping because of the pain over the past month. She can continue to walk after a break of around 5 minutes. She has hypertension, atrial fibrillation, and type 2 diabetes mellitus. She has smoked one pack of cigarettes daily for the past 32 years. Current medications include metformin, enalapril, aspirin, and warfarin. Vital signs are within normal limits. Examination shows an irregularly irregular pulse. The right lower extremity is cooler than the left lower extremity. The skin over the right leg appears shiny and dry. Femoral pulses are palpated bilaterally; pedal pulses are diminished on the right side. Which of the following is the most appropriate next step in management?
- A. MRI spine screening
- B. Duplex ultrasonography
- C. Ankle-brachial index (Correct Answer)
- D. Nerve conduction studies
- E. Biopsy of tibial artery
Extremity trauma and vascular injuries Explanation: ***Ankle-brachial index***
- The patient's symptoms of **intermittent claudication** (leg pain with exertion relieved by rest) and risk factors (smoking, diabetes, atrial fibrillation, hypertension) are highly suggestive of **peripheral artery disease (PAD)**. The **ankle-brachial index (ABI)** is the most appropriate initial diagnostic step as it is a quick, non-invasive, and reliable test to screen for PAD by comparing blood pressure in the ankles to blood pressure in the arms.
- A **diminished pedal pulse** on the right side and **cooler, shiny, dry skin** further support the suspicion of PAD, making ABI crucial for confirming the diagnosis and assessing its severity.
*MRI spine screening*
- While spinal pathology can cause leg pain, symptoms like **neurogenic claudication** typically improve with leaning forward or sitting and are not consistently relieved by standing still. The patient's pain relief with rest after walking points away from spinal stenosis.
- The patient's specific peripheral signs like a **cooler leg**, **diminished pedal pulses**, and **trophic changes** are not typical findings for spinal compression.
*Duplex ultrasonography*
- **Duplex ultrasonography** is a more advanced imaging technique used to visualize the blood vessels and assess blood flow, typically performed *after* an abnormal ABI confirms the presence of PAD.
- It helps in **localizing stenoses** and assessing their severity, but it is not the primary diagnostic screening tool in the initial evaluation of suspected PAD.
*Nerve conduction studies*
- **Nerve conduction studies (NCS)** are used to diagnose neuropathies. While diabetes is a risk factor for neuropathy, the patient's symptoms are classic for **vascular claudication** (pain with exertion, relieved by rest), rather than neuropathic pain, which is often described as burning, tingling, or numbing and does not typically resolve promptly with rest.
- The physical exam findings of a **cool leg** and **diminished pulses** are not consistent with a primary neurological problem.
*Biopsy of tibial artery*
- A **biopsy of the tibial artery** is an invasive procedure generally reserved for specific types of vasculitis (e.g., giant cell arteritis, polyarteritis nodosa) when other less invasive diagnostics have been inconclusive or raised suspicion for these conditions.
- It is not indicated for the initial workup of suspected **atherosclerotic peripheral artery disease**, which is the most likely diagnosis given the patient's risk factors and symptoms.
Extremity trauma and vascular injuries US Medical PG Question 8: A crying 4-year-old child is brought to the emergency department with a red, swollen knee. He was in his usual state of health until yesterday, when he sustained a fall in the sandbox at the local park. His mother saw it happen; she says he was walking through the sandbox, fell gently onto his right knee, did not cry or seem alarmed, and returned to playing without a problem. However, later that night, his knee became red and swollen. It is now painful and difficult to move. The child’s medical history is notable for frequent bruising and prolonged bleeding after circumcision. On physical exam, his knee is erythematous, tender, and swollen, with a limited range of motion. Arthrocentesis aspirates frank blood from the joint. Which of the following single tests is most likely to be abnormal in this patient?
- A. Prothrombin time (PT)
- B. Bleeding time
- C. Complete blood count
- D. Platelet aggregation studies
- E. Partial thromboplastin time (PTT) (Correct Answer)
Extremity trauma and vascular injuries Explanation: ***Partial thromboplastin time (PTT)***
- This patient's presentation with **hemarthrosis** (frank blood in the joint after minor trauma), easy bruising, and prolonged bleeding after circumcision suggests a **coagulation factor deficiency**, most commonly hemophilia.
- The **PTT** measures the integrity of the **intrinsic** and common coagulation pathways; deficiencies in factors VIII, IX, XI, or XII, which cause hemophilia A or B, prolong the PTT.
*Prothrombin time (PT)*
- The **PT** primarily assesses the **extrinsic** and common coagulation pathways, which involve factors VII, X, V, II, and fibrinogen.
- In hemophilia A or B, the extrinsic pathway is typically unaffected, so the PT would remain **normal**.
*Bleeding time*
- **Bleeding time** assesses **platelet function** and **vascular integrity**, which would be abnormal in conditions like thrombocytopenia or von Willebrand disease.
- This patient's symptoms are more consistent with a coagulation factor deficiency rather than a primary platelet disorder.
*Complete blood count*
- A **CBC** evaluates cell counts (red blood cells, white blood cells, platelets) and hemoglobin/hematocrit.
- While it might show **anemia** if there has been significant blood loss, it would not directly identify a specific coagulation factor deficiency or be the most likely test to be abnormal in a clotting disorder of this nature.
*Platelet aggregation studies*
- **Platelet aggregation studies** are used to diagnose disorders of **platelet function**, such as Glanzmann thrombasthenia or Bernard-Soulier syndrome.
- The clinical picture strongly points to a **factor deficiency** (e.g., hemophilia) causing severe bleeding into the joint, rather than a primary platelet aggregation defect.
Extremity trauma and vascular injuries US Medical PG Question 9: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Extremity trauma and vascular injuries Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Extremity trauma and vascular injuries US Medical PG Question 10: A 33-year-old woman presents to the emergency department with pain in her right wrist. She says she was walking on the sidewalk a few hours ago when she suddenly slipped and landed forcefully on her outstretched right hand with her palm facing down. The patient is afebrile, and vital signs are within normal limits. Physical examination of her right wrist shows mild edema and tenderness on the lateral side of the right hand with a decreased range of motion. Sensation is intact. The patient is able to make a fist and OK sign with her right hand. A plain radiograph of her right wrist is shown in the image. Which of the following bones is most likely fractured in this patient?
- A. Bone labeled 'A'
- B. Bone labeled 'D' (Correct Answer)
- C. Bone labeled 'C'
- D. Bone labeled 'E'
- E. Bone labeled 'B'
Extremity trauma and vascular injuries Explanation: ***Bone labeled 'D'***
- The clinical presentation of a fall on an **outstretched hand (FOOSH)** with pain on the **lateral aspect** of the wrist suggests a **scaphoid fracture**.
- Bone 'D' is the **scaphoid bone**, which is commonly fractured in this mechanism due to its position and poor blood supply, making it prone to **avascular necrosis** if untreated.
*Bone labeled 'A'*
- Bone 'A' is the **ulna**, which is less commonly fractured due to FOOSH injuries unless there is a direct impact or significant rotational force.
- While it articulates with the wrist, a fracture of the ulna would typically present with pain more medially and potentially forearm instability.
*Bone labeled 'C'*
- Bone 'C' is the first **metacarpal**, part of the thumb, which is distal to the wrist joint.
- A fracture here would cause pain more specifically localised to the thumb base rather than the general wrist area as described.
*Bone labeled 'E'*
- Bone 'E' is the **hamate bone**, located in the distal carpal row.
- Fractures of the hamate are less common than scaphoid fractures via FOOSH and are often associated with direct impact (e.g., from a golf club) or forceful gripping.
*Bone labeled 'B'*
- Bone 'B' represents the **radius**, specifically its distal portion. While a **Colles fracture** of the distal radius is common with FOOSH, the tenderness being on the "lateral side of the right hand" specifically points away from a general distal radius fracture and more towards the carpal bones, particularly the scaphoid.
- A Colles fracture often results in a **"dinner fork" deformity**, which is not mentioned in the presentation, and tenderness would be more widespread over the distal forearm.
More Extremity trauma and vascular injuries US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.