Organ preservation techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Organ preservation techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Organ preservation techniques US Medical PG Question 1: A 78-year-old man dies suddenly from complications of acute kidney failure. An autopsy is performed and microscopic evaluation of the kidneys shows pale, swollen cells in the proximal convoluted tubules. Microscopic evaluation of the liver shows similar findings. Which of the following is the most likely underlying mechanism of these findings?
- A. Double-stranded DNA breakage
- B. Impaired Na+/K+-ATPase pump activity (Correct Answer)
- C. Free radical formation
- D. Cytochrome C release
- E. Cytoplasmic triglyceride accumulation
Organ preservation techniques Explanation: ***Impaired Na+/K+-ATPase pump activity***
- **Acute kidney failure** leads to **hypoxia** and ATP depletion, which impairs the function of the **Na+/K+-ATPase pump** on the cell membrane.
- Failure of this pump results in **intracellular accumulation of sodium** and water, causing **cellular swelling** and pallor as seen in the kidneys and liver.
*Double-stranded DNA breakage*
- This is primarily associated with **apoptosis** or **radiation injury**, which would lead to nuclear fragmentation and cellular death rather than simple cellular swelling.
- While cell death can occur in acute kidney failure, the initial changes described (pale, swollen cells) are characteristic of **reversible cell injury** before extensive DNA damage.
*Free radical formation*
- **Free radical formation** (oxidative stress) can cause cellular injury, but it primarily leads to **lipid peroxidation of membranes** and damage to proteins and DNA, not directly to the widespread intracellular water accumulation described.
- While part of the injury cascade, it's not the most direct mechanism for the initial gross and microscopic findings of swelling.
*Cytochrome C release*
- **Cytochrome C release** from mitochondria is a critical step in the **intrinsic pathway of apoptosis**, leading to programmed cell death.
- The findings described (pale, swollen cells) are more indicative of **reversible cellular injury** or early necrosis, prior to the widespread activation of apoptosis.
*Cytoplasmic triglyceride accumulation*
- **Cytoplasmic triglyceride accumulation** (steatosis or fatty change) is often seen in conditions like **alcoholic liver disease** or **metabolic syndrome**.
- While it can be a sign of cellular injury, it does not directly explain the generalized "pale, swollen cells" observed in both the kidneys and liver following acute kidney failure, which points to water influx.
Organ preservation techniques US Medical PG Question 2: A 22-year-old man is brought to the emergency department by ambulance 1 hour after a motor vehicle accident. He did not require any circulatory resuscitation at the scene, but he was intubated because he was unresponsive. He has no history of serious illnesses. He is on mechanical ventilation with no sedation. His blood pressure is 121/62 mm Hg, the pulse is 68/min, and the temperature is 36.5°C (97.7°F). His Glasgow coma scale (GCS) is 3. Early laboratory studies show no abnormalities. A search of the state donor registry shows that he has registered as an organ donor. Which of the following is the most appropriate next step in evaluation?
- A. Evaluation of brainstem reflexes (Correct Answer)
- B. Brain MRI
- C. Electroencephalography
- D. Cerebral angiography
- E. Apnea test
Organ preservation techniques Explanation: ***Evaluation of brainstem reflexes***
- In a patient with a **Glasgow Coma Scale (GCS) of 3** and no response to noxious stimuli/sedation, assessment of **brainstem reflexes** is a critical step in determining brain death.
- This evaluation includes checking for pupillary light reflex, corneal reflex, vestibulo-ocular reflex (doll's eyes), oculocephalic reflex, and gag/cough reflexes to ascertain the complete absence of brainstem function.
*Brain MRI*
- While a brain MRI can provide detailed anatomical information regarding brain injury, it is **not the primary diagnostic test** for determining brain death.
- Brain death is a **clinical diagnosis** based on the irreversible loss of brain and brainstem function, which can be confirmed rapidly by clinical examination.
*Electroencephalography*
- **EEG** measures electrical activity in the brain and can show electrocerebral silence, which is consistent with brain death.
- However, EEG is **not always required** for the diagnosis of brain death and is often used as a confirmatory test in specific situations, such as when clinical examination is inconclusive or legal requirements necessitate it.
*Cerebral angiography*
- **Cerebral angiography** can demonstrate the absence of cerebral blood flow, which is a criterion for brain death.
- This is an **invasive procedure** and is generally reserved for situations where clinical examination tests are difficult to perform or interpret (e.g., severe facial trauma, drug intoxication), and is not the initial step.
*Apnea test*
- The **apnea test** is a critical component of the brain death evaluation, confirming the absence of spontaneous breathing response to hypercapnia.
- It is performed **after the absence of brainstem reflexes** has been established and all confounding factors (e.g., hypothermia, hypotension, sedatives) have been ruled out.
Organ preservation techniques US Medical PG Question 3: A 45-year-old woman comes to the physician because of a 3-month history of worsening fatigue, loss of appetite, itching of the skin, and progressive leg swelling. Although she has been drinking 2–3 L of water daily, she has been passing only small amounts of urine. She has type 1 diabetes mellitus, chronic kidney disease, hypertension, and diabetic polyneuropathy. Her current medications include insulin, torasemide, lisinopril, and synthetic erythropoietin. Her temperature is 36.7°C (98°F), pulse is 87/min, and blood pressure is 138/89 mm Hg. She appears pale. There is 2+ pitting edema in the lower extremities. Sensation to pinprick and light touch is decreased over the feet and legs bilaterally. Laboratory studies show:
Hemoglobin 11.4 g/dL
Leukocyte count 6000/mm3
Platelet count 280,000/mm3
Serum
Na+ 137 mEq/L
K+ 5.3 mEq/L
Cl− 100 mEq/L
HCO3− 20 mEq/L
Urea nitrogen 85 mg/dL
Creatinine 8 mg/dL
pH 7.25
Which of the following long-term treatments would best improve quality of life and maximize survival in this patient?
- A. Peritoneal dialysis
- B. Living donor kidney transplant (Correct Answer)
- C. Cadaveric kidney transplant
- D. Hemofiltration
- E. Fluid restriction
Organ preservation techniques Explanation: ***Living donor kidney transplant***
- A **living donor kidney transplant** offers the best outcomes for **quality of life and survival** in eligible patients with end-stage renal disease (ESRD), particularly when compared to dialysis, due to better graft survival rates and reduced complications.
- The patient's symptoms (fatigue, itching, leg swelling, oliguria, high urea nitrogen, creatinine, hyperkalemia, metabolic acidosis) are consistent with **ESRD**, and while she has several comorbidities, she is not explicitly stated to have contraindications for transplantation.
*Peritoneal dialysis*
- While an effective treatment for ESRD, **dialysis generally provides lower quality of life** and survival benefits compared to successful kidney transplantation.
- She already has significant fluid overload symptoms and **oliguria**, making adequate fluid removal through peritoneal dialysis potentially challenging without strict management and impacting her overall well-being.
*Cadaveric kidney transplant*
- A **cadaveric kidney transplant** is a viable option and offers better outcomes than dialysis, but it generally has **poorer graft survival** and a longer wait time compared to a living donor transplant due to delayed graft function and cold ischemia time.
- Given the option, a **living donor transplant is superior** in terms of long-term outcomes and reduces the time spent on dialysis.
*Hemofiltration*
- **Hemofiltration is a form of renal replacement therapy**, similar to hemodialysis, often used in acute settings or for critically ill patients with severe fluid overload or electrolyte imbalances.
- While it can manage her symptoms, it is not a long-term treatment that **improves quality of life or maximizes survival** better than transplantation for ESRD.
*Fluid restriction*
- **Fluid restriction** is a supportive measure to manage fluid overload in patients with ESRD; however, it addresses symptoms rather than the underlying progressive renal failure.
- While necessary as part of supportive care, it does not offer a definitive long-term solution or improve survival for ESRD, which requires **renal replacement therapy or transplantation**.
Organ preservation techniques US Medical PG Question 4: A 65-year-old man with decompensated cirrhosis secondary to hepatitis C is brought to the emergency department with 2 episodes of massive hematemesis that started 2 hours ago. He is a liver transplant candidate. The blood pressure is 110/85 mm Hg in the supine position and 90/70 mm Hg after sitting for 3 minutes. The pulse is 110/min, the respirations are 22/min, and the temperature is 36.1°C (97.0°F). The physical examination shows spider angiomata, palmar erythema, and symmetric abdominal distension with positive shifting dullness. The lung and heart examination shows no abnormalities. Two large-bore intravenous lines are obtained. Saline (0.9%) is initiated. Laboratory tests are pending. The most important next step is to administer which of the following intravenous therapies?
- A. Fresh frozen plasma
- B. Octreotide (Correct Answer)
- C. Packed red blood cells (RBCs)
- D. Propranolol
- E. Pantoprazole
Organ preservation techniques Explanation: ***Octreotide***
- This patient's presentation with **massive hematemesis**, **decompensated cirrhosis**, and signs of portal hypertension strongly suggests **esophageal variceal bleeding**.
- **Octreotide**, a somatostatin analog, is critical in managing variceal bleeding by causing **splanchnic vasoconstriction**, which reduces portal blood flow and pressure, thereby decreasing active bleeding.
*Fresh frozen plasma*
- While patients with **cirrhosis often have coagulopathy**, administering fresh frozen plasma (FFP) without documented severe coagulopathy or active bleeding requiring immediate reversal (e.g., before an invasive procedure) is not the highest priority.
- **FFP transfusions** can paradoxically increase portal pressure and volume, potentially worsening variceal bleeding.
*Packed red blood cells (RBCs)*
- Though the patient is likely anemic due to massive hematemesis, **transfusion of RBCs** should be guided by hemoglobin levels and clinical signs of hemodynamic instability, with a goal to achieve **hemodynamic stability** rather than over-transfusing.
- While important, **stopping the bleeding** with octreotide takes precedence before optimal RBC transfusion thresholds are determined.
*Propranolol*
- **Propranolol** is a non-selective beta-blocker used for **primary and secondary prophylaxis** of variceal bleeding.
- It is **contraindicated in acute bleeding** as it can worsen hypotension and interfere with the body's compensatory mechanisms during hypovolemic shock.
*Pantoprazole*
- **Pantoprazole**, a **proton pump inhibitor (PPI)**, is used to suppress stomach acid and is beneficial in managing **peptic ulcer bleeding**.
- However, it has no direct role in controlling **variceal bleeding**, which originates from esophageal varices rather than acid-related gastric or duodenal mucosa.
Organ preservation techniques US Medical PG Question 5: A 52-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He was an unrestrained passenger who was ejected from the vehicle. On presentation, he is found to be actively bleeding from numerous wounds. His blood pressure is 76/42 mmHg and pulse is 152/min. Attempts at resuscitation fail, and he dies 25 minutes later. Autopsy shows blood in the peritoneal cavity, and histology of the kidney reveals swelling of the proximal convoluted tubule epithelial cells. Which of the following is most likely the mechanism underlying the renal cell findings?
- A. Decreased activity of caspase 7
- B. Increased activity of caspase 9
- C. Increased function of the Na+/K+-ATPase
- D. Increased activity of caspase 8
- E. Decreased function of the Na+/K+-ATPase (Correct Answer)
Organ preservation techniques Explanation: ***Decreased function of the Na+/K+-ATPase***
- The patient experienced **hypovolemic shock** due to severe blood loss, leading to a significant drop in blood pressure and organ perfusion. This results in **ischemia** of the renal cells.
- **Ischemic injury** impairs ATP production, which is essential for the function of the **Na+/K+-ATPase pump**. Failure of this pump leads to intracellular accumulation of sodium and water, causing **cellular swelling**, particularly noticeable in the proximal convoluted tubules.
*Decreased activity of caspase 7*
- **Caspases**, including caspase 7, are involved in **apoptosis** (programmed cell death), which involves cell shrinkage and fragmentation, not the swelling observed here.
- Decreased caspase activity would generally *reduce* apoptosis, which is not the primary mechanism of acute cell injury in shock.
*Increased activity of caspase 9*
- Increased activity of **caspase 9** is indicative of the **intrinsic apoptotic pathway**, typically initiated by mitochondrial damage.
- While prolonged ischemia can eventually lead to apoptotic changes, the acute finding of **cellular swelling** points more directly to immediate membrane pump dysfunction due to ATP depletion.
*Increased function of the Na+/K+-ATPase*
- **Increased function** of the Na+/K+-ATPase would actively pump sodium out of the cell and potassium in, *preventing* intracellular swelling.
- This option contradicts the observed finding of proximal convoluted tubule epithelial cell swelling, which is characteristic of acute cellular injury due to pump failure.
*Increased activity of caspase 8*
- **Caspase 8** is a key initiator caspase in the **extrinsic apoptotic pathway**, often triggered by death receptor signaling.
- Similar to caspase 9, increased caspase 8 activity would lead to apoptosis, characterized by cell shrinkage, not the **cellular swelling** seen in acute ischemic injury.
Organ preservation techniques US Medical PG Question 6: A 45-year-old female is undergoing renal transplantation for management of chronic renal failure secondary to glomerulonephritis. The transplant surgeon placed the donor kidney in the recipient and anastomosed the donor renal artery to the recipient's external iliac artery as well as the donor ureter to the recipient's bladder. After removing the clamps on the external iliac artery, the recipient's blood is allowed to perfuse the transplanted kidney. Within 3 minutes, the surgeon notes that the kidney does not appear to be sufficiently perfused. Upon further investigation, an inflammatory reaction is noted that led to clotting off of the donor renal artery, preventing blood flow to the transplanted organ. Which of the following best describes the pathophysiology of this complication?
- A. Type III hypersensitivity reaction
- B. Type IV hypersensitivity reaction
- C. Graft-versus-host disease
- D. Type I hypersensitivity reaction
- E. Hyperacute rejection (Correct Answer)
Organ preservation techniques Explanation: ***Hyperacute rejection***
- This scenario describes **hyperacute rejection**, a **Type II hypersensitivity reaction** that occurs minutes to hours after transplantation due to pre-existing host antibodies (e.g., ABO or HLA antibodies) recognizing donor antigens on endothelial cells.
- The binding of these antibodies activates the complement system, leading to rapid **antibody-mediated cytotoxicity**, **thrombosis** of the graft vasculature, and ischemic necrosis.
- This represents the pathophysiologic mechanism causing the immediate graft failure observed.
*Type III hypersensitivity reaction*
- This reaction involves the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, leading to inflammation.
- It typically manifests hours to days after exposure and is not characterized by immediate graft thrombosis.
*Type IV hypersensitivity reaction*
- This is a **delayed-type hypersensitivity** mediated by T lymphocytes and macrophages, rather than antibodies.
- It usually occurs days to weeks after transplantation (e.g., in acute cellular rejection) and does not cause rapid vascular occlusion.
*Graft-versus-host disease*
- **Graft-versus-host disease (GVHD)** occurs when immunocompetent T cells from the donor (graft) recognize recipient (host) tissues as foreign and attack them.
- This complication is most common in **hematopoietic stem cell transplantation** and is unlikely to manifest minutes after solid organ transplantation.
*Type I hypersensitivity reaction*
- This is an immediate, **IgE-mediated allergic reaction** involving mast cell degranulation and release of inflammatory mediators.
- While rapid, it typically involves systemic allergic symptoms (e.g., anaphylaxis) or localized allergic responses, not specifically graft thrombosis in this context.
Organ preservation techniques US Medical PG Question 7: Two hours after undergoing a left femoral artery embolectomy, an obese 63-year-old woman has severe pain, numbness, and tingling of the left leg. The surgery was without complication and peripheral pulses were weakly palpable postprocedure. She has type 2 diabetes mellitus, peripheral artery disease, hypertension, and hypercholesterolemia. Prior to admission, her medications included insulin, enalapril, carvedilol, aspirin, and rosuvastatin. She appears uncomfortable. Her temperature is 37.1°C (99.3°F), pulse is 98/min, and blood pressure is 132/90 mm Hg. Examination shows a left groin surgical incision. The left lower extremity is swollen, stiff, and tender on palpation. Dorsiflexion of her left foot causes severe pain in her calf. Femoral pulses are palpated bilaterally. Pedal pulses are weaker on the left side as compared to the right side. Laboratory studies show:
Hemoglobin 12.1
Leukocyte count 11,300/mm3
Platelet count 189,000/mm3
Serum
Glucose 222 mg/dL
Creatinine 1.1 mg/dL
Urinalysis is within normal limits. Which of the following is the most likely cause of these findings?
- A. Reperfusion injury (Correct Answer)
- B. Cellulitis
- C. Cholesterol embolism
- D. Deep vein thrombosis
- E. Rhabdomyolysis
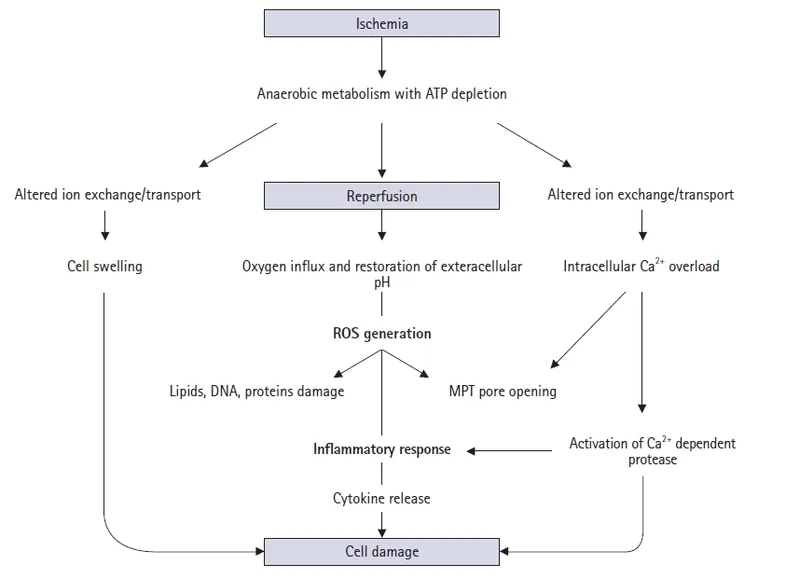
Organ preservation techniques Explanation: ***Reperfusion injury***
- The patient's symptoms of **severe pain, numbness, and tingling** in the left leg following an embolectomy, along with **swelling, stiffness, and tenderness** of the extremity, and pain on passive dorsiflexion (**pain with passive stretch**), are classic signs of **acute compartment syndrome**.
- In this context, compartment syndrome is caused by **reperfusion injury** following prolonged limb ischemia. When blood flow is restored after prolonged ischemia, the reperfusion causes **oxidative stress, inflammatory mediator release, and increased capillary permeability**, leading to **tissue edema and elevated intracompartmental pressure** that compresses nerves and vessels.
- The **2-hour timeline** post-embolectomy and the clinical triad of pain out of proportion, pain with passive stretch, and paresthesias make reperfusion injury leading to compartment syndrome the most likely diagnosis.
*Cellulitis*
- While cellulitis causes **pain, swelling, and redness**, it typically has a more **gradual onset** and is associated with warmth, erythema, and signs of infection.
- The **acute onset** (2 hours post-surgery), **severe neurologic symptoms** (numbness, tingling), and **pain with passive stretch** are not characteristic of cellulitis.
- The absence of fever, significant leukocytosis, or spreading erythema makes cellulitis unlikely.
*Cholesterol embolism*
- **Cholesterol emboli** can occur after vascular procedures and typically present with **livedo reticularis**, **"blue toe" syndrome**, **renal impairment**, or **eosinophilia**.
- While possible after arterial manipulation, the acute presentation with signs of **elevated compartment pressure** (pain with passive stretch, swelling, paresthesias) points to a pressure-related compartment issue rather than distal microembolization.
*Deep vein thrombosis*
- **DVT** causes **unilateral leg swelling, pain, and tenderness** but typically presents with a more **gradual onset** over hours to days.
- DVT would not explain the **acute severe pain with passive stretch**, **rapid neurologic symptoms** (paresthesias), or the **compartment syndrome findings** seen immediately (2 hours) post-procedure.
- The clinical picture of acute compartment syndrome better fits ischemia-reperfusion injury.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves muscle breakdown due to prolonged ischemia or trauma and is characterized by **elevated creatinine kinase (CK)**, **myoglobinuria**, and potentially **acute kidney injury**.
- While rhabdomyolysis can occur **secondary to** both the initial ischemia and subsequent compartment syndrome, it is a **consequence or complication** rather than the **primary cause** of the acute compartment syndrome findings.
- The immediate clinical presentation (severe pain with passive stretch, paresthesias, swelling) reflects **elevated intracompartmental pressure from reperfusion injury**, not rhabdomyolysis itself.
Organ preservation techniques US Medical PG Question 8: A 38-year-old kidney transplant recipient maintained on tacrolimus presents with a 2-week history of progressive confusion, ataxia, and visual disturbances. MRI shows multifocal white matter lesions without mass effect or enhancement. CSF analysis reveals mild pleocytosis with elevated protein. JC virus DNA is detected in CSF by PCR. Serum tacrolimus level is therapeutic at 8 ng/mL. Apply knowledge of this condition to determine the appropriate management strategy.
- A. Significantly reduce or discontinue immunosuppression and provide supportive care (Correct Answer)
- B. Switch from tacrolimus to sirolimus to preserve graft while treating infection
- C. Continue current immunosuppression and administer IVIG therapy
- D. Maintain immunosuppression and start cidofovir antiviral therapy
- E. Reduce tacrolimus by 50% and start high-dose corticosteroids
Organ preservation techniques Explanation: ***Significantly reduce or discontinue immunosuppression and provide supportive care***
- The patient presents with **Progressive Multifocal Leukoencephalopathy (PML)** caused by **JC virus** reactivation; the primary treatment is **immune reconstitution** to allow the body to fight the virus.
- Reducing or stopping agents like **tacrolimus** is critical for survival, even though it carries a high risk of **allograft rejection**.
*Switch from tacrolimus to sirolimus to preserve graft while treating infection*
- While **sirolimus** has some antiproliferative effects, it is still an **immunosuppressant** and will not allow for the aggressive immune recovery needed to halt **JC virus** replication.
- Managing the life-threatening neurological condition takes precedence over **graft preservation** in the acute phase of PML.
*Continue current immunosuppression and administer IVIG therapy*
- Maintaining current levels of **tacrolimus** prevents the T-cell mediated response necessary to clear the **JC virus** from the CNS.
- **IVIG therapy** has not been proven effective in clinical trials for the treatment of PML and does not address the underlying **immunosuppressed state**.
*Maintain immunosuppression and start cidofovir antiviral therapy*
- **Cidofovir** was previously studied for PML, but it has failed to show significant clinical benefit and is associated with severe **nephrotoxicity**.
- Antiviral therapy without addressing the **cellular immune deficiency** is insufficient to treat this opportunistic infection.
*Reduce tacrolimus by 50% and start high-dose corticosteroids*
- Adding **high-dose corticosteroids** is contraindicated as it further suppresses the immune system, potentially accelerating the progression of **PML**.
- Steroids are typically reserved only for patients who develop **Immune Reconstitution Inflammatory Syndrome (IRIS)** after immunosuppression is withdrawn.
Organ preservation techniques US Medical PG Question 9: A 41-year-old heart transplant recipient (5 years post-transplant) on cyclosporine, azathioprine, and prednisone develops progressive dyspnea on exertion. Echocardiogram shows preserved ejection fraction but abnormal diastolic dysfunction. Right heart catheterization reveals elevated filling pressures. Endomyocardial biopsy shows interstitial fibrosis without significant cellular infiltration. Coronary angiography shows diffuse, concentric narrowing of distal vessels. Synthesize these findings to determine the underlying pathophysiology and evaluate management options.
- A. Cardiac allograft vasculopathy requiring consideration for retransplantation evaluation (Correct Answer)
- B. Restrictive cardiomyopathy from previous rejection episodes requiring diuretic therapy
- C. Drug-induced cardiomyopathy from calcineurin inhibitor toxicity requiring switch to mTOR inhibitor
- D. Acute cellular rejection requiring pulse steroids and optimization of immunosuppression
- E. Antibody-mediated rejection requiring plasmapheresis and rituximab therapy
Organ preservation techniques Explanation: ***Cardiac allograft vasculopathy requiring consideration for retransplantation evaluation***
- **Cardiac allograft vasculopathy (CAV)** is the leading cause of late graft failure, characterized by **diffuse, concentric intimal hyperplasia** and narrowing of the distal coronary vessels.
- The presentation of **progressive dyspnea**, diastolic dysfunction, and **interstitial fibrosis** on biopsy—without acute cellular or antibody-mediated rejection—is pathognomonic for advanced CAV, where **retransplantation** remains the definitive surgical option.
*Restrictive cardiomyopathy from previous rejection episodes requiring diuretic therapy*
- While **interstitial fibrosis** can mimic a restrictive phenotype, this option overlooks the specific **angiographic finding** of distal concentric narrowing which points directly to CAV.
- **Diuretic therapy** may provide symptomatic relief for heart failure but does not address the underlying **progressive vasculopathy** and graft failure.
*Drug-induced cardiomyopathy from calcineurin inhibitor toxicity requiring switch to mTOR inhibitor*
- **Cyclosporine** (a calcineurin inhibitor) primarily causes **nephrotoxicity** and hypertension rather than direct cardiomyopathy with concentric vascular narrowing.
- While **mTOR inhibitors** (like Sirolimus) are used to slow the progression of CAV, they do not resolve established diffuse vascular disease with hemodynamic compromise.
*Acute cellular rejection requiring pulse steroids and optimization of immunosuppression*
- **Acute cellular rejection** is excluded by the endomyocardial biopsy, which specifically showed **no significant cellular infiltration**.
- This condition typically occurs earlier in the post-transplant period and would show **lymphocytic infiltration** and myocyte necrosis rather than concentric vessel narrowing.
*Antibody-mediated rejection requiring plasmapheresis and rituximab therapy*
- **Antibody-mediated rejection (AMR)** is characterized by **capillary endothelial injury** and C4d deposition on biopsy, which were not described in this patient.
- AMR typically presents with more acute graft dysfunction rather than the **slowly progressive** course and distal vessel pruning seen in this case.
Organ preservation techniques US Medical PG Question 10: A 52-year-old man with hepatocellular carcinoma (single 4.5 cm lesion) within Milan criteria is listed for liver transplantation with MELD exception points. While waiting, alpha-fetoprotein increases from 125 to 850 ng/mL over 3 months despite locoregional therapy. Repeat imaging shows the tumor has grown to 6 cm with possible vascular invasion. He has no extrahepatic disease. His wife offers to be a living donor. Synthesize the clinical data and evaluate the most appropriate management decision.
- A. Remove from transplant list and pursue systemic therapy with sorafenib (Correct Answer)
- B. Perform surgical resection then relist if recurrence occurs within criteria
- C. Downstage with aggressive locoregional therapy then reassess for transplantation
- D. Proceed with living donor transplantation given no extrahepatic disease
- E. Continue locoregional therapy and maintain listing with exception points
Organ preservation techniques Explanation: ***Remove from transplant list and pursue systemic therapy with sorafenib***
- This patient no longer meets the **Milan criteria** due to the lesion size exceeding 5 cm and the presence of suspected **vascular invasion**, which significantly increases the risk of recurrence.
- A rapid rise in **alpha-fetoprotein (AFP)** to >400 ng/mL is a strong predictor of poor post-transplant survival and biological aggressiveness, necessitating **delisting** and alternative systemic management.
*Perform surgical resection then relist if recurrence occurs within criteria*
- **Surgical resection** is generally contraindicated in cases of suspected **vascular invasion** as it is associated with extremely high rates of early systemic metastasis.
- This approach does not address the underlying biological aggressiveness evidenced by the soaring **AFP** and likely poor outcome.
*Downstage with aggressive locoregional therapy then reassess for transplantation*
- While **downstaging** is an option for tumors just outside criteria, the combination of **vascular invasion** and a rapidly rising **AFP** suggests the disease is no longer localized or controllable by these methods.
- Failure of previous **locoregional therapy** to control the AFP and tumor growth indicates a resistant phenotype that is unlikely to respond to further local intervention.
*Proceed with living donor transplantation given no extrahepatic disease*
- Even with a **living donor**, transplanting a patient with suspected **vascular invasion** and high **AFP** is ethically controversial due to the very high risk of rapid disease recurrence.
- **Living donor liver transplantation (LDLT)** does not bypass the need for favorable tumor biology to ensure a successful long-term oncologic outcome.
*Continue locoregional therapy and maintain listing with exception points*
- National matching rules generally require patients to stay within **Milan criteria** to maintain **MELD exception points**; exceeding 5 cm and vascular invasion disqualifies the patient.
- Maintaining the current status ignores the clear radiographic and biochemical evidence of **tumor progression**, which would result in a waste of a donor organ.
More Organ preservation techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.