Liver transplantation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Liver transplantation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Liver transplantation US Medical PG Question 1: A 60-year-old rock musician presents to the office because he has been feeling increasingly tired for the past 6 months. He has a history of intravenous drug use and alcohol abuse. He states that he feels quite tired, but he otherwise has no complaints. Physical examination is noncontributory. His laboratory values are normal other than moderately elevated liver enzymes. Which of the following additional tests should you order first?
- A. Hepatitis C virus antibodies (Correct Answer)
- B. Hepatitis B surface antigen
- C. Hepatitis E virus-specific IgM antibodies
- D. Hepatitis D virus-specific IgG antibody
- E. Hepatitis A virus-specific IgM antibodies
Liver transplantation Explanation: ***Hepatitis C virus antibodies***
- The patient's history of **intravenous drug use** and **chronic fatigue** with **elevated liver enzymes** strongly suggests chronic viral hepatitis, with hepatitis C being the most common blood-borne infection in persons with IVDU history.
- **Hepatitis C** is the **most prevalent chronic viral hepatitis** in the United States among persons with history of injection drug use, with transmission efficiency via needle sharing being very high.
- Hepatitis C often has a **long asymptomatic phase** (decades) before symptoms like fatigue and liver damage become apparent, making antibody testing the appropriate initial screen.
- While both HBV and HCV should ultimately be screened in this patient, **HCV prevalence is significantly higher** in the IVDU population, making it the priority initial test.
*Hepatitis B surface antigen*
- While **hepatitis B** can also be transmitted via intravenous drug use and cause chronic liver disease, **hepatitis C is more prevalent** in persons with IVDU history in the United States.
- **HBsAg** is used to detect active hepatitis B infection and should also be ordered, but given resource constraints and the clinical context, **anti-HCV is the higher-yield initial test**.
- Many IVDU patients have been vaccinated against HBV, further reducing its likelihood compared to HCV (for which no vaccine exists).
*Hepatitis E virus-specific IgM antibodies*
- **Hepatitis E** is typically transmitted via the **fecal-oral route** (contaminated water) and usually causes **acute, self-limiting hepatitis**, not chronic insidious fatigue and liver enzyme elevation in a Western patient.
- **IgM antibodies** would indicate an acute infection, which is less likely given the 6-month duration of symptoms.
- HEV rarely causes chronic infection except in immunocompromised patients.
*Hepatitis D virus-specific IgG antibody*
- **Hepatitis D** requires an existing **hepatitis B infection** to replicate (it's a satellite virus), meaning you would first need to confirm chronic hepatitis B before testing for HDV.
- While HDV can cause severe liver disease and is transmitted via blood exposure, it's not the initial test to pursue without evidence of HBV co-infection.
*Hepatitis A virus-specific IgM antibodies*
- **Hepatitis A** is transmitted via the **fecal-oral route** and causes an **acute, self-limiting infection** with complete resolution, rarely leading to chronic liver disease or persistent fatigue over 6 months.
- **IgM antibodies** are indicative of acute infection, which contradicts the chronic nature of the patient's symptoms.
- HAV does not cause chronic hepatitis.
Liver transplantation US Medical PG Question 2: A 22-year-old man is brought to the emergency department by ambulance 1 hour after a motor vehicle accident. He did not require any circulatory resuscitation at the scene, but he was intubated because he was unresponsive. He has no history of serious illnesses. He is on mechanical ventilation with no sedation. His blood pressure is 121/62 mm Hg, the pulse is 68/min, and the temperature is 36.5°C (97.7°F). His Glasgow coma scale (GCS) is 3. Early laboratory studies show no abnormalities. A search of the state donor registry shows that he has registered as an organ donor. Which of the following is the most appropriate next step in evaluation?
- A. Evaluation of brainstem reflexes (Correct Answer)
- B. Brain MRI
- C. Electroencephalography
- D. Cerebral angiography
- E. Apnea test
Liver transplantation Explanation: ***Evaluation of brainstem reflexes***
- In a patient with a **Glasgow Coma Scale (GCS) of 3** and no response to noxious stimuli/sedation, assessment of **brainstem reflexes** is a critical step in determining brain death.
- This evaluation includes checking for pupillary light reflex, corneal reflex, vestibulo-ocular reflex (doll's eyes), oculocephalic reflex, and gag/cough reflexes to ascertain the complete absence of brainstem function.
*Brain MRI*
- While a brain MRI can provide detailed anatomical information regarding brain injury, it is **not the primary diagnostic test** for determining brain death.
- Brain death is a **clinical diagnosis** based on the irreversible loss of brain and brainstem function, which can be confirmed rapidly by clinical examination.
*Electroencephalography*
- **EEG** measures electrical activity in the brain and can show electrocerebral silence, which is consistent with brain death.
- However, EEG is **not always required** for the diagnosis of brain death and is often used as a confirmatory test in specific situations, such as when clinical examination is inconclusive or legal requirements necessitate it.
*Cerebral angiography*
- **Cerebral angiography** can demonstrate the absence of cerebral blood flow, which is a criterion for brain death.
- This is an **invasive procedure** and is generally reserved for situations where clinical examination tests are difficult to perform or interpret (e.g., severe facial trauma, drug intoxication), and is not the initial step.
*Apnea test*
- The **apnea test** is a critical component of the brain death evaluation, confirming the absence of spontaneous breathing response to hypercapnia.
- It is performed **after the absence of brainstem reflexes** has been established and all confounding factors (e.g., hypothermia, hypotension, sedatives) have been ruled out.
Liver transplantation US Medical PG Question 3: A patient with HCC and a long history of alcohol dependence and chronic hepatitis C has been using the mTOR inhibitor sirolimus 100 mg for cancer treatment. Her cancer has shown a partial response. She also has a history of hypertension and poorly controlled type 2 diabetes mellitus complicated by diabetic retinopathy. Current medications include enalapril and insulin. She asks her oncologist and hepatologist if she could try everolimus for its purported survival benefit in treating HCC. Based on clinical considerations, which of the following statements is most accurate?
- A. The patient should start everolimus 50 mg because of the survival benefit relative to sirolimus 100 mg
- B. The patient is not a good candidate for everolimus due to her history of hypertension
- C. The patient should start everolimus 100 mg because of the survival benefit relative to sirolimus 100 mg
- D. The patient should start everolimus 50 mg because of her history of alcohol use disorder and hepatitis C
- E. The patient is not a good candidate for everolimus due to her history of diabetes (Correct Answer)
Liver transplantation Explanation: ***The patient is not a good candidate for Noxbinle due to her history of diabetes***
- The current medication is sirolimus, an **mTOR inhibitor** and its successor everolimus, also an mTOR inhibitor, is not beneficial for this patient due to her **poorly controlled type 2 diabetes mellitus**.
- mTOR inhibitors, including everolimus, are known to **worsen hyperglycemia** and **accelerate the progression of diabetes**, making it contraindicated in patients with already complicated diabetes.
*The patient should start everolimus 50 mg because of the survival benefit relative to sirolimus 100 mg*
- There is **no established evidence** that everolimus at any dose offers a superior survival benefit compared to sirolimus in HCC, particularly after a partial response to sirolimus.
- **Switching mTOR inhibitors** without a compelling clinical reason, especially with existing comorbidities, is not standard practice.
*The patient is not a good candidate for everolimus due to her history of hypertension*
- While mTOR inhibitors can contribute to **hypertension**, this patient is already on **enalapril** for her existing hypertension.
- Her **poorly controlled diabetes** presents a more direct and severe contraindication due to the metabolic side effects of everolimus.
*The patient should start everolimus 100 mg because of the survival benefit relative to sirolimus 100 mg*
- No clinical data supports a **superior survival benefit** of everolimus 100 mg over sirolimus 100 mg in HCC.
- Given the patient's existing **poorly controlled diabetes**, increasing the dose of an mTOR inhibitor or switching to an equivalent dose of another would heighten the risk of severe metabolic complications.
*The patient should start everolimus 50 mg because of her history of alcohol use disorder and hepatitis C*
- The patient's history of alcohol dependence and chronic hepatitis C are **risk factors for HCC** but do not directly contraindicate a specific dose of everolimus more than her diabetes.
- While liver impairment due to these conditions might influence dosing of various medications, the **primary concern for everolimus** in this case remains the uncontrolled diabetes.
Liver transplantation US Medical PG Question 4: A 56-year-old woman is brought to the emergency department by her family with altered mental status. Her husband says that she complained of fever, vomiting, and abdominal pain 2 days ago. She has a history of long-standing alcoholism and previous episodes of hepatic encephalopathy. Current vital signs include a temperature of 38.3°C (101°F), blood pressure of 85/60 mm Hg, pulse of 95/min, and a respiratory rate 30/min. On physical examination, the patient appears ill and obtunded. She is noted to have jaundice, a palpable firm liver, and massive abdominal distension with shifting dullness. Which of the following is the best initial step in management of this patient's condition?
- A. Empiric antibiotics (Correct Answer)
- B. Diagnostic paracentesis
- C. Large volume paracentesis
- D. Intravenous albumin
- E. Non-selective beta-blockers
Liver transplantation Explanation: ***Empiric antibiotics***
- This patient presents with **altered mental status**, **fever**, **hypotension (85/60 mm Hg)**, **tachypnea**, and **massive ascites** in the setting of **cirrhosis**, indicating **suspected spontaneous bacterial peritonitis (SBP) with septic shock**.
- In a **hemodynamically unstable patient** with suspected SBP, **empiric antibiotics** (typically a third-generation cephalosporin like ceftriaxone or cefotaxime) should be initiated **immediately** without waiting for diagnostic paracentesis results.
- Current **AASLD and EASL guidelines** emphasize that antibiotic therapy should not be delayed in critically ill patients, as early treatment significantly reduces mortality in SBP.
- Diagnostic paracentesis should still be performed urgently but should **not delay antibiotic administration** in this unstable patient.
*Diagnostic paracentesis*
- While **diagnostic paracentesis** is the gold standard for confirming SBP and should be performed promptly, it is not the **best initial step** in a hemodynamically unstable patient.
- In this critically ill patient with septic shock, obtaining ascitic fluid can be done **simultaneously with** or **immediately after** starting antibiotics, but antibiotics take priority.
- If the patient were stable, diagnostic paracentesis before antibiotics would be appropriate to guide therapy.
*Large volume paracentesis*
- **Large volume paracentesis** is indicated for symptomatic relief of tense ascites causing respiratory compromise, not as an initial step in suspected infection.
- In the setting of suspected SBP, only diagnostic paracentesis (50-100 mL) is needed initially, not large volume removal.
*Intravenous albumin*
- **Intravenous albumin** is given as adjunctive therapy in SBP patients with **renal dysfunction** (creatinine >1 mg/dL, BUN >30 mg/dL) or **hypotension** to prevent hepatorenal syndrome.
- While this patient may benefit from albumin, it is not the **initial step**—antibiotics and fluid resuscitation take priority.
- Albumin is typically given at 1.5 g/kg within 6 hours and 1 g/kg on day 3.
*Non-selective beta-blockers*
- **Non-selective beta-blockers** (propranolol, nadolol) are used for **primary and secondary prophylaxis of variceal bleeding** in portal hypertension.
- They are **contraindicated** in patients with **hypotension** (BP 85/60 mm Hg), **sepsis**, or **SBP**, as they can worsen hemodynamic instability.
- Recent studies suggest beta-blockers may be harmful in patients with refractory ascites or SBP.
Liver transplantation US Medical PG Question 5: A 67-year-old man is seen on the surgical floor after a transplant procedure. The previous day, the patient had a renal transplant from a matched donor. He is currently recovering and doing well. The patient has a past medical history of IV drug use, diabetes mellitus, oral cold sores, hypertension, renal failure, and dyslipidemia. The patient's current medications include lisinopril, atorvastatin, insulin, and aspirin. Prior to the procedure, he was also on dialysis. The patient is started on cyclosporine. The patient successfully recovers over the next few days. Which of the following medications should be started in this patient?
- A. Azithromycin
- B. TMP-SMX (Correct Answer)
- C. Acyclovir
- D. Low dose acyclovir
- E. Penicillin
Liver transplantation Explanation: ***TMP-SMX***
- **TMP-SMX (trimethoprim-sulfamethoxazole)** is the **most critical** prophylactic medication for all solid organ transplant recipients on immunosuppression.
- It provides essential prophylaxis against **Pneumocystis jirovecii pneumonia (PJP)**, a life-threatening opportunistic infection with high mortality if not prevented.
- PJP prophylaxis is a **universal recommendation** for all transplant patients and is typically continued for 6-12 months post-transplant.
- Additionally offers protection against **Toxoplasma gondii**, **Nocardia**, and common urinary tract infections, making it particularly valuable in renal transplant recipients.
*Azithromycin*
- Azithromycin is a macrolide antibiotic used for specific bacterial infections and sometimes for **Mycobacterium avium complex (MAC)** prophylaxis in severely immunocompromised patients.
- It is not standard prophylaxis in routine post-transplant care and does not protect against PJP, the most critical opportunistic infection in this setting.
*Acyclovir*
- High-dose acyclovir is used to **treat active HSV or VZV infections**, not for routine prophylaxis.
- This patient has no active viral infection requiring treatment doses at this time.
*Low dose acyclovir*
- Low-dose acyclovir (or valacyclovir) is indeed used for **HSV/VZV prophylaxis** in transplant patients, especially those with a history of cold sores.
- Many transplant centers do initiate this medication alongside TMP-SMX in the post-transplant period.
- However, in a **single-best-answer** context, **TMP-SMX takes priority** as it prevents PJP, which is universally life-threatening and has higher incidence without prophylaxis compared to severe HSV reactivation.
- TMP-SMX is considered the **essential first-line** prophylaxis that all transplant patients must receive.
*Penicillin*
- Penicillin is a narrow-spectrum antibiotic effective against certain gram-positive bacteria.
- It has no role in post-transplant opportunistic infection prophylaxis and does not protect against PJP, HSV, or other transplant-related infections.
Liver transplantation US Medical PG Question 6: An epidemiologist is evaluating the efficacy of Noxbinle in preventing HCC deaths at the population level. A clinical trial shows that over 5 years, the mortality rate from HCC was 25% in the control group and 15% in patients treated with Noxbinle 100 mg daily. Based on this data, how many patients need to be treated with Noxbinle 100 mg to prevent, on average, one death from HCC?
- A. 20
- B. 73
- C. 10 (Correct Answer)
- D. 50
- E. 100
Liver transplantation Explanation: ***10***
- The **number needed to treat (NNT)** is calculated by first finding the **absolute risk reduction (ARR)**.
- **ARR** = Risk in control group - Risk in treatment group = 25% - 15% = **10%** (or 0.10).
- **NNT = 1 / ARR** = 1 / 0.10 = **10 patients**.
- This means that **10 patients must be treated with Noxbinle to prevent one death from HCC** over 5 years.
*20*
- This would result from an ARR of 5% (1/0.05 = 20), which is not supported by the data.
- May arise from miscalculating the risk difference or incorrectly halving the actual ARR.
*73*
- This value does not correspond to any standard calculation of NNT from the given mortality rates.
- May result from confusion with other epidemiological measures or calculation error.
*50*
- This would correspond to an ARR of 2% (1/0.02 = 50), which significantly underestimates the actual risk reduction.
- Could result from incorrectly calculating the difference as a proportion rather than absolute percentage points.
*100*
- This would correspond to an ARR of 1% (1/0.01 = 100), grossly underestimating the treatment benefit.
- May result from confusing ARR with relative risk reduction or other calculation errors.
Liver transplantation US Medical PG Question 7: A 57-year-old man presents to the emergency department with fatigue. He states that his symptoms started yesterday and have been worsening steadily. The patient endorses a recent weight loss of 7 pounds this past week and states that he feels diffusely itchy. The patient has a past medical history of alcohol abuse, obesity, asthma, and IV drug use. His current medications include metformin, atorvastatin, albuterol, and fluticasone. In addition, the patient admits to smoking and drinking more than usual lately due to the stress he has experienced. His temperature is 98.7°F (37.1°C), blood pressure is 130/75 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam is notable for an ill-appearing man. The patient's skin appears yellow. Abdominal exam is notable for right upper quadrant tenderness. Cardiac and pulmonary exams are within normal limits. Laboratory values are ordered as seen below:
Hemoglobin: 14 g/dL
Hematocrit: 42%
Leukocyte count: 5,500 cells/mm^3 with normal differential
Platelet count: 70,000/mm^3
Partial thromboplastin time: 92 seconds
Prothrombin time: 42 seconds
AST: 1110 U/L
ALT: 990 U/L
Which of the following is most likely to be found in this patient's history?
- A. Recent antibiotic treatment with gentamicin
- B. Appropriate acute management of a deep vein thrombosis
- C. Decreased UDP-glucuronosyltransferase activity at birth
- D. Prosthetic valve with appropriate post-operative care
- E. Severe migraine headaches treated with acetaminophen (Correct Answer)
Liver transplantation Explanation: ***Severe migraine headaches treated with acetaminophen***
- The patient's presentation with **acute liver failure** (elevated AST/ALT, coagulopathy, jaundice) in the context of increased stress and likely increased medication use, strongly suggests **acetaminophen overdose** as the cause. Given his past medical history of alcohol abuse further increases his risk of liver injury with acetaminophen.
- While other etiologies such as acute viral hepatitis or ischemic hepatitis should be considered, acetaminophen overdose is the most common cause of acute liver failure.
*Recent antibiotic treatment with gentamicin*
- **Gentamicin** is an **aminoglycoside antibiotic** primarily associated with **nephrotoxicity** and **ototoxicity**, not acute liver failure.
- Liver dysfunction is not a typical adverse effect of gentamicin, making it an unlikely cause of the patient's symptoms.
*Appropriate acute management of a deep vein thrombosis*
- Treatment for deep vein thrombosis typically involves **anticoagulants** such as heparin or warfarin. While these medications can rarely cause liver injury, the severe and acute elevation in liver enzymes and coagulopathy seen here points away from a standard anticoagulant side effect.
- The clinical picture aligns much more closely with a direct hepatotoxic injury rather than an idiosyncratic reaction to anticoagulation.
*Decreased UDP-glucuronosyltransferase activity at birth*
- **Decreased UDP-glucuronosyltransferase (UGT) activity** at birth is characteristic of **Crigler-Najjar syndrome** or **Gilbert's syndrome**, which cause **unconjugated hyperbilirubinemia**.
- These are typically chronic conditions that present earlier in life and do not cause acute, severe hepatocellular injury with massively elevated AST/ALT and coagulopathy.
*Prosthetic valve with appropriate post-operative care*
- A prosthetic heart valve, even with appropriate post-operative care, is not directly linked to acute liver failure.
- While complications like endocarditis or hemolysis could cause some liver involvement, they would not typically present with this constellation of severe acute symptoms and laboratory findings.
Liver transplantation US Medical PG Question 8: A 58-year-old man is brought to the emergency department because of confusion, weight loss, and anuria. He has chronic kidney disease, hypertension, and type 2 diabetes mellitus. He was diagnosed with acute lymphoblastic leukemia at the age of 8 years and was treated with an allogeneic stem cell transplantation. He is HIV-positive and has active hepatitis C virus infection. He drinks around 8 cans of beer every week. His current medications include tenofovir, emtricitabine, atazanavir, daclatasvir, sofosbuvir, insulin, amlodipine, and enalapril. He appears lethargic. His temperature is 36°C (96.8°F), pulse is 130/min, respirations are 26/min, and blood pressure is 145/90 mm Hg. Examination shows severe edema in his legs and generalized muscular weakness. Auscultation of the lung shows crepitant rales. Laboratory studies show positive HCV antibody and positive HCV RNA. His HIV viral load is undetectable and his CD4+ T-lymphocyte count is 589/μL. Six months ago, his CD4+ T-lymphocyte count was 618/μL. An ECG of the heart shows arrhythmia with frequent premature ventricular contractions. Arterial blood gas analysis on room air shows:
pH 7.23
PCO2 31 mm Hg
HCO3- 13 mEq/L
Base excess -12 mEq/L
The patient states he would like to donate organs or tissues in the case of his death. Which of the following is an absolute contraindication for organ donation in this patient?
- A. HIV infection
- B. Childhood leukemia (Correct Answer)
- C. Alcoholism
- D. No absolute contraindications
- E. Acute kidney injury
Liver transplantation Explanation: ***Correct: Childhood leukemia***
- **History of hematologic malignancy** (including acute lymphoblastic leukemia) is an **absolute contraindication** for solid organ donation according to UNOS and OPTN guidelines.
- Even though this patient was treated 50 years ago with allogeneic stem cell transplantation, the concern for **residual malignant cells** or **transmission to immunosuppressed recipients** makes this an absolute exclusion.
- Unlike solid tumors (which may be acceptable after long disease-free intervals), **leukemias and lymphomas carry lifelong exclusion** from organ donation due to their systemic nature and potential for dormant cells.
*Incorrect: Acute kidney injury*
- **Acute kidney injury (AKI)** is NOT an absolute contraindication for organ donation.
- While the kidneys themselves may not be suitable for transplantation, other organs (heart, liver, lungs, corneas) could still be viable.
- Each organ is assessed individually for suitability.
*Incorrect: HIV infection*
- **Well-controlled HIV infection** (undetectable viral load, stable CD4 count >200) is no longer an absolute contraindication.
- Under the **HOPE Act (HIV Organ Policy Equity Act)**, organs from HIV-positive donors can be transplanted into HIV-positive recipients.
- This patient has excellent viral control (undetectable VL, CD4 589), making HIV not an absolute barrier.
*Incorrect: Alcoholism*
- **Alcohol use disorder** alone is not an absolute contraindication for organ donation.
- The suitability depends on individual organ assessment (e.g., liver function, cardiac health).
- This patient drinks 8 beers/week, which is moderate consumption and doesn't preclude donation of undamaged organs.
*Incorrect: No absolute contraindications*
- This patient **does have an absolute contraindication**: his history of hematologic malignancy (acute lymphoblastic leukemia).
- Despite the long time since treatment, hematologic cancers remain absolute exclusions for organ donation.
Liver transplantation US Medical PG Question 9: A 37-year-old man who had undergone liver transplantation 7 years ago, presents to the physician because of yellowish discoloration of the skin, sclera, and urine. He is on regular immunosuppressive therapy and is well-adherent to the treatment. He has no comorbidities and is not taking any other medication. He provides a history of similar episodes of yellowish skin discoloration 6–7 times since he underwent liver transplantation. Physical examination shows clinical jaundice. Laboratory studies show:
While blood cell (WBC) count 4,400/mm3
Hemoglobin 11.1 g/dL
Serum creatinine 0.9 mg/dL
Serum bilirubin (total) 44 mg/dL
Aspartate transaminase (AST) 1,111 U/L
Alanine transaminase (ALT) 671 U/L
Serum gamma-glutamyl transpeptidase 777 U/L
Alkaline phosphatase 888 U/L
Prothrombin time 17 seconds
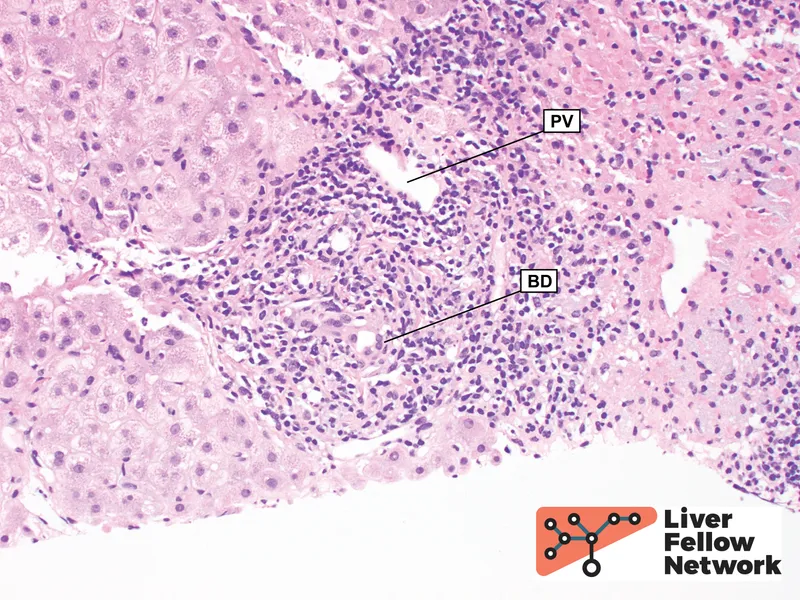
A Doppler ultrasound shows significantly reduced blood flow into the transplanted liver. A biopsy of the transplanted liver is likely to show which of the following histological features?
- A. Ballooning degeneration of hepatocytes
- B. Normal architecture of bile ducts and hepatocytes
- C. Irregularly shaped nodules of regenerating hepatocytes with peripheral halo
- D. Broad fibrous septations with formation of micronodules
- E. Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis (Correct Answer)
Liver transplantation Explanation: ***Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis***
- The patient's history of **repeated jaundice episodes** after liver transplantation, coupled with **elevated liver enzymes** and **significantly reduced transplanted liver blood flow** on Doppler, points to **chronic rejection**.
- **Chronic rejection** is histologically characterized by **interstitial cellular infiltration**, **parenchymal fibrosis**, and hallmark **obliterative arteritis**, which describes the progressive luminal narrowing and obliteration of hepatic arteries due to intimal proliferation.
*Ballooning degeneration of hepatocytes*
- This feature is typically associated with **acute hepatitis**, often viral or alcoholic, and indicates **hepatocyte swelling and necrosis**.
- While reflecting liver injury, it doesn't specifically point to **chronic rejection** in a transplanted liver with repeated episodes and vascular changes.
*Normal architecture of bile ducts and hepatocytes*
- This finding would suggest a **healthy liver** or a successful response to treatment, which contradicts the patient's symptoms of **jaundice**, highly elevated **liver enzymes**, and **reduced blood flow**.
- The presence of clinical symptoms and abnormal lab values rules out a normal liver architecture.
*Irregularly shaped nodules of regenerating hepatocytes with peripheral halo*
- This description is characteristic of **biliary hamartomas** (von Meyenburg complexes) or focal nodular hyperplasia, which are typically benign lesions and not indicative of the **severe liver injury** seen here.
- It does not align with the progressive nature of the patient's recurrent jaundice and vascular compromise identified.
*Broad fibrous septations with formation of micronodules*
- This histological pattern is typical of **cirrhosis**, a condition characterized by diffuse **fibrosis** and the formation of **regenerative nodules**, often resulting from chronic liver diseases like hepatitis or alcohol abuse.
- While fibrosis is part of chronic rejection, the description does not capture the specific **vascular and inflammatory changes** of **obliterative arteritis** that are central to chronic rejection.
Liver transplantation US Medical PG Question 10: A 38-year-old kidney transplant recipient maintained on tacrolimus presents with a 2-week history of progressive confusion, ataxia, and visual disturbances. MRI shows multifocal white matter lesions without mass effect or enhancement. CSF analysis reveals mild pleocytosis with elevated protein. JC virus DNA is detected in CSF by PCR. Serum tacrolimus level is therapeutic at 8 ng/mL. Apply knowledge of this condition to determine the appropriate management strategy.
- A. Significantly reduce or discontinue immunosuppression and provide supportive care (Correct Answer)
- B. Switch from tacrolimus to sirolimus to preserve graft while treating infection
- C. Continue current immunosuppression and administer IVIG therapy
- D. Maintain immunosuppression and start cidofovir antiviral therapy
- E. Reduce tacrolimus by 50% and start high-dose corticosteroids
Liver transplantation Explanation: ***Significantly reduce or discontinue immunosuppression and provide supportive care***
- The patient presents with **Progressive Multifocal Leukoencephalopathy (PML)** caused by **JC virus** reactivation; the primary treatment is **immune reconstitution** to allow the body to fight the virus.
- Reducing or stopping agents like **tacrolimus** is critical for survival, even though it carries a high risk of **allograft rejection**.
*Switch from tacrolimus to sirolimus to preserve graft while treating infection*
- While **sirolimus** has some antiproliferative effects, it is still an **immunosuppressant** and will not allow for the aggressive immune recovery needed to halt **JC virus** replication.
- Managing the life-threatening neurological condition takes precedence over **graft preservation** in the acute phase of PML.
*Continue current immunosuppression and administer IVIG therapy*
- Maintaining current levels of **tacrolimus** prevents the T-cell mediated response necessary to clear the **JC virus** from the CNS.
- **IVIG therapy** has not been proven effective in clinical trials for the treatment of PML and does not address the underlying **immunosuppressed state**.
*Maintain immunosuppression and start cidofovir antiviral therapy*
- **Cidofovir** was previously studied for PML, but it has failed to show significant clinical benefit and is associated with severe **nephrotoxicity**.
- Antiviral therapy without addressing the **cellular immune deficiency** is insufficient to treat this opportunistic infection.
*Reduce tacrolimus by 50% and start high-dose corticosteroids*
- Adding **high-dose corticosteroids** is contraindicated as it further suppresses the immune system, potentially accelerating the progression of **PML**.
- Steroids are typically reserved only for patients who develop **Immune Reconstitution Inflammatory Syndrome (IRIS)** after immunosuppression is withdrawn.
More Liver transplantation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.