Thromboembolic complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thromboembolic complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thromboembolic complications US Medical PG Question 1: A 32-year-old woman presents with progressive shortness of breath and a dry cough. She says that her symptoms onset recently after a 12-hour flight. Past medical history is unremarkable. Current medications are oral estrogen/progesterone containing contraceptive pills. Her vital signs include: blood pressure 110/60 mm Hg, pulse 101/min, respiratory rate 22/min, oxygen saturation 88% on room air, and temperature 37.9℃ (100.2℉). Her weight is 94 kg (207.2 lb) and height is 170 cm (5 ft 7 in). On physical examination, she is acrocyanotic. There are significant swelling and warmth over the right calf. There are widespread bilateral rales present. Cardiac auscultation reveals accentuation of the pulmonic component of the second heart sound (P2) and an S3 gallop. Which of the following ventilation/perfusion (V/Q) ratios most likely corresponds to this patient’s condition?
- A. 1.3 (Correct Answer)
- B. 1
- C. 0.8
- D. 0.5
- E. 0.3
Thromboembolic complications Explanation: ***1.3***
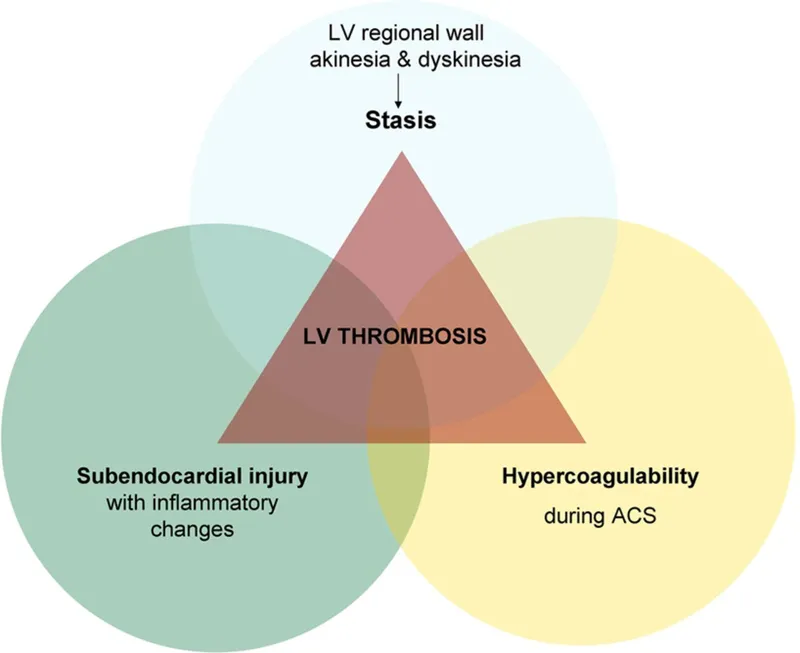
- This value represents an increased V/Q ratio, or **dead space ventilation**, which is characteristic of a **pulmonary embolism (PE)**. In PE, a portion of the lung is ventilated but not perfused due to the embolism blocking blood flow, leading to wasted ventilation.
- The patient's symptoms (sudden onset dyspnea after a long flight, use of oral contraceptives, calf swelling, hypoxia, and accentuated P2) are highly suggestive of a PE, which is the most likely cause of increased V/Q mismatch.
*1*
- A V/Q ratio of 1 indicates **perfect matching** of ventilation and perfusion, which is an ideal state not typically achieved throughout the entire lung, especially in disease.
- This value would not explain the patient's severe **hypoxia** and overall clinical picture of respiratory distress.
*0.8*
- This is the **average normal V/Q ratio** for the lung as a whole, representing slightly more perfusion than ventilation.
- While it's a normal physiological state, it does not account for the significant V/Q mismatch indicated by the patient's severe hypoxemia (SpO2 88%) and clinical symptoms.
*0.5*
- This value represents a **low V/Q ratio**, indicating relatively more perfusion than ventilation, often seen in conditions like **shunt physiology** (e.g., pneumonia, atelectasis, pulmonary edema).
- While the patient has rales and an S3 gallop suggesting potential pulmonary edema or heart failure secondary to increased right heart strain, the primary pathophysiology in PE is increased V/Q due to unperfused but ventilated lung regions.
*0.3*
- This is a severely **low V/Q ratio**, approaching a **shunt**, where blood passes through the lungs without being adequately oxygenated. This is typical of conditions like **severe pneumonia, ARDS, or significant atelectasis**.
- While PE can cause some degree of bronchoconstriction leading to areas of low V/Q, the predominant and most impactful V/Q mismatch in PE is the high V/Q ratio in areas of unperfused lung.
Thromboembolic complications US Medical PG Question 2: A 61-year-old woman presents to the emergency room with left leg pain and swelling. She recently returned to the United States from a trip to India. Her past medical history is notable for osteoarthritis in both hips, lumbar spinal stenosis, and hypertension. She takes lisinopril. Her temperature is 99°F (37.2°C), blood pressure is 140/85 mmHg, pulse is 110/min, and respirations are 24/min. On examination, her left calf is larger than her right calf. A lower extremity ultrasound demonstrates a deep venous thrombosis in the left femoral vein. Results from a complete blood count are within normal limits. She is admitted and started on unfractionated heparin. Seven days later, she presents with a dark erythematous skin lesion on her left thigh and worsening left leg swelling. A lower extremity ultrasound demonstrates a persistent deep venous thrombosis in the left femoral vein as well as a new deep venous thrombosis in the left popliteal vein. Results of a complete blood count are shown below:
Hemoglobin: 13.1 g/dL
Hematocrit: 38%
Leukocyte count: 9,600/mm^3 with normal differential
Platelet count: 74,000/mm^3
A medication with which of the following mechanisms of action is most appropriate to initiate in this patient after stopping the heparin?
- A. Cyclooxygenase inhibitor
- B. Direct thrombin inhibitor (Correct Answer)
- C. Anti-thrombin III activator
- D. Adenosine-diphosphate (ADP) receptor antagonist
- E. Vitamin K epoxide reductase inhibitor
Thromboembolic complications Explanation: **Direct thrombin inhibitor**
- The patient's presentation with a new thrombus, despite being on heparin, and a significantly **decreased platelet count (74,000/mm^3)**, points toward **heparin-induced thrombocytopenia (HIT)**.
- In HIT, heparin must be stopped immediately, and a **non-heparin anticoagulant** like a **direct thrombin inhibitor (e.g., argatroban, bivalirudin)** is the appropriate next step to prevent further thrombosis while avoiding platelet activation.
*Cyclooxygenase inhibitor*
- **Cyclooxygenase inhibitors (e.g., NSAIDs, aspirin)** primarily inhibit platelet aggregation and inflammation but are not the primary treatment for active thrombosis or HIT.
- While effective in preventing arterial clots, they are **insufficient for treating established venous thrombosis**, especially in the context of HIT where platelet activation is a key pathological feature.
*Anti-thrombin III activator*
- **Heparin** itself works by activating antithrombin III, which is precisely the drug that caused the HIT in this patient.
- Administering another antithrombin III activator (e.g., antithrombin III concentrate) would not address the underlying **pathogenesis of HIT**, which involves heparin-dependent antibodies causing platelet activation and thrombosis.
*Adenosine-diphosphate (ADP) receptor antagonist*
- **ADP receptor antagonists (e.g., clopidogrel, ticagrelor)** inhibit platelet aggregation and are used in arterial thrombotic conditions like acute coronary syndrome or stroke prevention.
- While they inhibit platelets, they are **not the first-line treatment for HIT** and its associated venous thrombosis, which requires direct anticoagulation rather than solely antiplatelet therapy.
*Vitamin K epoxide reductase inhibitor*
- **Vitamin K epoxide reductase inhibitors (e.g., warfarin)** are effective oral anticoagulants that inhibit the synthesis of vitamin K-dependent clotting factors.
- However, starting warfarin in acute HIT is **contraindicated** initially because it can lead to a paradoxical prothrombotic state due to a rapid decrease in protein C levels, especially if started before the platelet count has recovered or without overlap with a rapidly acting anticoagulant.
Thromboembolic complications US Medical PG Question 3: A 23-year-old woman with no significant past medical history currently on oral contraceptive pills presents to the emergency department with pleuritic chest pain. She states that it started today. Yesterday she had a trip and returned via plane. Her temperature is 98°F (36.7°C), blood pressure is 117/66 mmHg, pulse is 105/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals tachycardia, a normal S1 and S2, and clear breath sounds. The patient’s lower extremities are non-tender and symmetric. Chest pain is not reproducible with position changes or palpation but is worsened with deep breaths. Which of the following is the most appropriate next test for this patient?
- A. D-dimer
- B. Ultrasound of the lower extremities
- C. Ventilation-perfusion scan
- D. CT angiogram (Correct Answer)
- E. Chest radiograph
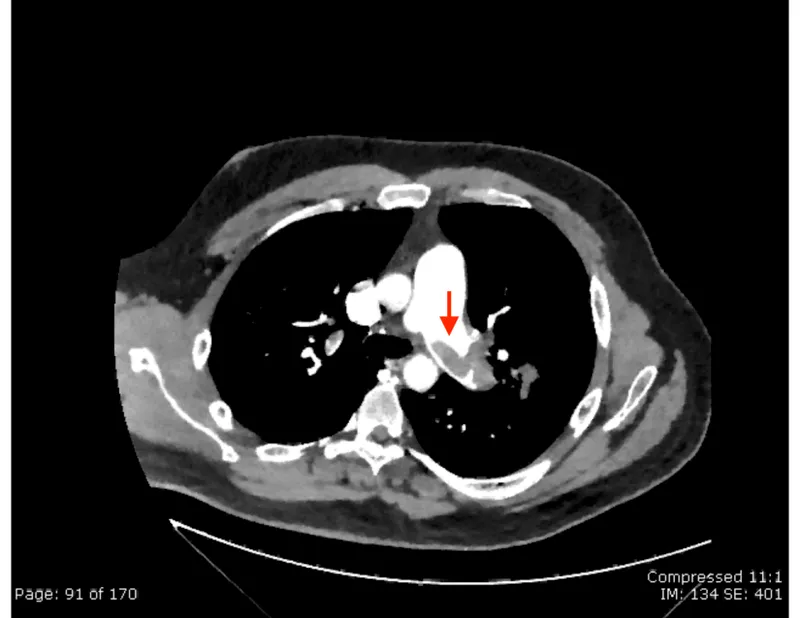
Thromboembolic complications Explanation: ***CT angiogram***
- This patient has **HIGH probability for pulmonary embolism (PE)** based on **Wells criteria**: oral contraceptive use (hypercoagulable state), recent long-haul flight (immobilization), pleuritic chest pain, and tachycardia (pulse 105/min).
- With a **Wells score ≥4**, the appropriate next step is **definitive imaging with CT pulmonary angiography (CTPA)**, which is the **gold standard** for diagnosing PE.
- **D-dimer should be bypassed** in high-probability cases, as a negative result would not adequately rule out PE, and a positive result (expected in high-probability patients) would require CTPA anyway.
- CTPA provides direct visualization of pulmonary arterial thrombi and can also identify alternative diagnoses.
*D-dimer*
- D-dimer is appropriate for **low to moderate probability PE** (Wells score <4) where a negative result can safely rule out PE and avoid unnecessary imaging.
- In this **high-probability case**, D-dimer is likely to be positive regardless, making it an unnecessary intermediate step that delays definitive diagnosis.
- Using D-dimer in high-probability patients can lead to false reassurance if negative or simply confirms the need for CTPA if positive.
*Ultrasound of the lower extremities*
- Lower extremity ultrasound diagnoses **deep vein thrombosis (DVT)**, not PE directly.
- While finding DVT in a patient with suspected PE would support anticoagulation, **absence of DVT does not rule out PE**, as thrombi may have already embolized.
- This would delay appropriate diagnosis and is not the most direct test for suspected PE.
*Ventilation-perfusion scan*
- V/Q scan is reserved for patients with **contraindications to CT contrast** (severe renal insufficiency, contrast allergy) or pregnant patients where radiation exposure should be minimized.
- This young patient has no mentioned contraindications to contrast-enhanced CT.
- V/Q scanning is less specific than CTPA and often yields indeterminate results.
*Chest radiograph*
- Chest X-ray is often **normal in PE** or shows non-specific findings (Westermark sign, Hampton's hump are rare).
- While it may help exclude alternative diagnoses like pneumothorax or pneumonia, it cannot definitively diagnose or rule out PE.
- In a patient with high clinical suspicion for PE, delaying CTPA to obtain a chest X-ray is not optimal management.
Thromboembolic complications US Medical PG Question 4: A 54-year-old woman comes to the physician because of a 6-month history of dull, persistent pain and swelling of her right leg. The pain is worse at the end of the day and is relieved by walking or elevating her feet. Two years ago, she developed acute deep vein thrombosis in her right calf after a long flight, which was treated with anticoagulants for 6 months. Physical examination shows 2+ pitting edema of her right leg. The skin around the right ankle shows a reddish-brown discoloration and multiple telangiectasias. She has dilated varicose veins in the right leg. Which of the following is most likely to establish the diagnosis?
- A. D-dimer assay
- B. Ankle-brachial pressure index
- C. Computerized tomography scan with contrast
- D. Duplex ultrasonography (Correct Answer)
- E. Nerve conduction studies
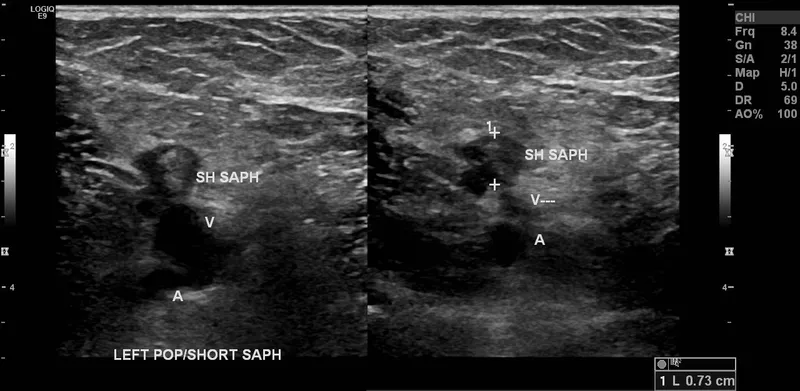
Thromboembolic complications Explanation: ***Duplex ultrasonography***
- **Duplex ultrasonography** is the gold standard for evaluating **venous insufficiency**, which is strongly suggested by the patient's history of **deep vein thrombosis (DVT)**, **chronic leg pain**, **pitting edema**, **stasis dermatitis** (reddish-brown discoloration), and **varicose veins**.
- This non-invasive imaging technique allows visualization of vein structure, blood flow, and valve function, helping to identify **venous reflux** or **obstruction**.
*D-dimer assay*
- A **D-dimer assay** is primarily used to **rule out acute DVT** or pulmonary embolism.
- While D-dimer levels may be elevated in chronic venous disease, it is **not specific** enough to establish a diagnosis of chronic venous insufficiency or its cause.
*Ankle-brachial pressure index*
- The **ankle-brachial pressure index (ABPI)** is used to diagnose **peripheral artery disease (PAD)** by comparing blood pressure in the ankle to the arm.
- This patient's symptoms are more consistent with **venous disease** rather than arterial insufficiency.
*Computerized tomography scan with contrast*
- A **CT scan with contrast** can visualize vascular structures but is **less sensitive and specific** for diagnosing venous insufficiency compared to duplex ultrasonography.
- It also involves **radiation exposure** and **contrast dye risks**, making it a less suitable initial diagnostic tool for this condition.
*Nerve conduction studies*
- **Nerve conduction studies** are used to diagnose **neuropathies** and conditions affecting the peripheral nerves and are not relevant for evaluating vascular issues.
- The patient's symptoms clearly point to a **vascular problem**, not a neurological one.
Thromboembolic complications US Medical PG Question 5: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
Thromboembolic complications Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
Thromboembolic complications US Medical PG Question 6: A mother brings her 6-year-old daughter in to the pediatrician’s clinic for a wellness visit. The mother has a history of von Willebrand’s disease (vWD) and is concerned that her daughter may be affected as well. The mother tells you that she has noticed that her daughter bruises very easily, and her bruises typically are visible for a longer period of time than those of her brother. She denies any personal history of blood clots in her past, but she says that her mother has had to be treated for pulmonary embolism in the recent past. Her birth history is significant for preeclampsia, preterm birth at 32 weeks, a NICU stay of two and a half weeks, and retinopathy of prematurity. She currently eats a diet full of green vegetables, fruits, and french fries. Her vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 106/54 mm Hg; heart rate, 111/min; and respiratory, rate 23/min. On physical examination, her pulses are bounding, complexion is pale, scattered bruises throughout all extremities that are specifically scattered around the knees and elbows. After ordering a coagulation panel, which of the following would one expect to see in the lab panel of a patient with vWD?
- A. Elevated platelet count
- B. Prolonged PT
- C. Normal bleeding time
- D. Decreased factor IX
- E. Prolonged PTT (Correct Answer)
Thromboembolic complications Explanation: ***Prolonged PTT***
- **Von Willebrand factor (vWF)** stabilizes **Factor VIII**, and in vWD, reduced vWF levels lead to lower Factor VIII activity, which is reflected as a **prolonged PTT**.
- The coagulation cascade components associated with PTT (intrinsic and common pathways) are affected due to the impaired function or deficiency of vWF.
*Elevated platelet count*
- **Platelet count** is typically **normal** in vWD, as the disorder primarily affects platelet function and adhesion, not platelet production.
- Thrombocytosis is not characteristic of vWD and would suggest other primary hematologic conditions.
*Prolonged PT*
- The **prothrombin time (PT)** measures the extrinsic and common pathways of coagulation, which are typically **unaffected** in vWD.
- PT prolongation would suggest deficiencies in factors VII, X, V, or prothrombin.
*Normal bleeding time*
- **Bleeding time** is typically **prolonged** in vWD because vWF is crucial for platelet adhesion to the subendothelium and platelet plug formation.
- A normal bleeding time would argue against a platelet function disorder like vWD.
*Decreased factor IX*
- **Factor IX** deficiency is associated with **Hemophilia B**, a separate X-linked coagulopathy, and is not directly affected in vWD.
- While vWD involves coagulation factor deficiencies, the primary factor stabilized by vWF is Factor VIII, not Factor IX.
Thromboembolic complications US Medical PG Question 7: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
Thromboembolic complications Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
Thromboembolic complications US Medical PG Question 8: A 55-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of alcohol abuse and is currently attending alcoholics anonymous with little success. He is currently drinking roughly 1L of hard alcohol every day and does not take his disulfiram anymore. Which of the following findings is most likely to also be found in this patient?
- A. Dysdiadochokinesia (Correct Answer)
- B. Microcytic anemia
- C. Constipation
- D. Decreased CNS NMDA activity
- E. Increased transketolase activity
Thromboembolic complications Explanation: ***Dysdiadochokinesia***
- Chronic **alcohol abuse** can lead to cerebellar degeneration, a condition characterized by damage to the **cerebellum**.
- **Dysdiadochokinesia**, the impaired ability to perform rapidly alternating movements, is a classic sign of **cerebellar dysfunction**.
*Microcytic anemia*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** due to folate deficiency, or less commonly, iron deficiency anemia from gastrointestinal bleeding.
- **Microcytic anemia** is usually associated with **iron deficiency** (often due to chronic blood loss) or **thalassemia**, neither of which are suggested here.
*Constipation*
- While various factors can cause constipation, **chronic alcohol abuse** is more commonly associated with **diarrhea** due to alterations in gut motility and malabsorption.
- Constipation is not a direct or prominent feature of **alcoholism**.
*Decreased CNS NMDA activity*
- **Chronic alcohol abuse** leads to an **upregulation of NMDA receptors** in the brain as a compensatory mechanism against alcohol's inhibitory effects on the central nervous system.
- When alcohol consumption ceases, this upregulated NMDA activity contributes to the **excitatory symptoms of alcohol withdrawal**, such as seizures and delirium tremens.
*Increased transketolase activity*
- **Transketolase activity** is usually **decreased** in chronic alcoholics due to **thiamine deficiency**, as thiamine (vitamin B1) is a critical cofactor for this enzyme.
- A **decrease** in transketolase activity is a key diagnostic indicator for thiamine deficiency, which contributes to conditions like **Wernicke-Korsakoff syndrome**.
Thromboembolic complications US Medical PG Question 9: A 27-year-old man is brought to the emergency department by ambulance following a motor vehicle accident 1 hour prior. He appears agitated. His blood pressure is 85/60 mm Hg, the pulse is 110/min, and the respiratory rate is 19/min. Physical examination shows bruising of the left flank and fracture of the left lower thoracic bones. Strict bed rest and monitoring with intravenous fluids is initiated. Urinalysis shows numerous RBCs. A contrast-enhanced CT scan shows normal enhancement of the right kidney. The left renal artery is only visible in the proximal section with a small amount of extravasated blood around the left kidney. The left kidney shows no enhancement. Imaging of the spleen shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Immediate surgical exploration (Correct Answer)
- B. Observation with delayed repair
- C. Conservative management
- D. Renal artery embolization
- E. Renal artery embolization with delayed nephrectomy
Thromboembolic complications Explanation: ***Immediate surgical exploration***
- The patient presents with signs of **hemodynamic instability** (BP 85/60, pulse 110/min, agitation) and imaging findings consistent with **left renal artery avulsion** and devascularization (no enhancement of the left kidney, visible only proximally, extravasated blood). These findings necessitate immediate surgical intervention to control hemorrhage and assess kidney viability.
- The goal is to revascularize the kidney if possible, perform a nephrectomy if the kidney is unsalvageable, and manage hemorrhage to stabilize the patient.
*Observation with delayed repair*
- This approach is typically reserved for **hemodynamically stable** patients with renal injuries, especially lower-grade injuries that do not involve complete vessel avulsion or ongoing significant hemorrhage.
- Delaying intervention in a hemodynamically unstable patient with a presumed renal artery avulsion can lead to further decompensation, irreversible kidney damage, and increased mortality.
*Conservative management*
- **Conservative management** is appropriate for hemodynamically stable patients with minor renal injuries, such as contusions or small lacerations, or for very selected cases of more severe injuries that have spontaneously tamponaded and are not causing significant clinical compromise.
- The patient's **hemodynamic instability** and direct evidence of renal artery injury preclude conservative management in this case.
*Renal artery embolization*
- **Renal artery embolization** is a highly effective, minimally invasive technique for controlling bleeding from renal injuries. However, it is primarily indicated for **hemodynamically stable patients** with contained hemorrhage or specific pseudoaneurysms/AV fistulas.
- In a hemodynamically unstable patient with a complete renal artery avulsion and non-perfused kidney, embolization is unlikely to revascularize the kidney and may even hinder subsequent surgical repair if revascularization is deemed possible. Furthermore, it might not be sufficient to control diffuse or extensive bleeding associated with avulsion.
*Renal artery embolization with delayed nephrectomy*
- While embolization can precede nephrectomy in certain scenarios for better hemorrhage control, it is not the primary immediate step in a **hemodynamically unstable** patient with renal artery avulsion and a non-enhancing kidney.
- The primary concern is the patient's instability, which requires immediate surgical control, and delaying nephrectomy after embolization often isn't feasible if the kidney is completely devascularized and the patient is unstable. The decision for nephrectomy typically occurs during the initial surgical exploration.
Thromboembolic complications US Medical PG Question 10: A 35-year-old man suffers severe polytrauma including traumatic brain injury (GCS 6), pulmonary contusions, splenic laceration, and open femur fracture. He undergoes damage control surgery with splenectomy and external fixation. On ICU day 4, he develops worsening hypoxemia (PaO2/FiO2 ratio 150), bilateral infiltrates on chest X-ray, normal pulmonary capillary wedge pressure, petechiae, and altered mental status beyond his head injury. Fat globules are noted in urine. Platelet count drops from 245,000 to 89,000/μL. Evaluate the diagnosis and management priority.
- A. Sepsis from missed abdominal injury; return to OR for re-exploration
- B. Transfusion-related acute lung injury; diuresis and transfusion avoidance
- C. Disseminated intravascular coagulation; aggressive factor replacement
- D. Acute respiratory distress syndrome; increase PEEP and lung-protective ventilation
- E. Fat embolism syndrome; supportive care and definitive fracture fixation when stable (Correct Answer)
Thromboembolic complications Explanation: ***Fat embolism syndrome; supportive care and definitive fracture fixation when stable***
- This patient presents with the classic **Gurd’s triad**: respiratory distress (hypoxemia, infiltrates), neurologic symptoms (altered mental status), and a **petechial rash** 24–72 hours after a **long bone fracture**.
- Laboratory findings of **thrombocytopenia** and **fat globules in urine** further confirm the diagnosis, with management prioritizing **supportive care** and stabilization before definitive orthopedic intervention.
*Sepsis from missed abdominal injury; return to OR for re-exploration*
- While common in trauma, sepsis typically presents with **hemodynamic instability**, fever, or leukocytosis, rather than the specific petechial rash seen here.
- Re-exploration is unnecessary unless there is evidence of **peritonitis** or a clear source of infection that cannot be managed medically.
*Transfusion-related acute lung injury; diuresis and transfusion avoidance*
- **TRALI** presents with acute hypoxemia and bilateral infiltrates shortly after blood administration, but does not explain the **petechiae** or fat globules.
- Unlike circulatory overload, TRALI management focuses on **supportive ventilation** rather than aggressive **diuresis**, which might worsen the patient's condition.
*Disseminated intravascular coagulation; aggressive factor replacement*
- **DIC** can cause a drop in platelets and widespread bleeding, but it is usually a consumptive process resulting in prolonged **PT/PTT** and elevated **D-dimer**.
- While fat embolism can trigger secondary coagulopathy, the primary pathology here is the embolism itself, and factor replacement is only indicated for active, severe hemorrhage.
*Acute respiratory distress syndrome; increase PEEP and lung-protective ventilation*
- While the P/F ratio of 150 meets criteria for **ARDS**, this diagnosis alone fails to account for the **petechial rash** and systemic fat globules.
- Lung-protective ventilation is part of the treatment for fat embolism, but the question asks for the most comprehensive diagnosis and management strategy for all clinical features.
More Thromboembolic complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.