Immunosuppression principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Immunosuppression principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Immunosuppression principles US Medical PG Question 1: A 56-year-old man comes to the emergency department because of progressively worsening shortness of breath and fever for 2 days. He also has a nonproductive cough. He does not have chest pain or headache. He has chronic myeloid leukemia and had a bone marrow transplant 3 months ago. His current medications include busulfan, mycophenolate mofetil, tacrolimus, and methylprednisolone. His temperature is 38.1°C (100.6°F), pulse is 103/min, respirations are 26/min, and blood pressure is 130/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 93%. Pulmonary examination shows diffuse crackles. The spleen tip is palpated 4 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.3 g/dL
Leukocyte count 4,400/mm3
Platelet count 160,000/mm3
Serum
Glucose 78 mg/dL
Creatinine 2.1 mg/dL
D-dimer 96 ng/mL (N < 250)
pp65 antigen positive
Galactomannan antigen negative
Urinalysis is normal. An x-ray of the chest shows diffuse bilateral interstitial infiltrates. An ECG shows sinus tachycardia. Which of the following is the most appropriate pharmacotherapy?
- A. Levofloxacin
- B. Ganciclovir (Correct Answer)
- C. Valganciclovir
- D. Azithromycin
- E. Acyclovir
Immunosuppression principles Explanation: ***Ganciclovir***
- The patient's **positive pp65 antigen** confirms **cytomegalovirus (CMV) infection**, the most common viral infection in immunocompromised bone marrow transplant recipients.
- This patient has **severe, life-threatening CMV pneumonitis** evidenced by hypoxia (O2 sat 93%), tachypnea, and diffuse bilateral interstitial infiltrates.
- **Intravenous ganciclovir** is the **first-line treatment** for severe CMV disease due to its potent antiviral activity and reliable bioavailability in critically ill patients.
*Valganciclovir*
- **Valganciclovir** is an **oral prodrug of ganciclovir** with excellent bioavailability, but it is primarily reserved for **CMV prophylaxis** or **maintenance therapy** after initial IV treatment.
- In this patient with **acute, severe CMV pneumonitis** requiring urgent intervention (hypoxia, respiratory distress), **IV ganciclovir is strongly preferred** for faster, more reliable drug delivery and higher tissue concentrations.
*Levofloxacin*
- This **fluoroquinolone antibiotic** treats **bacterial infections**, not viral pathogens like CMV.
- The **positive pp65 antigen** specifically identifies CMV as the etiology, and negative galactomannan rules out invasive aspergillosis.
- While empiric antibacterial coverage might be considered in febrile neutropenic patients, the clear viral diagnosis directs therapy toward antivirals.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic effective against atypical bacteria (Mycoplasma, Chlamydophila) and some other bacterial pathogens.
- It has **no activity against CMV** and would not address the confirmed viral etiology.
*Acyclovir*
- **Acyclovir** is effective against **herpes simplex virus (HSV)** and **varicella-zoster virus (VZV)**, but has **poor activity against CMV** due to inadequate phosphorylation by CMV enzymes.
- The positive pp65 antigen specifically indicates CMV, for which ganciclovir (not acyclovir) is required.
Immunosuppression principles US Medical PG Question 2: A 37-year-old man who had undergone liver transplantation 7 years ago, presents to the physician because of yellowish discoloration of the skin, sclera, and urine. He is on regular immunosuppressive therapy and is well-adherent to the treatment. He has no comorbidities and is not taking any other medication. He provides a history of similar episodes of yellowish skin discoloration 6–7 times since he underwent liver transplantation. Physical examination shows clinical jaundice. Laboratory studies show:
While blood cell (WBC) count 4,400/mm3
Hemoglobin 11.1 g/dL
Serum creatinine 0.9 mg/dL
Serum bilirubin (total) 44 mg/dL
Aspartate transaminase (AST) 1,111 U/L
Alanine transaminase (ALT) 671 U/L
Serum gamma-glutamyl transpeptidase 777 U/L
Alkaline phosphatase 888 U/L
Prothrombin time 17 seconds
A Doppler ultrasound shows significantly reduced blood flow into the transplanted liver. A biopsy of the transplanted liver is likely to show which of the following histological features?
- A. Ballooning degeneration of hepatocytes
- B. Normal architecture of bile ducts and hepatocytes
- C. Irregularly shaped nodules of regenerating hepatocytes with peripheral halo
- D. Broad fibrous septations with formation of micronodules
- E. Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis (Correct Answer)
Immunosuppression principles Explanation: ***Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis***
- The patient's history of **repeated jaundice episodes** after liver transplantation, coupled with **elevated liver enzymes** and **significantly reduced transplanted liver blood flow** on Doppler, points to **chronic rejection**.
- **Chronic rejection** is histologically characterized by **interstitial cellular infiltration**, **parenchymal fibrosis**, and hallmark **obliterative arteritis**, which describes the progressive luminal narrowing and obliteration of hepatic arteries due to intimal proliferation.
*Ballooning degeneration of hepatocytes*
- This feature is typically associated with **acute hepatitis**, often viral or alcoholic, and indicates **hepatocyte swelling and necrosis**.
- While reflecting liver injury, it doesn't specifically point to **chronic rejection** in a transplanted liver with repeated episodes and vascular changes.
*Normal architecture of bile ducts and hepatocytes*
- This finding would suggest a **healthy liver** or a successful response to treatment, which contradicts the patient's symptoms of **jaundice**, highly elevated **liver enzymes**, and **reduced blood flow**.
- The presence of clinical symptoms and abnormal lab values rules out a normal liver architecture.
*Irregularly shaped nodules of regenerating hepatocytes with peripheral halo*
- This description is characteristic of **biliary hamartomas** (von Meyenburg complexes) or focal nodular hyperplasia, which are typically benign lesions and not indicative of the **severe liver injury** seen here.
- It does not align with the progressive nature of the patient's recurrent jaundice and vascular compromise identified.
*Broad fibrous septations with formation of micronodules*
- This histological pattern is typical of **cirrhosis**, a condition characterized by diffuse **fibrosis** and the formation of **regenerative nodules**, often resulting from chronic liver diseases like hepatitis or alcohol abuse.
- While fibrosis is part of chronic rejection, the description does not capture the specific **vascular and inflammatory changes** of **obliterative arteritis** that are central to chronic rejection.
Immunosuppression principles US Medical PG Question 3: A 43-year-old woman comes to the office with a 5-day history of a rash. She's had a rash across her neck, shoulders, and the palms of her hands for the past five days. She's also had large-volume watery diarrhea for the same period of time. Past medical history is notable for acute myeloid leukemia, for which she received a stem cell transplant from a donor about two months prior. Physical exam reveals a faint red maculopapular rash across her neck, shoulders, and hands, as well as an enlarged liver and spleen. Labs are notable for a total bilirubin of 10. Which of the following is the mechanism of this patient's pathology?
- A. Drug hypersensitivity reaction
- B. Host CD8+ T cells against graft antigens
- C. Graft T cells against host antigens (Correct Answer)
- D. Pre-existing host antibodies against graft antigens
- E. Host antibodies that have developed against graft antigens
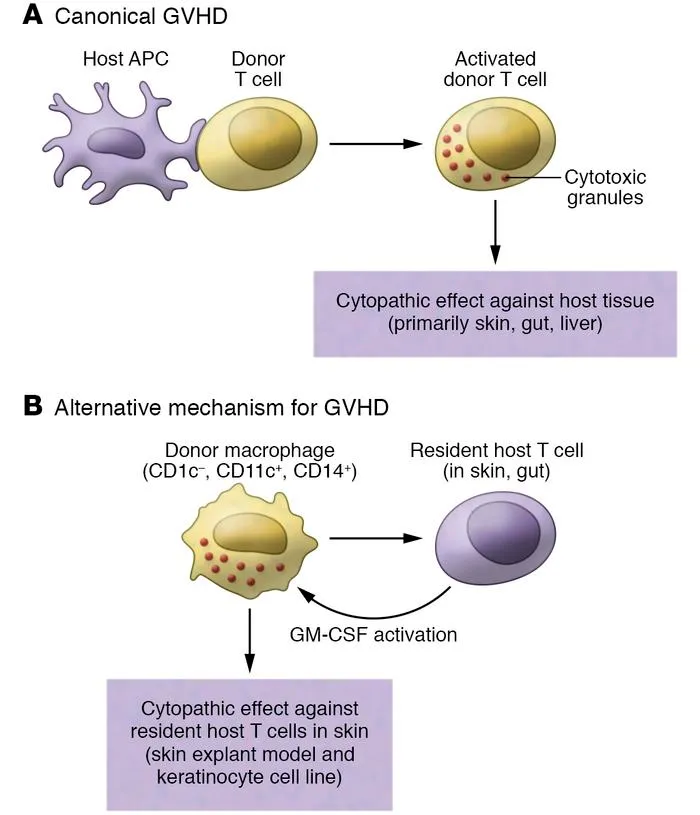
Immunosuppression principles Explanation: ***Graft T cells against host antigens***
- This patient's symptoms (rash, diarrhea, hepatosplenomegaly, elevated bilirubin) occurring after a stem cell transplant are classic for **graft-versus-host disease (GVHD)**.
- GVHD occurs when **donor T cells** from the graft recognize the recipient's (host's) tissues as foreign and mount an immune attack against them.
*Drug hypersensitivity reaction*
- While drug rashes can occur, the widespread nature, severe GI involvement (large-volume watery diarrhea), and liver dysfunction, especially in the context of a recent stem cell transplant, point away from a simple **hypersensitivity reaction**.
- A drug reaction would typically not cause such severe systemic effects or splenomegaly.
*Host CD8+ T cells against graft antigens*
- This describes **host-versus-graft rejection**, where the recipient's immune system attacks the transplanted cells.
- In a stem cell transplant setting, the host's immune system is typically severely suppressed to prevent this, and the clinical picture here is characteristic of the donor cells attacking the host.
*Pre-existing host antibodies against graft antigens*
- Pre-existing antibodies would cause a **hyperacute or acute rejection** much earlier after transplantation, often within minutes to days.
- This patient's symptoms developed two months post-transplant, which is more typical for acute GVHD, mediated by T cells.
*Host antibodies that have developed against graft antigens*
- The development of host antibodies against graft antigens would lead to **humoral rejection**, which typically manifests differently and less commonly causes the specific constellation of symptoms seen here (skin rash, severe diarrhea, cholestatic hepatitis in the context of stem cell transplant).
- T-cell-mediated responses are the primary drivers of GVHD in this scenario.
Immunosuppression principles US Medical PG Question 4: A 14-year-old boy has undergone kidney transplantation due to stage V chronic kidney disease. A pre-transplantation serologic assessment showed that he is negative for past or present HIV infection, viral hepatitis, EBV, and CMV infection. He has a known allergy for macrolides. The patient has no complaints 1 day after transplantation. His vital signs include: blood pressure 120/70 mm Hg, heart rate 89/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, the patient appears to be pale, his lungs are clear on auscultation, heart sounds are normal, and his abdomen is non-tender on palpation. His creatinine is 0.65 mg/dL (57.5 µmol/L), GFR is 71.3 mL/min/1.73 m2, and urine output is 0.9 mL/kg/h. Which of the following drugs should be used in the immunosuppressive regimen in this patient?
- A. Belatacept
- B. Sirolimus
- C. Omalizumab
- D. Daclizumab
- E. Basiliximab (Correct Answer)
Immunosuppression principles Explanation: **Basiliximab**
- **Basiliximab** is a **monoclonal antibody** that targets the **IL-2 receptor (CD25)** on activated T cells, preventing their proliferation and inducing immunosuppression.
- It is commonly used as **induction therapy** in kidney transplant recipients due to its good safety profile, especially in pediatric patients, without the nephrotoxicity associated with calcineurin inhibitors, minimizing acute rejection risks immediately post-transplant.
*Belatacept*
- **Belatacept** works by co-stimulation blockade, binding to **CD80 and CD86** on antigen-presenting cells to prevent T-cell activation.
- It is typically reserved for patients who cannot tolerate calcineurin inhibitors due to **nephrotoxicity** or require a steroid-sparing regimen, which is not indicated as an immediate need in this patient.
*Sirolimus*
- **Sirolimus** is an **mTOR inhibitor** that works by blocking T-cell proliferation and B-cell differentiation.
- It is associated with several side effects, including **delayed wound healing**, **thrombocytopenia**, and **hyperlipidemia**, which are undesirable in the immediate post-transplant period, especially in a growing adolescent.
*Omalizumab*
- **Omalizumab** is an **anti-IgE monoclonal antibody** primarily used for allergic asthma and chronic spontaneous urticaria.
- It has no role in **immunosuppression for organ transplantation** as its mechanism of action is unrelated to preventing graft rejection.
*Daclizumab*
- **Daclizumab** is another **monoclonal antibody** that also targets the **IL-2 receptor (CD25)**, similar to basiliximab.
- However, daclizumab has been **withdrawn from the market** due to serious adverse effects including severe liver injury and autoimmune encephalitis, making it unavailable for clinical use in transplantation.
Immunosuppression principles US Medical PG Question 5: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
Immunosuppression principles Explanation: ***Renal failure***
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
Immunosuppression principles US Medical PG Question 6: Fourteen days after a laparoscopic cholecystectomy for cholelithiasis, a 45-year-old woman comes to the emergency department because of persistent episodic epigastric pain for 3 days. The pain radiates to her back, occurs randomly throughout the day, and is associated with nausea and vomiting. Each episode lasts 30 minutes to one hour. Antacids do not improve her symptoms. She has hypertension and fibromyalgia. She has smoked 1–2 packs of cigarettes daily for the past 10 years and drinks 4 cans of beer every week. She takes lisinopril and pregabalin. She appears uncomfortable. Her temperature is 37°C (98.6° F), pulse is 84/min, respirations are 14/min, and blood pressure is 127/85 mm Hg. Abdominal examination shows tenderness to palpation in the upper quadrants without rebound or guarding. Bowel sounds are normal. The incisions are clean, dry, and intact. Serum studies show:
AST 80 U/L
ALT 95 U/L
Alkaline phosphatase 213 U/L
Bilirubin, total 1.3 mg/dL
Direct 0.7 mg/dL
Amylase 52 U/L
Abdominal ultrasonography shows dilation of the common bile duct and no gallstones. Which of the following is the most appropriate next step in management?
- A. Counseling on alcohol cessation
- B. Endoscopic retrograde cholangiopancreatography (Correct Answer)
- C. Proton pump inhibitor therapy
- D. CT scan of the abdomen
- E. Reassurance and follow-up in 4 weeks
Immunosuppression principles Explanation: ***Endoscopic retrograde cholangiopancreatography***
- The patient's symptoms (epigastric pain radiating to the back, nausea, vomiting, elevated liver enzymes, and **common bile duct (CBD) dilation** on ultrasound after cholecystectomy) are highly suggestive of **postcholecystectomy syndrome**, specifically due to a retained or de novo **CBD stone** or **sphincter of Oddi dysfunction**.
- **ERCP** is both diagnostic and therapeutic in this setting, allowing for visualization of the bile ducts, stone extraction (if present), or sphincterotomy.
*Counseling on alcohol cessation*
- While **alcohol cessation** is beneficial for overall health, especially with a history of alcohol use, it is not the most immediate or appropriate next step for the acute and severe symptoms presented.
- The patient's symptoms are more indicative of a **biliary obstruction** rather than alcohol-related chronic pancreatitis or liver disease, given the acute onset post-surgery.
*Proton pump inhibitor therapy*
- **PPI therapy** is used for acid-related disorders such as GERD or peptic ulcers, which typically present with burning epigastric pain that improves with antacids.
- This patient's pain radiates to the back, is associated with nausea and vomiting, does not improve with antacids, and has abnormal imaging/labs (CBD dilation, elevated liver enzymes), ruling out a simple acid-related issue.
*CT scan of the abdomen*
- An abdominal **CT scan** could provide more detailed imaging but is generally less effective than ERCP for evaluating **biliary duct pathology** and is not therapeutic.
- Given the ultrasound findings of **CBD dilation** and the patient's symptoms, a more invasive but definitive diagnostic and therapeutic procedure is warranted.
*Reassurance and follow-up in 4 weeks*
- The patient is experiencing severe, persistent symptoms with abnormal liver enzymes and imaging findings indicating **biliary obstruction** post-cholecystectomy.
- **Reassurance and delayed follow-up** would be inappropriate and could lead to worsening of her condition, including cholangitis or pancreatitis if left untreated.
Immunosuppression principles US Medical PG Question 7: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Immunosuppression principles Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
Immunosuppression principles US Medical PG Question 8: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
Immunosuppression principles Explanation: ***Surgical debridement***
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
Immunosuppression principles US Medical PG Question 9: A 38-year-old kidney transplant recipient maintained on tacrolimus presents with a 2-week history of progressive confusion, ataxia, and visual disturbances. MRI shows multifocal white matter lesions without mass effect or enhancement. CSF analysis reveals mild pleocytosis with elevated protein. JC virus DNA is detected in CSF by PCR. Serum tacrolimus level is therapeutic at 8 ng/mL. Apply knowledge of this condition to determine the appropriate management strategy.
- A. Significantly reduce or discontinue immunosuppression and provide supportive care (Correct Answer)
- B. Switch from tacrolimus to sirolimus to preserve graft while treating infection
- C. Continue current immunosuppression and administer IVIG therapy
- D. Maintain immunosuppression and start cidofovir antiviral therapy
- E. Reduce tacrolimus by 50% and start high-dose corticosteroids
Immunosuppression principles Explanation: ***Significantly reduce or discontinue immunosuppression and provide supportive care***
- The patient presents with **Progressive Multifocal Leukoencephalopathy (PML)** caused by **JC virus** reactivation; the primary treatment is **immune reconstitution** to allow the body to fight the virus.
- Reducing or stopping agents like **tacrolimus** is critical for survival, even though it carries a high risk of **allograft rejection**.
*Switch from tacrolimus to sirolimus to preserve graft while treating infection*
- While **sirolimus** has some antiproliferative effects, it is still an **immunosuppressant** and will not allow for the aggressive immune recovery needed to halt **JC virus** replication.
- Managing the life-threatening neurological condition takes precedence over **graft preservation** in the acute phase of PML.
*Continue current immunosuppression and administer IVIG therapy*
- Maintaining current levels of **tacrolimus** prevents the T-cell mediated response necessary to clear the **JC virus** from the CNS.
- **IVIG therapy** has not been proven effective in clinical trials for the treatment of PML and does not address the underlying **immunosuppressed state**.
*Maintain immunosuppression and start cidofovir antiviral therapy*
- **Cidofovir** was previously studied for PML, but it has failed to show significant clinical benefit and is associated with severe **nephrotoxicity**.
- Antiviral therapy without addressing the **cellular immune deficiency** is insufficient to treat this opportunistic infection.
*Reduce tacrolimus by 50% and start high-dose corticosteroids*
- Adding **high-dose corticosteroids** is contraindicated as it further suppresses the immune system, potentially accelerating the progression of **PML**.
- Steroids are typically reserved only for patients who develop **Immune Reconstitution Inflammatory Syndrome (IRIS)** after immunosuppression is withdrawn.
Immunosuppression principles US Medical PG Question 10: A 41-year-old heart transplant recipient (5 years post-transplant) on cyclosporine, azathioprine, and prednisone develops progressive dyspnea on exertion. Echocardiogram shows preserved ejection fraction but abnormal diastolic dysfunction. Right heart catheterization reveals elevated filling pressures. Endomyocardial biopsy shows interstitial fibrosis without significant cellular infiltration. Coronary angiography shows diffuse, concentric narrowing of distal vessels. Synthesize these findings to determine the underlying pathophysiology and evaluate management options.
- A. Cardiac allograft vasculopathy requiring consideration for retransplantation evaluation (Correct Answer)
- B. Restrictive cardiomyopathy from previous rejection episodes requiring diuretic therapy
- C. Drug-induced cardiomyopathy from calcineurin inhibitor toxicity requiring switch to mTOR inhibitor
- D. Acute cellular rejection requiring pulse steroids and optimization of immunosuppression
- E. Antibody-mediated rejection requiring plasmapheresis and rituximab therapy
Immunosuppression principles Explanation: ***Cardiac allograft vasculopathy requiring consideration for retransplantation evaluation***
- **Cardiac allograft vasculopathy (CAV)** is the leading cause of late graft failure, characterized by **diffuse, concentric intimal hyperplasia** and narrowing of the distal coronary vessels.
- The presentation of **progressive dyspnea**, diastolic dysfunction, and **interstitial fibrosis** on biopsy—without acute cellular or antibody-mediated rejection—is pathognomonic for advanced CAV, where **retransplantation** remains the definitive surgical option.
*Restrictive cardiomyopathy from previous rejection episodes requiring diuretic therapy*
- While **interstitial fibrosis** can mimic a restrictive phenotype, this option overlooks the specific **angiographic finding** of distal concentric narrowing which points directly to CAV.
- **Diuretic therapy** may provide symptomatic relief for heart failure but does not address the underlying **progressive vasculopathy** and graft failure.
*Drug-induced cardiomyopathy from calcineurin inhibitor toxicity requiring switch to mTOR inhibitor*
- **Cyclosporine** (a calcineurin inhibitor) primarily causes **nephrotoxicity** and hypertension rather than direct cardiomyopathy with concentric vascular narrowing.
- While **mTOR inhibitors** (like Sirolimus) are used to slow the progression of CAV, they do not resolve established diffuse vascular disease with hemodynamic compromise.
*Acute cellular rejection requiring pulse steroids and optimization of immunosuppression*
- **Acute cellular rejection** is excluded by the endomyocardial biopsy, which specifically showed **no significant cellular infiltration**.
- This condition typically occurs earlier in the post-transplant period and would show **lymphocytic infiltration** and myocyte necrosis rather than concentric vessel narrowing.
*Antibody-mediated rejection requiring plasmapheresis and rituximab therapy*
- **Antibody-mediated rejection (AMR)** is characterized by **capillary endothelial injury** and C4d deposition on biopsy, which were not described in this patient.
- AMR typically presents with more acute graft dysfunction rather than the **slowly progressive** course and distal vessel pruning seen in this case.
More Immunosuppression principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.