Trauma/Emergencies

On this page
🚨 The Trauma Command Center: Emergency Response Mastery
Trauma care compresses months of medical decision-making into minutes, where your ability to recognize patterns, prioritize interventions, and synthesize across organ systems determines whether a patient survives or deteriorates. You'll master the systematic frameworks that transform chaos into controlled response-from understanding the body's physiological cascade during injury to building diagnostic discrimination skills and executing evidence-based treatment protocols. This lesson equips you with the command center mindset and pattern recognition tools that define expert emergency clinicians who act decisively when seconds matter most.
The trauma response system operates on time-critical algorithms where the first 60 minutes (the "Golden Hour") determine survival outcomes. Understanding these systematic approaches enables rapid pattern recognition and prevents the cognitive overload that leads to missed diagnoses in 25% of complex trauma cases.
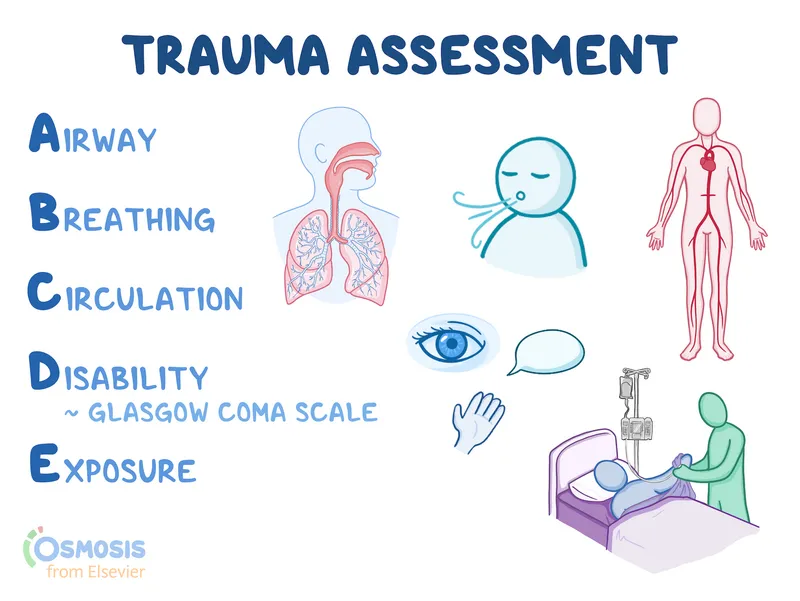
📌 Remember: ABCDE - Airway with C-spine, Breathing, Circulation, Disability, Exposure - Each step has <2 minute assessment windows in unstable patients
Trauma Response Hierarchy
-
Immediate Threats (0-5 minutes)
- Airway obstruction: >90% mortality if unrecognized
- Tension pneumothorax: 100% fatal without decompression
- Massive hemorrhage: >40% blood loss = 80% mortality
- External bleeding: Direct pressure controls 85%
- Internal bleeding: Requires surgical intervention <1 hour
- Pelvic fractures: Blood loss 2-4 liters average
-
Life-Threatening Injuries (5-15 minutes)
- Hemothorax: >1500mL initial drainage = thoracotomy
- Cardiac tamponade: Beck's triad present in only 10%
- Flail chest: ≥3 ribs fractured in ≥2 places
- Paradoxical movement with <60% normal ventilation
- Underlying pulmonary contusion in 75% of cases
-
Potentially Life-Threatening (15-60 minutes)
- Pulmonary contusion: Develops over 24-48 hours
- Myocardial contusion: CK-MB elevation in 15%
- Diaphragmatic rupture: Left-sided in 90% of cases
| Priority Level | Time Window | Mortality Risk | Key Interventions | Success Rate |
|---|---|---|---|---|
| Immediate | 0-5 min | >80% if delayed | Airway, decompression, hemorrhage control | 95% if rapid |
| Urgent | 5-15 min | 40-60% | Chest tubes, fluid resuscitation, imaging | 85% survival |
| Delayed | 15-60 min | 10-25% | Definitive repair, monitoring | 90% survival |
| Minimal | >60 min | <5% | Observation, outpatient follow-up | 98% survival |
| Expectant | Variable | >95% | Comfort care, family support | Palliative |
💡 Master This: The "Lethal Triad" of trauma - Hypothermia (<35°C), Acidosis (pH <7.2), and Coagulopathy (INR >1.5) creates a death spiral with >80% mortality when all three present
Understanding trauma triage principles establishes the foundation for recognizing injury patterns that guide systematic assessment and intervention priorities.
🚨 The Trauma Command Center: Emergency Response Mastery
⚡ The Physiological Storm: Trauma's Cascade Response
Shock Classification Physiology
-
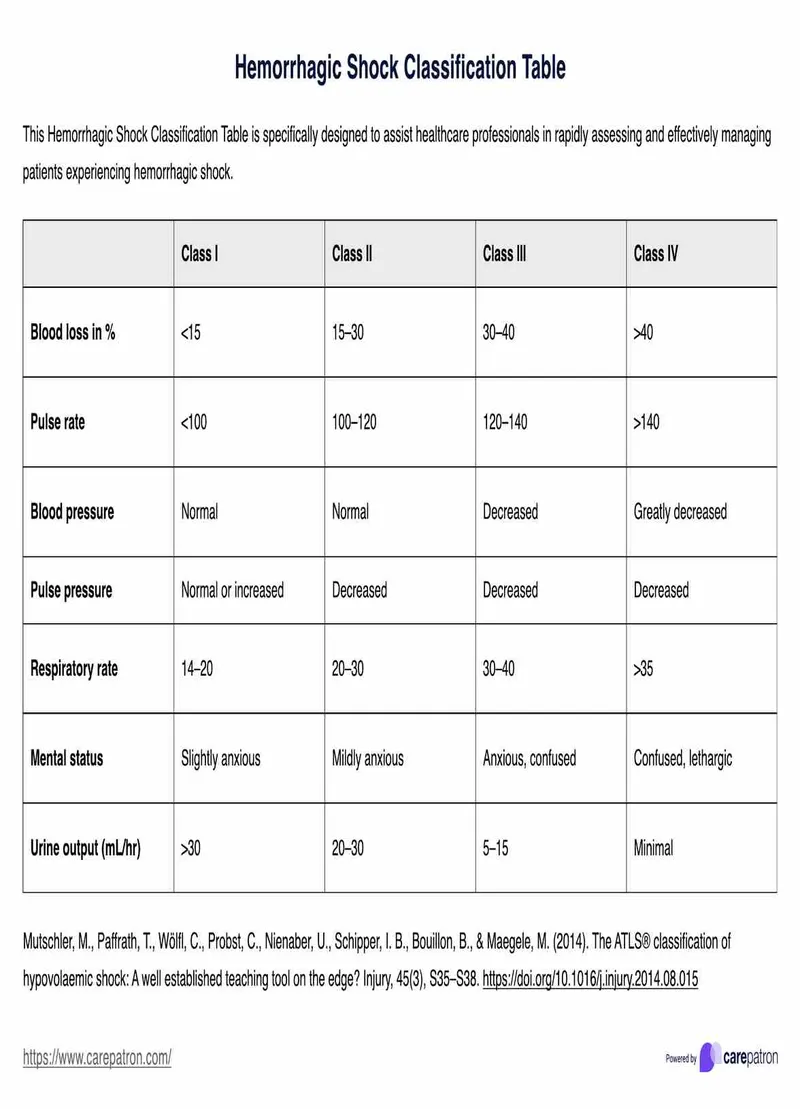
Class I Hemorrhage (<15% blood loss, <750mL)
- Heart rate: <100 bpm (normal compensatory response)
- Blood pressure: Normal (vasoconstriction maintains perfusion)
- Pulse pressure: Normal or slightly ↓
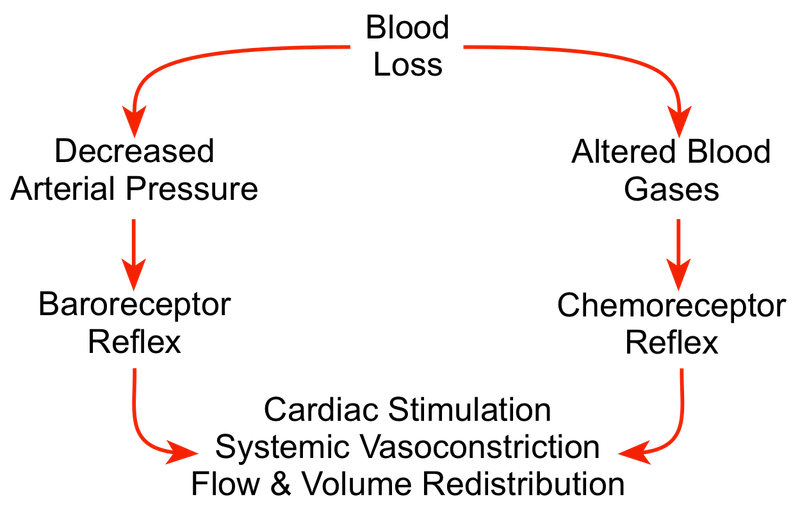
- Sympathetic activation maintains cardiac output
- Peripheral vasoconstriction preserves central circulation
- Urine output: >30mL/hr (adequate renal perfusion)
-
Class II Hemorrhage (15-30% loss, 750-1500mL)
- Heart rate: 100-120 bpm (compensatory tachycardia)
- Blood pressure: Normal (maximal compensation)
- Pulse pressure: ↓ (decreased stroke volume)
- Anxiety and restlessness from catecholamine surge
- Capillary refill: 2-3 seconds (delayed but present)
- Urine output: 20-30mL/hr (mild oliguria)
📌 Remember: HARM - Heart rate ↑, Anxiety, Restlessness, Mild oliguria characterize Class II shock compensation
-
Class III Hemorrhage (30-40% loss, 1500-2000mL)
- Heart rate: 120-140 bpm (marked tachycardia)
- Blood pressure: ↓ (compensation failing)
- Mental status: Confused (cerebral hypoperfusion)
- Skin: Cool, clammy (maximal vasoconstriction)
- Capillary refill: >3 seconds (poor perfusion)
- Urine output: 5-15mL/hr (significant oliguria)
-
Class IV Hemorrhage (>40% loss, >2000mL)
- Heart rate: >140 bpm or bradycardia (pre-terminal)
- Blood pressure: Severely ↓ (systolic <70 mmHg)
- Mental status: Lethargic to unconscious
- Skin: Cold, pale (peripheral shutdown)
- Capillary refill: Absent (no peripheral perfusion)
- Urine output: Negligible (renal failure imminent)
| Shock Class | Blood Loss | Heart Rate | Systolic BP | Mental Status | Urine Output | Mortality |
|---|---|---|---|---|---|---|
| I | <15% (<750mL) | <100 | Normal | Alert | >30mL/hr | <5% |
| II | 15-30% (750-1500mL) | 100-120 | Normal | Anxious | 20-30mL/hr | 10-15% |
| III | 30-40% (1500-2000mL) | 120-140 | Decreased | Confused | 5-15mL/hr | 35-40% |
| IV | >40% (>2000mL) | >140 | Severely ↓ | Lethargic | Negligible | >80% |
💡 Master This: Compensated shock can maintain normal blood pressure until 30% blood volume lost - Tachycardia and anxiety are the earliest reliable signs of significant hemorrhage
Understanding shock physiology reveals why systematic assessment protocols detect life-threatening injuries before obvious clinical deterioration occurs.
⚡ The Physiological Storm: Trauma's Cascade Response
🎯 The Pattern Recognition Matrix: Clinical Decision Frameworks
Mechanism-Based Injury Prediction
- Motor Vehicle Collision Patterns
-
Frontal impact: Predictable "down and under" vs "up and over" pathways
- Down-under: Knee-femur-hip-pelvis injury sequence (65% of cases)
- Up-over: Head-cervical spine-thorax injury pattern (35% of cases)
- Steering wheel contact: Cardiac contusion risk (15% incidence)
- Dashboard impact: Posterior hip dislocation (85% with knee trauma)
-
Side impact: Lateral compression injury patterns
- Ipsilateral injuries: Shoulder-ribs-pelvis-femur (90% same side)
- Contralateral head injury: Coup-contrecoup mechanism (25%)
- Aortic injury risk: 3x higher than frontal impact
- Splenic injury: Left-sided impact (70% incidence)
-
Rear impact: Hyperextension-hyperflexion sequence
- Cervical spine injury: C5-C6 most common level (40%)
- Delayed symptom onset: 24-48 hours typical
- Whiplash syndrome: >6 months symptoms in 15%
-
📌 Remember: DRIVE - Down-under pathway, Rear hyperextension, Ipsilateral side impact, Vertical compression, Ejection = 5x mortality
Fall Pattern Recognition
-
Fall Height Correlation
- <10 feet: Extremity injuries predominate (75%)
- 10-20 feet: Calcaneus-spine-wrist triad ("Don Juan" syndrome)
- >20 feet: Multi-system trauma (85% require surgery)
- Landing position determines injury pattern
- Feet-first: Bilateral calcaneus → lumbar spine (60%)
- Head-first: Cervical spine → brain injury (90% fatal)
-
Pediatric Fall Considerations
- Head-heavy body proportion changes injury patterns
- >3x body height = significant injury risk
- Subdural hematoma more common than adults (3:1 ratio)
- Non-accidental trauma consideration with inconsistent mechanism
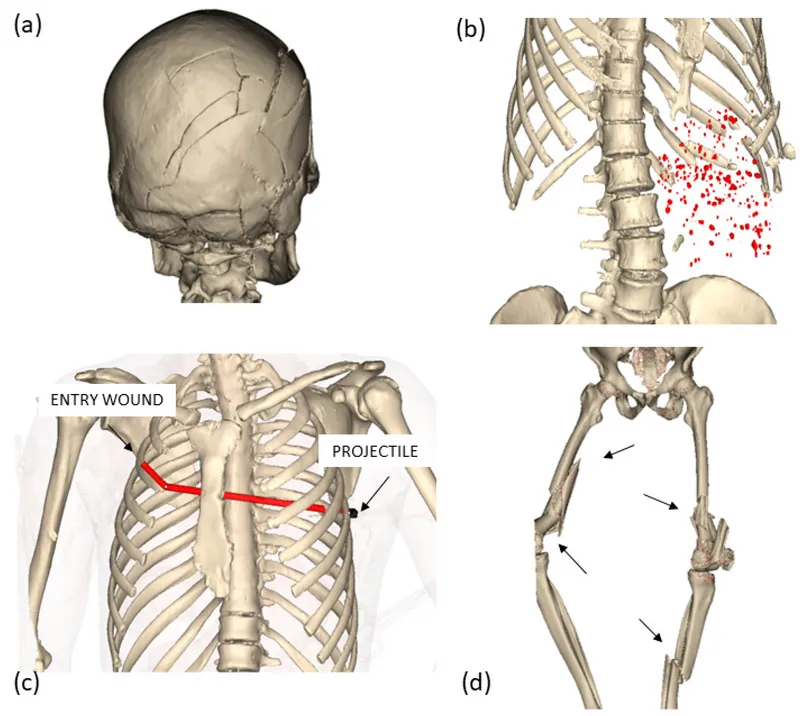
Penetrating Trauma Algorithms
- Gunshot Wound Assessment
- High-velocity (>2000 ft/sec): Cavitation injury 5x bullet diameter
- Low-velocity (<1000 ft/sec): Direct tissue destruction only
- Trajectory mapping: Entry + exit + anatomical path
- Abdominal GSW: Exploratory laparotomy if peritoneal violation
- Chest GSW: Hemothorax in 85%, pneumothorax in 95%
- Head GSW: Mortality >90% if bihemispheric or ventricular
| Mechanism | Primary Injuries | Secondary Injuries | Mortality Risk | Key Assessment |
|---|---|---|---|---|
| Frontal MVC | Head, chest, abdomen | Cervical spine, extremities | 15-25% | Steering wheel deformity |
| Side MVC | Ipsilateral torso | Contralateral head | 20-30% | Door intrusion >12 inches |
| Fall >20ft | Axial skeleton | Visceral organs | 35-45% | Landing surface/position |
| GSW torso | Direct organ damage | Vascular injury | 25-40% | Trajectory/velocity |
| Stab wound | Single organ | Adjacent structures | 5-15% | Weapon length/angle |
💡 Master This: Waddell's Triad in pediatric auto-pedestrian accidents - Femur fracture + thoracic injury + contralateral head injury from impact-fall-run over sequence
These pattern recognition frameworks enable systematic evaluation that reveals injury combinations requiring immediate intervention versus observation protocols.
🎯 The Pattern Recognition Matrix: Clinical Decision Frameworks
🔍 The Diagnostic Discrimination Engine: Systematic Injury Analysis
Imaging Decision Algorithms
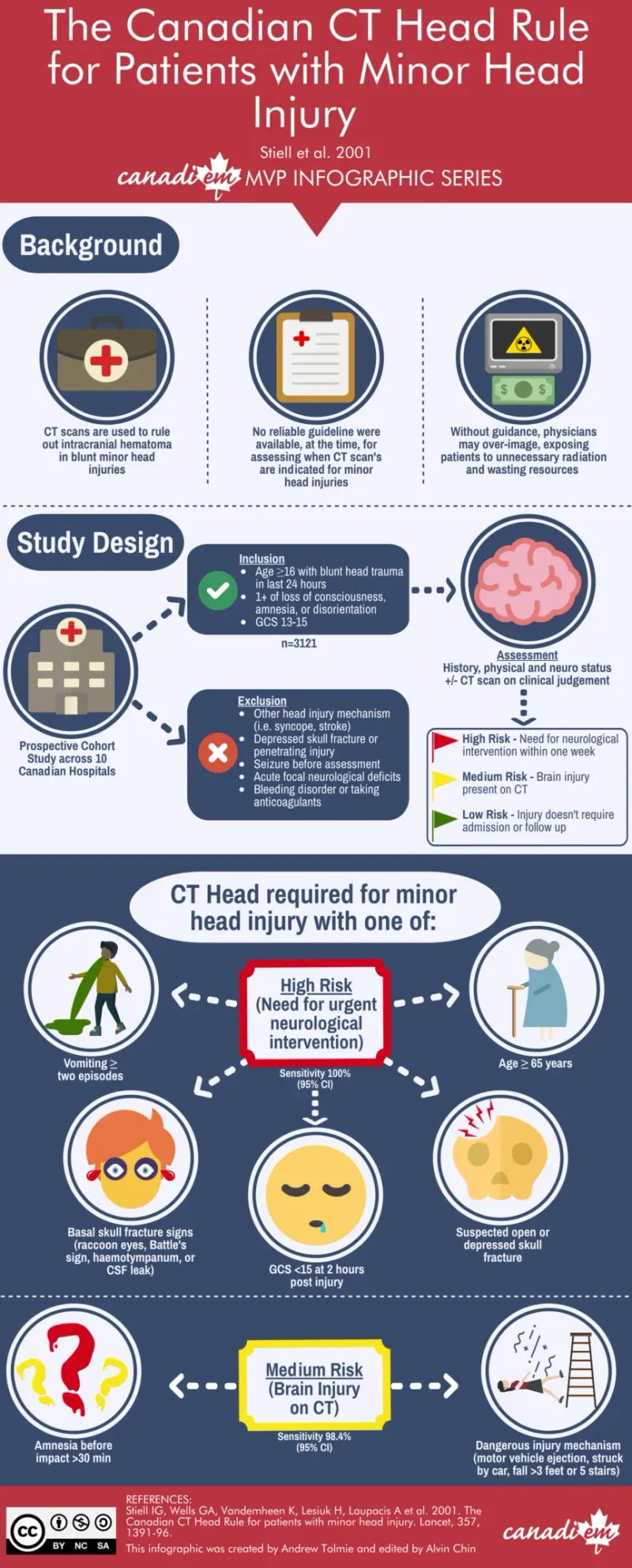
- CT Head Indications (Canadian CT Head Rule - 99.4% sensitivity)
-
High Risk (require neurosurgical intervention)
- GCS score <15 at 2 hours post-injury
- Suspected open or depressed skull fracture
- Any sign of basal skull fracture (hemotympanum, raccoon eyes)
- Vomiting ≥2 episodes
- Age ≥65 years
-
Medium Risk (clinically important brain injury)
- Amnesia before impact ≥30 minutes
- Dangerous mechanism (pedestrian struck, fall >3 feet)
-
📌 Remember: HEADS - High GCS, Elderly >65, Amnesia >30min, Dangerous mechanism, Signs of skull fracture = CT indicated
Chest Trauma Differentiation
-
Immediate Thoracotomy Indications
- Initial chest tube output >1500mL
- Continued bleeding >200mL/hr for 2-4 hours
- Massive air leak with inability to expand lung
- Cardiac tamponade with hemodynamic instability
-
Chest Tube vs Observation
- Pneumothorax >20%: Chest tube required
- Pneumothorax <20% + stable: Observation acceptable
- Hemothorax >300mL: Chest tube drainage
- Small hemothorax + stable: Serial imaging
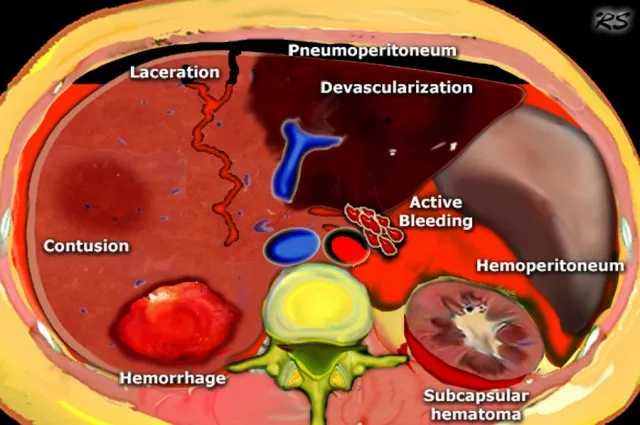
Abdominal Trauma Discrimination
-
Immediate Laparotomy Criteria
- Hemodynamic instability with positive FAST
- Peritonitis on physical examination
- Free air on imaging (hollow viscus injury)
- Penetrating trauma with peritoneal violation
-
CT vs Observation Thresholds
- Hemoperitoneum without hemodynamic compromise
- Solid organ injury grades I-III (stable patients)
- Retroperitoneal hematoma (blunt trauma)
| Injury Type | Grade I-II | Grade III | Grade IV-V | Operative Rate | Mortality |
|---|---|---|---|---|---|
| Splenic laceration | Observation 95% | Observation 80% | Surgery 60% | 15-20% | 5-10% |
| Liver laceration | Observation 90% | Observation 70% | Surgery 80% | 20-25% | 10-15% |
| Kidney injury | Observation 98% | Observation 85% | Surgery 40% | 5-10% | 2-5% |
| Pancreatic injury | Observation 60% | Surgery 70% | Surgery 95% | 40-50% | 15-25% |
| Bowel injury | Surgery 100% | Surgery 100% | Surgery 100% | 100% | 5-15% |
💡 Master This: Damage control surgery principles - Control hemorrhage → Limit contamination → Temporary closure → ICU resuscitation → Definitive repair in 24-48 hours
Spinal Trauma Clearance Protocols
-
NEXUS Criteria (99.6% sensitivity for C-spine injury)
- No posterior midline cervical tenderness
- No evidence of intoxication
- Normal level of alertness
- No focal neurological deficit
- No painful distracting injuries
-
Canadian C-Spine Rule (100% sensitivity, higher specificity)
- High-risk factors: Age ≥65, dangerous mechanism, paresthesias
- Low-risk factors: Simple rear-end MVC, sitting position, ambulatory
- Range of motion: Able to rotate neck 45° left and right
These systematic discrimination tools enable rapid, evidence-based decisions that optimize resource utilization while maintaining diagnostic accuracy for critical injuries.
🔍 The Diagnostic Discrimination Engine: Systematic Injury Analysis
⚖️ The Treatment Command Protocol: Evidence-Based Intervention Algorithms
Damage Control Resuscitation Protocol
- Massive Transfusion Protocol (MTP activation criteria)
- Assessment of Blood Consumption (ABC) score ≥2
- Systolic BP ≤90 mmHg (1 point)
- Heart rate ≥120 bpm (1 point)
- Positive FAST exam (1 point)
- Penetrating mechanism (1 point)
- Shock Index ≥1.0 (HR/SBP ratio)
- Clinical judgment: Anticipated >10 units PRBC in 24 hours
- Assessment of Blood Consumption (ABC) score ≥2
Resuscitation Endpoints
-
Goal-Directed Therapy Targets
- Hemoglobin: 7-9 g/dL (restrictive strategy)
- Platelet count: >50,000 (>100,000 if CNS injury)
- INR: <1.5 (FFP or PCC correction)
- Fibrinogen: >150 mg/dL (cryoprecipitate if low)
- pH: >7.2 (bicarbonate if severe acidosis)
- Temperature: >35°C (active rewarming protocols)
-
Permissive Hypotension (until hemorrhage control)
- Systolic BP target: 80-90 mmHg (penetrating trauma)
- Systolic BP target: 90-100 mmHg (blunt trauma)
- MAP target: >65 mmHg (if head injury present)
📌 Remember: STOP the Lethal Triad - Stop bleeding, Temperature >35°C, Optimize pH >7.2, Platelets >50K
Surgical Intervention Thresholds
-
Emergency Department Thoracotomy (EDT)
- Penetrating chest trauma: <15 minutes arrest
- Penetrating abdominal trauma: <5 minutes arrest
- Blunt trauma: Generally contraindicated (survival <2%)
- Signs of life: Required within 15 minutes of arrival
-
Damage Control Surgery Principles
- Phase I: Control hemorrhage and contamination (<90 minutes)
- Phase II: ICU resuscitation (24-48 hours)
- Phase III: Definitive repair (when physiologically stable)
| Intervention | Time Window | Success Rate | Mortality Reduction | Key Endpoints |
|---|---|---|---|---|
| MTP activation | <30 minutes | 85% hemostasis | 40% reduction | 1:1:1 ratio maintained |
| Damage control surgery | <90 minutes | 70% survival | 50% reduction | Hemorrhage control |
| Permissive hypotension | Until hemostasis | 60% less bleeding | 25% reduction | SBP 80-90 mmHg |
| Hypothermia prevention | Continuous | 90% normothermia | 30% reduction | Core temp >35°C |
| Early antibiotics | <1 hour | 95% compliance | 20% infection ↓ | Broad spectrum |
💡 Master This: Damage control mindset - "Life over limb, function over form" - Temporary measures that save life take priority over definitive repair until physiological stability achieved
Specific Injury Management
-
Tension Pneumothorax (immediate decompression)
- Needle decompression: 2nd intercostal space, midclavicular line
- 14-gauge needle or larger (standard IV catheter inadequate)
- Chest tube placement: 5th intercostal space, anterior axillary line
- Success rate: >95% with proper technique
-
Pericardial Tamponade (emergency pericardiocentesis)
- Subxiphoid approach: 45° angle toward left shoulder
- Aspiration: Even 20-30mL can restore cardiac output
- Definitive treatment: Surgical pericardial window or repair
These evidence-based treatment protocols provide systematic approaches that optimize outcomes through goal-directed interventions with measurable endpoints and defined success criteria.
⚖️ The Treatment Command Protocol: Evidence-Based Intervention Algorithms
🔗 The Multi-System Integration Matrix: Advanced Trauma Synthesis
The Inflammatory Cascade Integration
-
Systemic Inflammatory Response (SIRS) progression
- Initial hit: Tissue damage + hemorrhage triggers cytokine release
- Cytokine storm: IL-1, TNF-α, IL-6 peak at 6-12 hours
- Compensatory response: IL-10, IL-4 anti-inflammatory surge
- Immunoparalysis: >48 hours post-injury, infection susceptibility ↑
-
Multi-Organ Dysfunction Sequence
- Lung (first affected): ARDS develops in 25% of severe trauma
- Kidney: AKI in 30% of shock patients within 48 hours
- Liver: Synthetic dysfunction by 72 hours (albumin, coagulation)
- GI tract: Bacterial translocation and stress ulceration
Coagulopathy Integration Patterns
- Trauma-Induced Coagulopathy (TIC) mechanisms
- Acute coagulopathy: Present in 25% on arrival (independent of dilution)
- Protein C activation: Thrombomodulin upregulation causes anticoagulation
- Fibrinolysis: tPA release leads to clot breakdown
- Platelet dysfunction: ADP and thrombin response impaired
Neurotrauma-Systemic Interactions
-
Brain-Body Crosstalk in trauma
- Sympathetic storm: Catecholamine surge causes cardiac dysfunction
- Neurogenic pulmonary edema: α-adrenergic vasoconstriction
- Stress hyperglycemia: Cortisol and catecholamine effects
- Immunosuppression: HPA axis activation reduces T-cell function
-
Secondary Brain Injury Prevention
- Hypotension (SBP <90 mmHg): Doubles mortality in TBI
- Hypoxia (SaO2 <90%): Triples poor neurological outcome
- Hyperthermia (>38.5°C): Worsens cerebral edema
- Hyperglycemia (>180 mg/dL): Increases infarct size
| System | Primary Insult | Secondary Effects | Timeline | Prevention Strategy | Outcome Impact |
|---|---|---|---|---|---|
| Pulmonary | Contusion/aspiration | ARDS, pneumonia | 24-72 hours | Lung-protective ventilation | 30% mortality ↓ |
| Renal | Hypoperfusion/rhabdo | AKI, electrolyte disorders | 12-48 hours | Fluid optimization | 25% mortality ↓ |
| Cardiac | Contusion/tamponade | Arrhythmias, failure | 6-24 hours | Hemodynamic monitoring | 20% mortality ↓ |
| Hepatic | Hypoperfusion/injury | Synthetic dysfunction | 48-96 hours | Avoid hepatotoxins | 15% mortality ↓ |
| Neurologic | Primary injury | Edema, herniation | 1-72 hours | ICP management | 40% mortality ↓ |
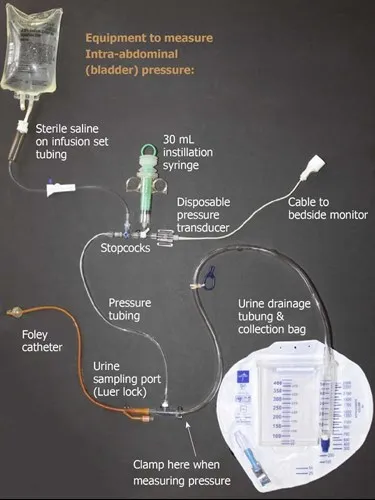
⭐ Clinical Pearl: Abdominal compartment syndrome develops in 15% of trauma patients requiring massive resuscitation - Bladder pressure >20 mmHg with organ dysfunction requires decompressive laparotomy
💡 Master This: "The second hit phenomenon" - Subsequent insults (surgery, infection, hypotension) in primed inflammatory state cause disproportionate organ dysfunction - Timing of interventions critical
Geriatric Trauma Considerations
-
Age-Related Vulnerability Factors
- Physiological reserve: ↓50% cardiac output response to stress
- Medication interactions: Anticoagulants in 40% of patients >65
- Comorbidity burden: ≥3 conditions in 75% of elderly trauma
- Frailty index: >5 deficits predicts poor outcomes regardless of injury
-
Modified Thresholds for elderly patients
- Tachycardia: May be blunted by β-blockers (30% of patients)
- Hypotension: Baseline SBP may be >140 mmHg (adjust targets)
- GCS: Baseline cognitive impairment affects assessment
- Pain response: Altered due to neuropathy and medications
Understanding these multi-system interactions enables proactive management that prevents cascade failures and optimizes outcomes through integrated care approaches that address both primary injuries and secondary complications.
🔗 The Multi-System Integration Matrix: Advanced Trauma Synthesis
🎯 The Trauma Mastery Arsenal: Rapid Response Excellence
The Essential Numbers Arsenal
📌 Remember: "Rule of 30s" - 30% blood loss = shock, 30 minutes = golden hour window, 30 mmHg pulse pressure = significant volume loss
- Critical Thresholds
- Shock Index >1.0 = significant hemorrhage
- GCS ≤8 = intubation required
- Systolic BP <90 = hypotensive shock
- Heart Rate >120 = compensatory tachycardia
- Respiratory Rate >29 = respiratory distress
- Temperature <35°C = hypothermia (lethal triad)
Rapid Assessment Framework
| Assessment | Normal | Concerning | Critical | Action Required |
|---|---|---|---|---|
| Airway | Clear speech | Stridor/hoarseness | Obstruction | Immediate intubation |
| Breathing | RR 12-20, SpO2 >95% | RR >25, SpO2 90-95% | RR >30, SpO2 <90% | Ventilatory support |
| Circulation | HR <100, SBP >90 | HR 100-120, SBP 70-90 | HR >120, SBP <70 | Massive transfusion |
| Disability | GCS 15, PERRL | GCS 9-14, sluggish | GCS ≤8, fixed pupils | Neurosurgical consult |
| Exposure | Normothermic | Mild hypothermia | Temp <35°C | Active rewarming |
💡 Master This: ATLS systematic approach prevents missed injuries in >95% of cases - Never deviate from primary survey sequence regardless of obvious injuries
Procedure Mastery Checklist
-
Needle Decompression (tension pneumothorax)
- Location: 2nd intercostal space, midclavicular line
- Needle: 14-gauge or larger (standard IV inadequate)
- Depth: 4-5 cm in average adult
- Confirmation: Rush of air and clinical improvement
-
Chest Tube Insertion
- Location: 5th intercostal space, anterior axillary line
- Size: 36-40 French for hemothorax, 28-32 French for pneumothorax
- Technique: Blunt dissection through pleura
- Suction: -20 cmH2O continuous suction
Master these rapid response protocols, and you possess the systematic frameworks that enable expert trauma care under high-pressure conditions where seconds determine outcomes and systematic approaches prevent cognitive overload that leads to missed diagnoses and delayed interventions.
🎯 The Trauma Mastery Arsenal: Rapid Response Excellence
Practice Questions: Trauma/Emergencies
Test your understanding with these related questions
A 34-year-old man is admitted to the emergency department after a motor vehicle accident in which he sustained blunt abdominal trauma. On admission, he is conscious, has a GCS score of 15, and has normal ventilation with no signs of airway obstruction. Vitals initially are blood pressure 95/65 mmHg, heart rate 87/min, respiratory rate 14/min, and oxygen saturation of 95% on room air. The physical exam is significant only for tenderness to palpation over the left flank. Noncontrast CT of the abdomen shows fractures of the 9th and 10th left ribs. Intravenous fluids are administered and the patient's blood pressure increases to 110/80 mm Hg. Three days later after admission, the patient suddenly complains of weakness and left upper quadrant (LUQ) pain. Vitals are blood pressure 80/50 mm Hg, heart rate 97/min, respiratory rate 18/min, temperature 36.2℃ (97.2℉) and oxygen saturation of 99% on room air. Prompt administration of 2L of IV fluids increases the blood pressure to 100/70 mm Hg. On physical exam, there is dullness to percussion and rebound tenderness with guarding in the LUQ. Bowel sounds are present. Raising the patient's left leg results in pain in his left shoulder. Stat hemoglobin level is 9.8 g/dL. Which of the following findings would be most likely seen if a CT scan were performed now?











