Post-transplant infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Post-transplant infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Post-transplant infections US Medical PG Question 1: A 26-year-old man comes to the physician for a follow-up examination. He was diagnosed with HIV infection 2 weeks ago. His CD4+ T-lymphocyte count is 162/mm3 (N ≥ 500). An interferon-gamma release assay is negative. Prophylactic treatment against which of the following pathogens is most appropriate at this time?
- A. Cytomegalovirus
- B. Toxoplasma gondii
- C. Mycobacterium tuberculosis
- D. Aspergillus fumigatus
- E. Pneumocystis jirovecii (Correct Answer)
Post-transplant infections Explanation: ***Pneumocystis jirovecii***
- This patient's **CD4+ T-lymphocyte count of 162/mm3** is below the threshold of 200/mm3, indicating a significant risk for **Pneumocystis pneumonia (PCP)**, an opportunistic infection in HIV.
- Prophylaxis with **trimethoprim-sulfamethoxazole (TMP-SMX)** is highly effective and recommended for HIV patients with CD4 counts less than 200/mm3.
*Cytomegalovirus*
- **CMV prophylaxis** is generally not recommended for all HIV patients, even with low CD4 counts, unless there is evidence of active disease or extremely low CD4 counts (e.g., <50/mm3) with high viral loads.
- While CMV can cause end-organ disease in advanced HIV, routine primary prophylaxis is not standard for this CD4 level.
*Toxoplasma gondii*
- **Toxoplasma prophylaxis** is indicated for HIV patients with **CD4 counts less than 100/mm3** who are also seropositive for *Toxoplasma gondii*.
- The patient's CD4 count is 162/mm3, and there's no mention of *Toxoplasma* serostatus, making it less appropriate than PCP prophylaxis.
*Mycobacterium tuberculosis*
- The patient's **interferon-gamma release assay (IGRA) is negative**, which suggests no **latent tuberculosis infection (LTBI)**, thus making primary prophylaxis unnecessary at this time.
- While HIV patients are at high risk for TB, prophylaxis is typically given for LTBI or as secondary prophylaxis for those who have completed treatment for active TB.
*Aspergillus fumigatus*
- **Aspergillus infections** are typically seen in patients with severe **neutropenia** or those receiving high-dose corticosteroids, not primarily in HIV patients based solely on CD4 count.
- Routine prophylaxis for Aspergillus is not recommended for HIV patients, even with low CD4 counts, unless there is a specific risk factor.
Post-transplant infections US Medical PG Question 2: A 55-year-old woman recently underwent kidney transplantation for end-stage renal disease. Her early postoperative period was uneventful, and her serum creatinine is lowered from 4.3 mg/dL (preoperative) to 2.5 mg/dL. She is immediately started on immunosuppressive therapy. On postoperative day 7, she presents to the emergency department (ED) because of nausea, fever, abdominal pain at the transplant site, malaise, and pedal edema. The vital signs include: pulse 106/min, blood pressure 167/96 mm Hg, respirations 26/min, and temperature 40.0°C (104.0°F). The surgical site shows no signs of infection. Her urine output is 250 mL over the past 24 hours. Laboratory studies show:
Hematocrit 33%
White blood cell (WBC) count 6700/mm3
Blood urea 44 mg/dL
Serum creatinine 3.3 mg/dL
Serum sodium 136 mEq/L
Serum potassium 5.6 mEq/L
An ultrasound of the abdomen shows collection of fluid around the transplanted kidney with moderate hydronephrosis. Which of the following initial actions is the most appropriate?
- A. Re-operate and remove the failed kidney transplant
- B. Continue with an ultrasound-guided biopsy of the transplanted kidney (Correct Answer)
- C. Start on pulse steroid treatment or OKT3
- D. Supportive treatment with IV fluids, antibiotics, and antipyretics
- E. Consider hemodialysis
Post-transplant infections Explanation: ***Continue with an ultrasound-guided biopsy of the transplanted kidney***
- The patient's symptoms (fever, malaise, abdominal pain, rising creatinine) and ultrasound findings (fluid collection, hydronephrosis) are highly suggestive of **acute renal allograft rejection** or an **obstructive uropathy**, necessitating a definitive diagnosis through biopsy.
- A biopsy will differentiate between rejection, drug toxicity, or other causes of allograft dysfunction, guiding appropriate and specific treatment.
*Re-operate and remove the failed kidney transplant*
- Removing the transplanted kidney is a drastic measure and premature at this stage, as the cause of dysfunction is not yet confirmed.
- The elevated creatinine and hydronephrosis could be reversible with proper treatment once the underlying cause is identified.
*Start on pulse steroid treatment or OKT3*
- While pulse steroids or OKT3 (muromonab-CD3) are used to treat acute rejection, administering them without a definitive diagnosis from a biopsy could be inappropriate and potentially harmful.
- The symptoms could also be due to infection or obstruction, which would not respond to these immunosuppressive therapies and could worsen with increased immunosuppression.
*Supportive treatment with IV fluids, antibiotics, and antipyretics*
- Supportive care alone is insufficient given the potential for acute allograft rejection or severe obstruction, which requires specific intervention.
- Although the patient has fever, there are no clear signs of infection, and empirical antibiotics may delay necessary diagnostic steps.
*Consider hemodialysis*
- While the patient's creatinine is elevated and potassium is high, these parameters alone do not immediately warrant hemodialysis without exploring the underlying cause of allograft dysfunction.
- Dialysis is typically considered when there are severe indications like refractory hyperkalemia, fluid overload, acidosis, or uremic symptoms that cannot be otherwise managed, and the primary goal should be to treat the cause of decreasing kidney function.
Post-transplant infections US Medical PG Question 3: An investigator is conducting a study to identify potential risk factors for post-transplant hypertension. The investigator selects post-transplant patients with hypertension and gathers detailed information regarding their age, gender, preoperative blood pressure readings, and current medications. The results of the study reveal that some of the patients had been treated with cyclosporine. This study is best described as which of the following?
- A. Cross-sectional study
- B. Retrospective cohort study
- C. Prospective cohort study
- D. Case series
- E. Case-control study (Correct Answer)
Post-transplant infections Explanation: ***Case-control study***
- A **case-control study** compares individuals with a disease (cases) to individuals without the disease (controls) to identify risk factors retrospectively.
- In this study, the investigator selects post-transplant patients **with hypertension** (the cases) and looks backward at their exposures, including cyclosporine use, to identify potential risk factors.
- The analytical goal of "identifying risk factors" and the observation that **some patients had been treated with cyclosporine** (implying comparison with those who were not) indicates a case-control design.
- Even if controls are not explicitly mentioned, the study design involves analyzing exposure patterns among cases to identify associations with risk factors.
*Case series*
- A **case series** is purely descriptive and involves collecting detailed information on a group of patients with a common condition without any comparison or analytical hypothesis testing.
- While this study does describe patients with post-transplant hypertension, the key difference is the **analytical intent** to identify risk factors, which goes beyond simple description.
- A true case series would simply report clinical characteristics without attempting to establish associations between exposures and outcomes.
*Cross-sectional study*
- A **cross-sectional study** assesses both exposure and outcome simultaneously at a single point in time to determine prevalence.
- This approach would involve surveying a population of post-transplant patients to determine the prevalence of hypertension and associated factors at that moment.
- The study described has already selected patients with the outcome (hypertension), making it retrospective rather than cross-sectional.
*Retrospective cohort study*
- A **retrospective cohort study** examines past data by first classifying patients based on **exposure status** (e.g., cyclosporine use vs. no cyclosporine), then following them forward in time to see who developed the outcome.
- The key difference is that cohort studies **start with exposure** and move to outcome, whereas this study **starts with outcome** (hypertension) and looks back at exposures.
- If the investigator had selected all transplant patients, divided them by cyclosporine exposure, and then determined hypertension rates in each group, it would be a retrospective cohort study.
*Prospective cohort study*
- A **prospective cohort study** identifies a cohort at baseline (before the outcome) and follows them forward in time to observe who develops the outcome.
- This study has already selected patients **with the outcome present**, making it retrospective rather than prospective.
- A prospective design would require identifying transplant patients at the time of transplant and following them over time to see who develops hypertension.
Post-transplant infections US Medical PG Question 4: A 56-year-old man comes to the emergency department because of progressively worsening shortness of breath and fever for 2 days. He also has a nonproductive cough. He does not have chest pain or headache. He has chronic myeloid leukemia and had a bone marrow transplant 3 months ago. His current medications include busulfan, mycophenolate mofetil, tacrolimus, and methylprednisolone. His temperature is 38.1°C (100.6°F), pulse is 103/min, respirations are 26/min, and blood pressure is 130/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 93%. Pulmonary examination shows diffuse crackles. The spleen tip is palpated 4 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.3 g/dL
Leukocyte count 4,400/mm3
Platelet count 160,000/mm3
Serum
Glucose 78 mg/dL
Creatinine 2.1 mg/dL
D-dimer 96 ng/mL (N < 250)
pp65 antigen positive
Galactomannan antigen negative
Urinalysis is normal. An x-ray of the chest shows diffuse bilateral interstitial infiltrates. An ECG shows sinus tachycardia. Which of the following is the most appropriate pharmacotherapy?
- A. Levofloxacin
- B. Ganciclovir (Correct Answer)
- C. Valganciclovir
- D. Azithromycin
- E. Acyclovir
Post-transplant infections Explanation: ***Ganciclovir***
- The patient's **positive pp65 antigen** confirms **cytomegalovirus (CMV) infection**, the most common viral infection in immunocompromised bone marrow transplant recipients.
- This patient has **severe, life-threatening CMV pneumonitis** evidenced by hypoxia (O2 sat 93%), tachypnea, and diffuse bilateral interstitial infiltrates.
- **Intravenous ganciclovir** is the **first-line treatment** for severe CMV disease due to its potent antiviral activity and reliable bioavailability in critically ill patients.
*Valganciclovir*
- **Valganciclovir** is an **oral prodrug of ganciclovir** with excellent bioavailability, but it is primarily reserved for **CMV prophylaxis** or **maintenance therapy** after initial IV treatment.
- In this patient with **acute, severe CMV pneumonitis** requiring urgent intervention (hypoxia, respiratory distress), **IV ganciclovir is strongly preferred** for faster, more reliable drug delivery and higher tissue concentrations.
*Levofloxacin*
- This **fluoroquinolone antibiotic** treats **bacterial infections**, not viral pathogens like CMV.
- The **positive pp65 antigen** specifically identifies CMV as the etiology, and negative galactomannan rules out invasive aspergillosis.
- While empiric antibacterial coverage might be considered in febrile neutropenic patients, the clear viral diagnosis directs therapy toward antivirals.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic effective against atypical bacteria (Mycoplasma, Chlamydophila) and some other bacterial pathogens.
- It has **no activity against CMV** and would not address the confirmed viral etiology.
*Acyclovir*
- **Acyclovir** is effective against **herpes simplex virus (HSV)** and **varicella-zoster virus (VZV)**, but has **poor activity against CMV** due to inadequate phosphorylation by CMV enzymes.
- The positive pp65 antigen specifically indicates CMV, for which ganciclovir (not acyclovir) is required.
Post-transplant infections US Medical PG Question 5: A 33-year-old HIV-positive male is seen in clinic for follow-up care. When asked if he has been adhering to his HIV medications, the patient exclaims that he has been depressed, thus causing him to not take his medication for six months. His CD4+ count is now 33 cells/mm3. What medication(s) should he take in addition to his anti-retroviral therapy?
- A. Azithromycin and fluconazole
- B. Azithromycin, dapsone, and fluconazole
- C. Dapsone
- D. Fluconazole
- E. Azithromycin and trimethoprim-sulfamethoxazole (Correct Answer)
Post-transplant infections Explanation: ***Azithromycin and trimethoprim-sulfamethoxazole***
- With a **CD4+ count of 33 cells/mm3**, this patient is at high risk for **Pneumocystis jirovecii pneumonia (PJP)** and **Toxoplasma gondii encephalitis**, for which **trimethoprim-sulfamethoxazole (TMP-SMX)** is the prophylaxis of choice.
- He is also at very high risk for **Mycobacterium avium complex (MAC) infection**, for which **azithromycin** is the recommended preventative treatment when the CD4 count is below 50 cells/mm3.
*Azithromycin and fluconazole*
- While **azithromycin** is indicated for MAC prophylaxis, **fluconazole** is typically used for **cryptococcal meningitis** or **candidiasis**, which are not the primary, immediate prophylactic concerns at this specific CD4 count unless there's evidence of these infections.
- The most critical opportunistic infections to prevent at a CD4 count of 33 cells/mm3 are PJP, Toxoplasmosis, and MAC.
*Azithromycin, dapsone, and fluconazole*
- **Dapsone** can be used as an alternative for **PJP prophylaxis** if TMP-SMX is contraindicated, but it is not the first-line choice and does not cover toxoplasmosis as effectively as TMP-SMX alone.
- **Fluconazole** again is not a primary prophylactic agent at this CD4 count in the absence of specific indications.
*Dapsone*
- **Dapsone** is an alternative for **PJP prophylaxis** and can also prevent **Toxoplasma gondii encephalitis** when combined with pyrimethamine, but it is not the first-line recommendation.
- It does not provide coverage against **MAC infection**, which is a significant risk at this CD4 count.
*Fluconazole*
- **Fluconazole** is primarily used for **fungal infections** like **candidiasis** or **cryptococcosis**.
- It does not prevent **PJP, Toxoplasmosis, or MAC**, which are the most critical prophylactic concerns for a patient with a CD4 count of 33 cells/mm3.
Post-transplant infections US Medical PG Question 6: A 26-year-old man is undergoing a bone marrow transplantation for treatment of a non-Hodgkin lymphoma that has been refractory to several rounds of chemotherapy and radiation over the past 2 years. He has been undergoing a regimen of cyclophosphamide and total body irradiation for the past several weeks in anticipation of his future transplant. This morning, he reports developing a productive cough and is concerned because he noted some blood in his sputum this morning. The patient also reports pain with inspiration. His temperature is 101°F (38.3°C), blood pressure is 115/74 mmHg, pulse is 120/min, respirations are 19/min, and oxygen saturation is 98% on room air. A chest radiograph and CT are obtained and shown in Figures A and B respectively. Which of the following is the most likely diagnosis?
- A. Streptococcus pneumoniae
- B. Aspergillus fumigatus (Correct Answer)
- C. Pneumocystis jiroveci pneumonia
- D. Staphylococcus aureus
- E. Mycoplasma pneumonia
Post-transplant infections Explanation: ***Aspergillus fumigatus***
- The patient's immunocompromised state due to **chemotherapy** and **total body irradiation** for lymphoma, combined with the presence of a **productive cough with hemoptysis**, pleuritic pain, and fever, is highly suggestive of an invasive fungal infection.
- **Chest imaging** demonstrating nodules with surrounding ground-glass opacity (the **"halo sign"** on CT) is characteristic of **invasive aspergillosis** in immunocompromised patients, where the ground-glass attenuation represents hemorrhage around a nodular lesion.
*Streptococcus pneumoniae*
- While *S. pneumoniae* can cause pneumonia in immunocompromised patients, it typically presents with **lobar consolidation** on imaging, not the nodular lesions with a halo sign seen here.
- **Hemoptysis**, although possible, is less common as a prominent symptom than in invasive fungal infections in this context.
*Pneumocystis jiroveci pneumonia*
- *Pneumocystis* pneumonia (PCP) typically presents with **diffuse interstitial infiltrates** on chest imaging, often described as ground-glass opacities, but usually lacks the focal nodular lesions or hemoptysis seen here.
- PCP is more common in patients with **HIV/AIDS** or those undergoing specific immunosuppressive regimens (e.g., high-dose corticosteroids), and while possible, the imaging findings do not directly support it.
*Staphylococcus aureus*
- *S. aureus* pneumonia can cause **abscess formation** and **cavitary lesions**, but the imaging described (nodules with halo sign) is not typical.
- While it can cause severe pneumonia in immunocompromised hosts, **hemoptysis** and the specific imaging findings align less with *S. aureus* and more with invasive mold infections.
*Mycoplasma pneumonia*
- *Mycoplasma pneumoniae* causes **"walking pneumonia"** and typically presents with milder symptoms and **interstitial or patchy infiltrates** on chest imaging.
- Severe symptoms like **hemoptysis** and the imaging findings of nodular lesions with a halo sign are not characteristic of *Mycoplasma* infection.
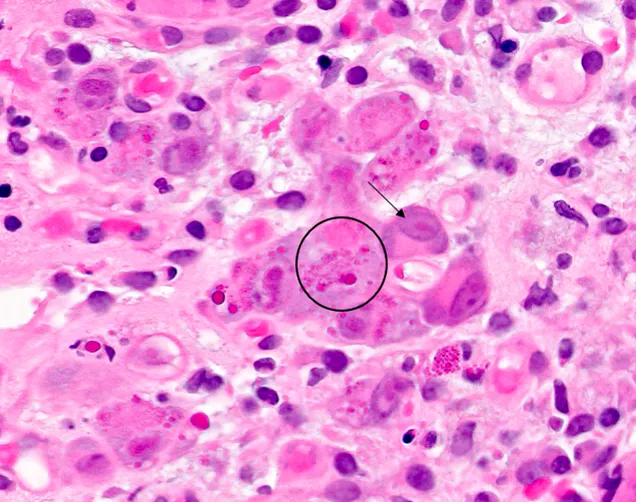
Post-transplant infections US Medical PG Question 7: A 55-year-old man comes to the physician because of fever, fatigue, dry cough, headache, and myalgia over the past week. Two days ago, he developed several painful oral lesions and difficulty swallowing. He underwent kidney transplantation 3 years ago. His temperature is 38.2°C (100.7°F). Physical examination shows bilateral rales, hepatosplenomegaly, and multiple 1–2 cm ulcerative lesions with raised borders in the oral mucosa. A photomicrograph of a liver biopsy specimen is shown. Which of the following is the most likely causal pathogen?
- A. Aspergillus fumigatus
- B. Blastomyces dermatitidis
- C. Coccidioides immitis
- D. Paracoccidioides brasiliensis
- E. Histoplasma capsulatum (Correct Answer)
Post-transplant infections Explanation: ***Histoplasma capsulatum***
- The patient's presentation with **fever, fatigue, dry cough, headache, myalgia, respiratory symptoms (bilateral rales), hepatosplenomegaly**, and **painful oral ulcerative lesions** in an **immunocompromised individual (kidney transplant recipient)** is highly suggestive of **disseminated histoplasmosis**.
- The photomicrograph shows numerous **small, intracellular yeast forms within macrophages**, which is the pathognomonic finding for *Histoplasma capsulatum*.
- *Histoplasma* is endemic to the Ohio and Mississippi River valleys and commonly causes disseminated disease in immunocompromised patients.
*Aspergillus fumigatus*
- *Aspergillus* typically causes invasive pulmonary aspergillosis in immunocompromised patients, presenting with **fever and cough**, but generally does not cause **oral ulcerative lesions** or **hepatosplenomegaly** in this disseminated pattern.
- Microscopically, *Aspergillus* appears as **septate hyphae with acute-angle branching (45°)**, which is inconsistent with the intracellular yeasts in the image provided.
*Blastomyces dermatitidis*
- *Blastomyces* can cause pulmonary disease and disseminate to the **skin and bones**, but **oral lesions** and **hepatosplenomegaly** are less common presenting features.
- The yeast forms of *Blastomyces* are characteristically **large (8-15 μm), broad-based budding yeasts**, which are much larger than the small organisms seen in the photomicrograph.
*Coccidioides immitis*
- *Coccidioidomycosis* is endemic to the southwestern U.S. and can cause pulmonary symptoms, but disseminated disease typically involves the **skin, bones, joints, and meninges**, with **oral lesions and hepatosplenomegaly** being less frequent manifestations.
- Microscopically, *Coccidioides* is characterized by **large spherules (20-80 μm) containing endospores**, which are not seen in the provided image showing small intracellular organisms.
*Paracoccidioides brasiliensis*
- This fungus is endemic to Central and South America and can cause oral lesions that are typically **mulberry-like** or **verrucous** in appearance, with disseminated disease often affecting the lungs, lymph nodes, and mucosal surfaces.
- Microscopic examination reveals **multiple budding yeasts** with a characteristic **"ship's wheel" or "pilot's wheel" appearance**, which differs significantly from the small intracellular yeasts within macrophages shown in the image.
Post-transplant infections US Medical PG Question 8: A 14-year-old boy has undergone kidney transplantation due to stage V chronic kidney disease. A pre-transplantation serologic assessment showed that he is negative for past or present HIV infection, viral hepatitis, EBV, and CMV infection. He has a known allergy for macrolides. The patient has no complaints 1 day after transplantation. His vital signs include: blood pressure 120/70 mm Hg, heart rate 89/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, the patient appears to be pale, his lungs are clear on auscultation, heart sounds are normal, and his abdomen is non-tender on palpation. His creatinine is 0.65 mg/dL (57.5 µmol/L), GFR is 71.3 mL/min/1.73 m2, and urine output is 0.9 mL/kg/h. Which of the following drugs should be used in the immunosuppressive regimen in this patient?
- A. Belatacept
- B. Sirolimus
- C. Omalizumab
- D. Daclizumab
- E. Basiliximab (Correct Answer)
Post-transplant infections Explanation: **Basiliximab**
- **Basiliximab** is a **monoclonal antibody** that targets the **IL-2 receptor (CD25)** on activated T cells, preventing their proliferation and inducing immunosuppression.
- It is commonly used as **induction therapy** in kidney transplant recipients due to its good safety profile, especially in pediatric patients, without the nephrotoxicity associated with calcineurin inhibitors, minimizing acute rejection risks immediately post-transplant.
*Belatacept*
- **Belatacept** works by co-stimulation blockade, binding to **CD80 and CD86** on antigen-presenting cells to prevent T-cell activation.
- It is typically reserved for patients who cannot tolerate calcineurin inhibitors due to **nephrotoxicity** or require a steroid-sparing regimen, which is not indicated as an immediate need in this patient.
*Sirolimus*
- **Sirolimus** is an **mTOR inhibitor** that works by blocking T-cell proliferation and B-cell differentiation.
- It is associated with several side effects, including **delayed wound healing**, **thrombocytopenia**, and **hyperlipidemia**, which are undesirable in the immediate post-transplant period, especially in a growing adolescent.
*Omalizumab*
- **Omalizumab** is an **anti-IgE monoclonal antibody** primarily used for allergic asthma and chronic spontaneous urticaria.
- It has no role in **immunosuppression for organ transplantation** as its mechanism of action is unrelated to preventing graft rejection.
*Daclizumab*
- **Daclizumab** is another **monoclonal antibody** that also targets the **IL-2 receptor (CD25)**, similar to basiliximab.
- However, daclizumab has been **withdrawn from the market** due to serious adverse effects including severe liver injury and autoimmune encephalitis, making it unavailable for clinical use in transplantation.
Post-transplant infections US Medical PG Question 9: A 66-year-old man is transferred from another hospital after 3 days of progressively severe headache, vomiting, low-grade fever, and confusion. According to his partner, the patient has been dealing with some memory loss and complaining about headaches for the past 2 weeks. He has a history of interstitial pulmonary disease that required lung transplantation 2 years ago. Upon admission, he is found with a blood pressure of 160/100 mm Hg, a pulse of 58/min, a respiratory rate of 15/min, and a body temperature of 36°C (97°F). During the examination, he is found with oral thrush and symmetric and reactive pupils; there are no focal neurological signs or papilledema. A lumbar puncture is performed. Which of the following features would be expected to be found in this case?
- A. Aspect: clear, opening pressure: normal, cell count: < 5 cells/µL, protein: normal, glucose: normal
- B. Aspect: clear, opening pressure: normal, cell count: ↑ lymphocytes, protein: normal, glucose: normal
- C. Aspect: cloudy, opening pressure: ↑, cell count: ↑ neutrophils, protein: ↑, glucose: ↓
- D. Aspect: xanthochromic, opening pressure: normal, cell count: ↑ red blood cells, protein: normal, glucose: normal
- E. Aspect: clear, opening pressure: ↑, cell count: ↑ lymphocytes, protein: ↑, glucose: ↓ (Correct Answer)
Post-transplant infections Explanation: ***Aspect: clear, opening pressure: ↑, cell count: ↑ lymphocytes, protein: ↑, glucose: ↓***
- This patient presents with symptoms highly suggestive of **cryptococcal meningitis**, a common opportunistic infection in immunocompromised individuals like transplant recipients.
- **Cryptococcal meningitis** characteristically presents with **clear CSF** (not cloudy, which differentiates it from bacterial meningitis), **markedly elevated opening pressure** (often >25 cm H₂O), **lymphocytic pleocytosis**, **elevated protein**, and **decreased glucose** due to fungal metabolism.
- The presence of **oral thrush** strongly suggests fungal infection in this immunocompromised patient.
*Aspect: clear, opening pressure: normal, cell count: < 5 cells/µL, protein: normal, glucose: normal*
- This describes **normal cerebrospinal fluid (CSF)** parameters, which would not be expected in a patient presenting with signs and symptoms of meningitis, such as headache, vomiting, fever, and confusion.
- The patient's history of lung transplantation and oral thrush suggests an immunocompromised state and an opportunistic infection, ruling out normal CSF.
*Aspect: clear, opening pressure: normal, cell count: ↑ lymphocytes, protein: normal, glucose: normal*
- While **increased lymphocytes** can be seen in aseptic or viral meningitis, the overall picture of normal opening pressure, protein, and glucose does not fit this immunocompromised patient with subacute meningitis.
- The presence of **oral thrush** and **2 weeks of symptoms** indicate a more severe opportunistic infection like cryptococcal meningitis, which would show elevated opening pressure and abnormal protein and glucose levels.
*Aspect: cloudy, opening pressure: ↑, cell count: ↑ neutrophils, protein: ↑, glucose: ↓*
- This CSF profile is characteristic of **bacterial meningitis**, which is primarily marked by **cloudy CSF** due to significant **neutrophilic pleocytosis**.
- While the patient is immunocompromised, the history of **subacute symptoms** (2 weeks of headache/memory loss) and gradual deterioration is more typical of a fungal infection like **cryptococcal meningitis** rather than acute bacterial meningitis, which presents more acutely.
*Aspect: xanthochromic, opening pressure: normal, cell count: ↑ red blood cells, protein: normal, glucose: normal*
- **Xanthochromic CSF** with **elevated red blood cells** indicates subarachnoid hemorrhage.
- While headache is present, the patient's symptoms of fever, progressive confusion, oral thrush, and immunocompromised status point away from a primary hemorrhagic event and towards an infectious etiology.
Post-transplant infections US Medical PG Question 10: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
Post-transplant infections Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
More Post-transplant infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.