Blunt abdominal trauma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Blunt abdominal trauma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Blunt abdominal trauma US Medical PG Question 1: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Blunt abdominal trauma Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
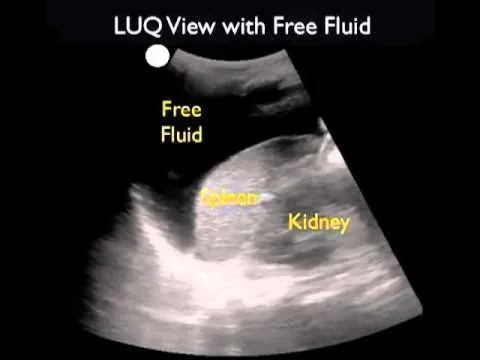
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
Blunt abdominal trauma US Medical PG Question 2: A 41-year-old man is admitted to the emergency room after being struck in the abdomen by a large cement plate while transporting it. On initial assessment by paramedics at the scene, his blood pressure was 110/80 mm Hg, heart rate 85/min, with no signs of respiratory distress. On admission, the patient is alert but in distress. He complains of severe, diffuse, abdominal pain and severe weakness. Vital signs are now: blood pressure 90/50 mm Hg, heart rate 96/min, respiratory rate 19/min, temperature 37.4℃ (99.3℉), and oxygen saturation of 95% on room air. His lungs are clear on auscultation. The cardiac exam is significant for a narrow pulse pressure. Abdominal examination reveals a large bruise over the epigastric and periumbilical regions. The abdomen is distended and there is diffuse tenderness to palpation with rebound and guarding, worst in the epigastric region. There is hyperresonance to percussion in the epigastric region and absence of hepatic dullness in the right upper quadrant. Aspiration of the nasogastric tube reveals bloody contents. Focused assessment with sonography for trauma (FAST) shows free fluid in the pelvic region. Evaluation of the perisplenic and perihepatic regions is impossible due to the presence of free air. Aggressive intravenous fluid resuscitation is administered but fails to improve upon the patient’s hemodynamics. Which of the following is the next best step in management?
- A. Emergency laparoscopy
- B. Abdominal ultrasound
- C. Diagnostic peritoneal lavage (DPL)
- D. Emergency laparotomy (Correct Answer)
- E. CT scan
Blunt abdominal trauma Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** unresponsive to fluid resuscitation, coupled with clear signs of **perforation** (hyperresonance, absent hepatic dullness, free air on FAST limited view). This clinical picture is a direct indication for immediate surgical intervention.
- The presence of bloody nasogastric tube contents, diffuse tenderness with rebound and guarding, and a history of significant blunt trauma further support the need for urgent exploratory **laparotomy** to identify and repair the source of injury.
*Emergency laparoscopy*
- While laparoscopy can be used for abdominal exploration, it is **contraindicated in hemodynamically unstable patients** due to the need for pneumoperitoneum, which can further compromise cardiovascular stability.
- In cases of suspected visceral perforation with extensive free air and massive bleeding, **laparoscopy may be technically challenging** and less efficient than open laparotomy for rapid control of hemorrhage and contamination.
*Abdominal ultrasound*
- An abdominal ultrasound (**FAST exam**) has already been partially performed, revealing free fluid and raising suspicion of free air, making further ultrasound redundant.
- While useful for initial trauma assessment, an ultrasound **cannot definitively rule out all abdominal injuries**, especially hollow viscus perforations or retroperitoneal hematomas, and is insufficient for unstable patients with clear signs of peritonitis.
*Diagnostic peritoneal lavage (DPL)*
- **DPL is largely replaced by FAST and CT scans** in most trauma centers, especially given the availability of imaging.
- Although it can detect intraperitoneal bleeding or perforation, it is an **invasive procedure** with potential complications and would only confirm what is already strongly suspected clinically; it does not address the need for immediate therapeutic intervention in an unstable patient.
*CT scan*
- A CT scan would be the imaging modality of choice for a **hemodynamically stable** patient with blunt abdominal trauma.
- However, performing a CT scan on an **unstable patient** would unnecessarily delay definitive surgical management, which is critical given the signs of ongoing internal bleeding and likely perforation.
Blunt abdominal trauma US Medical PG Question 3: A 34-year-old man is admitted to the emergency department after a motor vehicle accident in which he sustained blunt abdominal trauma. On admission, he is conscious, has a GCS score of 15, and has normal ventilation with no signs of airway obstruction. Vitals initially are blood pressure 95/65 mmHg, heart rate 87/min, respiratory rate 14/min, and oxygen saturation of 95% on room air. The physical exam is significant only for tenderness to palpation over the left flank. Noncontrast CT of the abdomen shows fractures of the 9th and 10th left ribs. Intravenous fluids are administered and the patient's blood pressure increases to 110/80 mm Hg. Three days later after admission, the patient suddenly complains of weakness and left upper quadrant (LUQ) pain. Vitals are blood pressure 80/50 mm Hg, heart rate 97/min, respiratory rate 18/min, temperature 36.2℃ (97.2℉) and oxygen saturation of 99% on room air. Prompt administration of 2L of IV fluids increases the blood pressure to 100/70 mm Hg. On physical exam, there is dullness to percussion and rebound tenderness with guarding in the LUQ. Bowel sounds are present. Raising the patient's left leg results in pain in his left shoulder. Stat hemoglobin level is 9.8 g/dL. Which of the following findings would be most likely seen if a CT scan were performed now?
- A. Subdiaphragmatic air collection
- B. Low-density areas within the splenic parenchyma (Correct Answer)
- C. Heterogeneous parenchymal enhancement of the pancreatic tail
- D. Herniation of the stomach into the thoracic cavity
- E. Irregular linear areas of hypoattenuation in the liver parenchyma
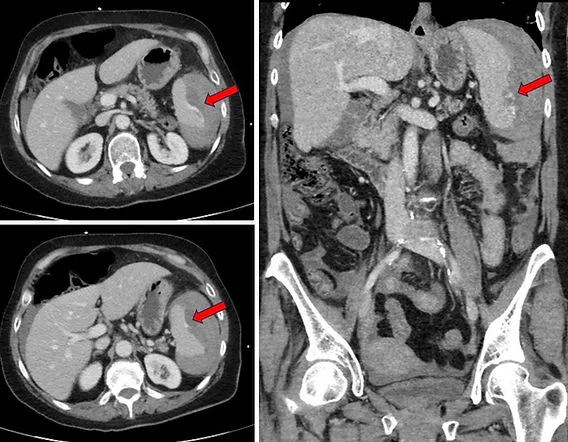
Blunt abdominal trauma Explanation: **Low-density areas within the splenic parenchyma**
- The patient's history of trauma, initial left rib fractures, LUQ pain, and **Kehr's sign** (left shoulder pain from diaphragmatic irritation), followed by sudden decompensation and anemia, are highly indicative of **delayed splenic rupture**.
- On CT scan, **low-density areas** (fluid collections or hematomas) within the splenic parenchyma or around the spleen are characteristic findings of splenic injury and rupture, including intraparenchymal hematomas or subcapsular hematomas.
*Subdiaphragmatic air collection*
- This finding suggests a **perforated viscus**, such as the stomach or intestine, allowing air to escape into the peritoneal cavity.
- While blunt trauma can cause hollow organ injury, the patient's symptoms (Kehr's sign, LUQ pain, initial rib fractures) and the delayed presentation of hypovolemic shock are more consistent with splenic rupture than perforation.
*Heterogeneous parenchymal enhancement of the pancreatic tail*
- This symptom is indicative of **pancreatic injury**, which can occur with blunt abdominal trauma, especially with rapid deceleration.
- However, the patient's presentation, particularly the prominent Kehr's sign and the context of left rib fractures, points more strongly towards splenic involvement rather than primary pancreatic injury.
*Herniation of the stomach into the thoracic cavity*
- This describes a **diaphragmatic rupture**, which can occur in severe blunt trauma and lead to gastric herniation.
- While possible with severe trauma, the immediate presentation of **Kehr's sign** and the progressive symptoms are more characteristic of splenic rupture than an acute diaphragmatic hernia with gastric displacement.
*Irregular linear areas of hypoattenuation in the liver parenchyma*
- These findings suggest **hepatic lacerations** or hematomas, indicating liver injury.
- Although liver injury is a common finding in blunt abdominal trauma, the patient's specific presentation of **left-sided pain**, **left shoulder pain**, and left rib fractures points preferentially to **splenic injury** rather than liver injury.
Blunt abdominal trauma US Medical PG Question 4: A 24-year-old man is brought by ambulance to the emergency department after a motor vehicle accident. He was the front seat driver in a head on collision. He is currently unconscious. The patient’s past medical history is only notable for an allergy to amoxicillin as he developed a rash when it was given for a recent upper respiratory infection 1 week ago. Otherwise, he is a college student in good health. The patient is resuscitated. A FAST exam is notable for free fluid in Morrison’s pouch. An initial assessment demonstrates only minor bruises and scrapes on his body. After further resuscitation the patient becomes responsive and begins vomiting. Which of the following is the most likely diagnosis?
- A. Duodenal hematoma
- B. Rupture of the inferior vena cava
- C. No signs of internal trauma
- D. Laceration of the spleen
- E. Laceration of the liver (Correct Answer)
Blunt abdominal trauma Explanation: ***Laceration of the liver***
- **Morrison's pouch** (hepatorenal recess) is located between the **liver and right kidney** in the **right upper quadrant**, making it the primary collection site for blood from **liver injuries**.
- The presence of **free fluid in Morrison's pouch** on FAST exam is the classic finding for **hepatic trauma** with intraperitoneal bleeding.
- **Vomiting** after resuscitation can occur with significant abdominal trauma and irritation from blood in the peritoneal cavity.
- Liver lacerations are among the most common solid organ injuries in blunt abdominal trauma from motor vehicle accidents.
*Laceration of the spleen*
- While splenic injuries are common in blunt abdominal trauma, free fluid from splenic laceration typically collects in the **left upper quadrant** (splenorenal recess) or **left paracolic gutter** first, not primarily in Morrison's pouch.
- Morrison's pouch is anatomically distant from the spleen, making this a less likely diagnosis with this specific FAST finding.
*Duodenal hematoma*
- A duodenal hematoma typically presents with **gastric outlet obstruction symptoms** like epigastric pain and persistent vomiting days after injury.
- This injury is **retroperitoneal** and rarely causes significant **intraperitoneal free fluid** that would be detected in Morrison's pouch unless there is an associated perforation.
*Rupture of the inferior vena cava*
- A ruptured IVC would cause **massive retroperitoneal hemorrhage** and result in rapid circulatory collapse with profound shock.
- This is a **retroperitoneal structure**, so bleeding would not typically present as free intraperitoneal fluid in Morrison's pouch.
- The patient's ability to become responsive after resuscitation makes this catastrophic injury unlikely.
*No signs of internal trauma*
- The presence of **free fluid in Morrison's pouch** on FAST exam is definitive evidence of **intraperitoneal bleeding**, indicating significant internal trauma.
- This finding directly contradicts the statement of no internal trauma, making this option clearly incorrect.
Blunt abdominal trauma US Medical PG Question 5: A previously healthy 27-year-old man is brought to the emergency department 35 minutes after being involved in a high-speed motor vehicle collision in which he was an unrestrained passenger. He was ambulatory at the accident scene, with stable vital signs and no major external injuries except abrasions to both upper extremities. On arrival, he is alert and oriented. His temperature is 37.3°C (99.1°F), pulse is 88/min, respirations are 14/min, and blood pressure is 128/74 mm Hg. Abdominal examination shows ecchymosis over the upper abdomen, with tenderness to palpation over the left upper quadrant. There is no guarding or rigidity. Rectal examination is unremarkable. A CT scan of the abdomen with intravenous contrast shows a subcapsular splenic hematoma comprising 8% of the surface area, with no contrast extravasation and minimal blood in the peritoneal cavity. Which of the following is the next best step in management?
- A. Discharge home and follow up closely
- B. Coil embolization of short gastric vessels
- C. Exploratory laparotomy and splenectomy
- D. Hospitalization and frequent ultrasounds (Correct Answer)
- E. Laparoscopic splenectomy
Blunt abdominal trauma Explanation: ***Hospitalization and frequent ultrasounds***
- The patient has a **small, contained splenic hematoma** (grade I-II) and remains **hemodynamically stable**, which are key indicators for **nonoperative management (NOM)** in blunt splenic trauma. Frequent ultrasounds can monitor for expansion of the hematoma or development of free fluid.
- **Serial physical exams** and **vital signs monitoring** are crucial to detect any signs of splenic injury progression or hemodynamic instability, which would necessitate a change in management.
*Discharge home and follow up closely*
- Discharging a patient with a documented **splenic hematoma**, even if small and stable, carries a significant risk of **delayed rupture** or progression of the injury, making it an unsafe initial management strategy.
- While the patient is currently stable, internal bleeding can worsen rapidly, requiring close observation in a hospital setting for at least 24-48 hours.
*Coil embolization of short gastric vessels*
- **Angioembolization** is typically indicated for **higher-grade splenic injuries** (grades III-V), active contrast extravasation, pseudoaneurysms, or continued bleeding despite nonoperative management.
- In this case, there is **no contrast extravasation** and the injury is low-grade, making embolization an overly aggressive first-line intervention.
*Exploratory laparotomy and splenectomy*
- **Laparotomy** and **splenectomy** are reserved for patients with **hemodynamic instability** that doesn't respond to resuscitation, signs of ongoing significant hemorrhage, or higher-grade injuries unsuitable for nonoperative management.
- The patient is currently **hemodynamically stable** and has a low-grade splenic injury, making immediate surgery unnecessary and potentially leading to higher morbidity without clear benefit.
*Laparoscopic splenectomy*
- Similar to open splenectomy, **laparoscopic splenectomy** is a surgical intervention used for significant splenic injuries that fail nonoperative management or cause hemodynamic instability.
- Given the patient's **stable condition** and low-grade injury, immediate surgical removal of the spleen is not indicated and would remove the opportunity for spleen preservation.
Blunt abdominal trauma US Medical PG Question 6: A 43-year-old man is brought to the emergency department 30 minutes after falling from the roof of a construction site. He reports abdominal and right-sided flank pain. His temperature is 37.1°C (98.8°F), pulse is 114/min, and blood pressure is 100/68 mm Hg. Physical examination shows numerous ecchymoses over the trunk and flanks and a tender right abdomen without a palpable mass. Focused assessment with sonography for trauma (FAST) shows no intraperitoneal fluid collections. His hemoglobin concentration is 7.6 g/dL. The most likely cause of his presentation is injury to which of the following organs?
- A. Liver
- B. Kidney (Correct Answer)
- C. Stomach
- D. Small bowel
- E. Spleen
Blunt abdominal trauma Explanation: ***Kidney***
- The patient's presentation with **flank pain**, **ecchymoses over the flank**, and **hypotension** following a fall from height is highly suggestive of **renal injury**. The absence of intraperitoneal fluid on FAST scan further supports an injury to a retroperitoneal organ like the kidney.
- The **significantly decreased hemoglobin (7.6 g/dL)** indicates substantial blood loss, which is consistent with the vascular nature of the kidney and potential for severe hemorrhage following trauma.
*Liver*
- While liver injury can cause **hypotension** and **abdominal pain** after trauma, the primary pain would typically be in the **right upper quadrant**, not specifically the flank.
- Liver injuries often result in **intraperitoneal fluid collections** (hemoperitoneum), which were explicitly absent on the FAST scan in this patient.
*Stomach*
- Stomach injuries typically result from penetrating trauma or severe blunt force, leading to **peritonitis** and potential **gastric content leakage**, which would cause diffuse abdominal pain and potentially peritonitis signs.
- It is an **intraperitoneal organ**, and injury might be seen on a FAST scan as free fluid, which is not present here.
*Small bowel*
- Small bowel injuries typically present with **diffuse abdominal pain**, **peritoneal signs**, and can lead to **sepsis** due to contamination.
- These injuries often cause **intraperitoneal fluid** or air, neither of which is reported.
*Spleen*
- Splenic injuries typically cause **left upper quadrant pain** and can lead to significant **intraperitoneal bleeding**, which would be detected by a FAST scan.
- The patient's symptoms are localized to the **right side** and flank, making splenic injury less likely.
Blunt abdominal trauma US Medical PG Question 7: A 33-year-old man is brought to the emergency department because of trauma from a motor vehicle accident. His pulse is 122/min and rapid and thready, the blood pressure is 78/37 mm Hg, the respirations are 26/min, and the oxygen saturation is 90% on room air. On physical examination, the patient is drowsy, with cold and clammy skin. Abdominal examination shows ecchymoses in the right flank. The external genitalia are normal. No obvious external wounds are noted, and the rest of the systemic examination values are within normal limits. Blood is sent for laboratory testing and urinalysis shows 6 RBC/HPF. Hematocrit is 22% and serum creatinine is 1.1 mg/dL. Oxygen supplementation and IV fluid resuscitation are started immediately, but the hypotension persists. The focused assessment with sonography in trauma (FAST) examination shows a retroperitoneal fluid collection. What is the most appropriate next step in management?
- A. Perform an MRI scan of the abdomen and pelvis
- B. CT of the abdomen and pelvis with contrast
- C. Obtain a retrograde urethrogram
- D. Take the patient to the OR for an exploratory laparotomy (Correct Answer)
- E. Perform a diagnostic peritoneal lavage
Blunt abdominal trauma Explanation: ***Take the patient to the OR for an exploratory laparotomy***
- The patient is **hemodynamically unstable** (BP 78/37 mm Hg, pulse 122/min) with signs of hemorrhagic shock (cold and clammy skin, drowsy, tachycardia) and **hypotension persists despite IV fluid resuscitation**.
- FAST examination shows **retroperitoneal fluid collection** (presumed blood), flank ecchymoses (Grey Turner sign), and hematocrit of 22% indicating **significant blood loss**.
- According to **ATLS (Advanced Trauma Life Support) protocols**, hemodynamically **unstable patients with positive FAST exams require immediate surgical intervention** and should not be delayed for further imaging.
- **Exploratory laparotomy** allows for immediate identification and control of bleeding sources, which is life-saving in this persistently hypotensive patient. The retroperitoneal hematoma can be explored and bleeding vessels ligated or repaired.
*CT of the abdomen and pelvis with contrast*
- CT scan is the **appropriate next step for hemodynamically STABLE trauma patients** or those who **respond to initial resuscitation** to characterize injuries and guide management.
- This patient has **persistent hypotension despite resuscitation**, making him too unstable to safely transport to the CT scanner. Delaying surgery for imaging in an unstable patient increases mortality risk.
- The principle is: **"Blood pressure is better than pictures"** - unstable patients need operative hemorrhage control, not diagnostic imaging.
*Perform an MRI scan of the abdomen and pelvis*
- **MRI has no role in acute trauma evaluation** due to long acquisition time (30-60 minutes), limited availability, and inability to adequately monitor critically ill patients in the MRI suite.
- This would be an inappropriate and potentially fatal delay in a patient with ongoing hemorrhage and hemodynamic instability.
*Perform a diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has been largely replaced by FAST examination for detecting intraperitoneal hemorrhage in the modern trauma algorithm.
- While DPL can detect intra-abdominal blood, the **FAST has already identified retroperitoneal fluid**, and the patient's persistent instability mandates immediate surgical intervention rather than additional diagnostic procedures.
- DPL also does not evaluate the retroperitoneum well and would not change management in this unstable patient.
*Obtain a retrograde urethrogram*
- **Retrograde urethrogram (RUG)** is indicated when urethral injury is suspected (blood at meatus, high-riding prostate, perineal hematoma, inability to void).
- This patient has **normal external genitalia** and only microscopic hematuria (6 RBC/HPF), which is nonspecific in blunt trauma.
- The immediate life-threatening issue is **hemorrhagic shock from retroperitoneal bleeding**, not potential urethral injury. RUG would be an inappropriate delay in management and can be performed later if clinically indicated.
Blunt abdominal trauma US Medical PG Question 8: A 37-year-old woman is brought to the emergency department 15 minutes after falling down a flight of stairs. On arrival, she has shortness of breath, right-sided chest pain, right upper quadrant abdominal pain, and right shoulder pain. She is otherwise healthy. She takes no medications. She appears pale. Her temperature is 37°C (98.6°F), pulse is 115/min, respirations are 20/min, and blood pressure is 85/45 mm Hg. Examination shows several ecchymoses over the right chest. There is tenderness to palpation over the right chest wall and right upper quadrant of the abdomen. Bowel sounds are normal. Cardiopulmonary examination shows no abnormalities. Neck veins are flat. Which of the following is the most likely diagnosis?
- A. Splenic laceration
- B. Liver hematoma (Correct Answer)
- C. Pneumothorax
- D. Duodenal hematoma
- E. Small bowel perforation
Blunt abdominal trauma Explanation: ***Liver hematoma***
- The patient's presentation with **right upper quadrant abdominal pain**, **right shoulder pain** (referred pain from diaphragmatic irritation), and **hypotension** following a fall points strongly to **liver injury**.
- The liver is the **most commonly injured organ** in blunt abdominal trauma due to its size and position.
*Splenic laceration*
- While splenic laceration can cause hypovolemic shock, pain is typically localized to the **left upper quadrant** and left shoulder (**Kehr's sign**), not the right.
- The ecchymoses and tenderness are predominantly on the **right side** of the chest and abdomen.
*Pneumothorax*
- A pneumothorax would typically present with **unilateral diminished breath sounds**, **hyperresonance to percussion**, and potentially **tracheal deviation**, none of which are mentioned.
- The patient's **blood pressure is low**, which is more suggestive of significant hemorrhage than an isolated pneumothorax, especially with **flat neck veins**.
*Duodenal hematoma*
- A duodenal hematoma typically presents with **epigastric pain**, **vomiting**, and symptoms of **gastric outlet obstruction**, often days after the injury.
- It does not typically cause **referred shoulder pain** or immediate **hypovolemic shock** as seen here.
*Small bowel perforation*
- Small bowel perforation would present with signs of **peritonitis**, such as **rebound tenderness**, **guarding**, and absent or diminished bowel sounds due to inflammation from bowel contents.
- While there is abdominal pain, the **bowel sounds are normal**, and the primary symptoms align more with **hemorrhage**.
Blunt abdominal trauma US Medical PG Question 9: A 33-year-old man is brought to the emergency department 20 minutes after losing control over his bicycle and colliding with a parked car. The handlebar of the bicycle hit his lower abdomen. On arrival, he is alert and oriented. His pulse is 90/min, respirations are 17/min and blood pressure is 110/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. The pupils are equal and reactive to light. There are multiple bruises over his chest and lower extremities. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. There is no pelvic instability. Rectal examination is unremarkable. A complete blood count, prothrombin time, and serum concentrations of glucose, creatinine, and electrolytes are within the reference range. Urine dipstick is mildly positive for blood. Microscopic examination of the urine shows 20 RBCs/hpf. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. Laparotomy
- C. Observation and follow-up
- D. Suprapubic catheterization
- E. CT scan of the abdomen and pelvis (Correct Answer)
Blunt abdominal trauma Explanation: ***CT scan of the abdomen and pelvis***
- This patient has suffered significant trauma to the lower abdomen, as indicated by colliding with a parked car and handlebar impact, along with **hematuria** (urine dipstick positive for blood, 20 RBCs/hpf).
- A CT scan of the abdomen and pelvis is crucial to assess for potential **intra-abdominal organ injury**, particularly to the kidneys, bladder, or bowel, given the mechanism of injury and the presence of hematuria.
*Intravenous pyelography*
- While IVP can visualize the urinary tract, it is generally **less sensitive and specific** than CT scanning for detecting trauma-related urinary tract injuries and concurrent injuries to other abdominal organs.
- Furthermore, modern trauma care primarily utilizes **CT scanning** due to its superior anatomical detail and ability to assess multiple organ systems simultaneously.
*Laparotomy*
- **Exploratory laparotomy** is a surgical procedure indicated for patients with signs of **hemodynamic instability**, peritonitis, or clear evidence of severe intra-abdominal injury, none of which are present in this hemodynamically stable patient.
- Performing a laparotomy without further diagnostic imaging in a stable patient is premature and carries unnecessary risks.
*Observation and follow-up*
- While the patient is currently hemodynamically stable and the abdomen is soft and non-tender, the **mechanism of injury** (handlebar impact to the lower abdomen) combined with **hematuria** suggests a high likelihood of significant internal injury that requires further evaluation.
- **Observation alone** without imaging could lead to delayed diagnosis and treatment of a potentially serious injury to the urinary tract or other abdominal organs.
*Suprapubic catheterization*
- **Suprapubic catheterization** is used to drain the bladder when urethral catheterization is not possible or contraindicated, for example in cases of suspected urethral injury.
- There is no indication of urethral injury here (**unremarkable rectal exam**, no gross blood at the meatus), and the primary concern is evaluation of the organs, not bladder drainage.
Blunt abdominal trauma US Medical PG Question 10: A 27-year-old-man is brought to the emergency department 30 minutes after being involved in a motorcycle accident. He lost control at high speed and was thrown forward onto the handlebars. On arrival, he is alert and responsive. He has abdominal pain and superficial lacerations on his left arm. Vital signs are within normal limits. Examination shows a tender, erythematous area over his epigastrium. The abdomen is soft and non-distended. A CT scan of the abdomen shows no abnormalities. Treatment with analgesics is begun, the lacerations are cleaned and dressed, and the patient is discharged home after 2 hours of observation. Four days later, the patient returns to the emergency department with gradually worsening upper abdominal pain, fever, poor appetite, and vomiting. His pulse is 91/min and blood pressure is 135/82 mm Hg. Which of the following is the most likely diagnosis?
- A. Abdominal compartment syndrome
- B. Aortic dissection
- C. Splenic rupture
- D. Pancreatic ductal injury (Correct Answer)
- E. Diaphragmatic rupture
Blunt abdominal trauma Explanation: ***Pancreatic ductal injury***
- A forceful impact to the **epigastrium** (e.g., falling onto handlebars) can cause **pancreatic injury**, particularly a **ductal transection**, due to the pancreas being compressed against the vertebral column.
- Initial CT scans can be normal because the injury to the **ductal system** takes time to manifest, leading to delayed symptoms like **worsening abdominal pain, fever, vomiting**, and **poor appetite** several days later due to **pancreatitis** or a **pseudocyst** formation.
*Abdominal compartment syndrome*
- This typically presents with **acute abdominal distension**, increased intra-abdominal pressure, and organ dysfunction (e.g., oliguria, respiratory compromise), which are not described here.
- It's an immediate complication of severe trauma or fluid resuscitation, not a delayed presentation like described.
*Aortic dissection*
- Characterized by **sudden-onset, severe, tearing chest or back pain** and often involves hypertension or Marfan syndrome.
- It would manifest immediately with hemodynamic instability and distinct pain, not a delayed presentation of progressive abdominal symptoms.
*Splenic rupture*
- Often causes **left upper quadrant pain**, **Kehr's sign** (referred shoulder pain), and **hemodynamic instability** due to significant blood loss.
- While possible in trauma, a normal initial CT scan makes this less likely, and its symptoms usually appear earlier or are more severe.
*Diaphragmatic rupture*
- Can present with **dyspnea, shoulder pain**, or signs of **herniated abdominal organs** into the chest.
- It causes more immediate respiratory distress or gastrointestinal obstruction symptoms, and the abdominal symptoms described are not typical for this injury.
More Blunt abdominal trauma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.