Systemic inflammatory response syndrome US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systemic inflammatory response syndrome. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systemic inflammatory response syndrome US Medical PG Question 1: A 25-year-old man presents to the emergency department after a motor vehicle accident. He was the unrestrained front seat driver in a head on collision. The patient is unresponsive and his medical history is unknown. His temperature is 99.5°F (37.5°C), blood pressure is 67/38 mmHg, pulse is 190/min, respirations are 33/min, and oxygen saturation is 98% on room air. The patient is started on IV fluids, blood products, and norepinephrine. A FAST exam is performed and a pelvic binder is placed. One hour later, his temperature is 98.3°F (36.8°C), blood pressure is 119/66 mmHg, pulse is 110/min, respirations are 15/min, and oxygen saturation is 97% on room air. The patient is currently responsive. Management of the patient's pelvic fracture is scheduled by the orthopedic service. While the patient is waiting in the emergency department he suddenly complains of feeling hot, aches, and a headache. The patient's temperature is currently 101°F (38.3°C). He has not been given any pain medications and his past medical history is still unknown. Which of the following is the most likely diagnosis?
- A. Acute hemolytic transfusion reaction
- B. Febrile non-hemolytic transfusion reaction (Correct Answer)
- C. Sympathetic response to pain
- D. Minor blood group incompatibility
- E. Leukoagglutination reaction
Systemic inflammatory response syndrome Explanation: ***Febrile non-hemolytic transfusion reaction***
- This reaction is characterized by a **fever** and other constitutional symptoms (chills, headache, malaise) developing **within 4 hours of transfusion**, without evidence of hemolysis. The patient's symptoms and temperature rise after blood product administration fit this description.
- It is typically caused by antibodies in the recipient's plasma reacting with **leukocyte antigens** present on donor white blood cells or by **cytokines** released from donor leukocytes during storage.
*Acute hemolytic transfusion reaction*
- This reaction typically presents with more severe symptoms such as **hypotension**, **hemoglobinuria**, flank pain, and diffuse bleeding, indicating widespread intravascular hemolysis due to **ABO incompatibility**.
- Although the patient received blood products, his symptoms (feeling hot, aches, headache, mild fever) are not indicative of the severe, life-threatening nature of an acute hemolytic reaction.
*Sympathetic response to pain*
- While pain can cause a sympathetic response (tachycardia, hypertension), it typically does **not cause a fever** as seen in this patient.
- The patient's initial presentation included signs of shock, and after resuscitation, his vital signs normalized before the new symptoms appeared, suggesting a new process rather than ongoing pain alone.
*Minor blood group incompatibility*
- Reactions to minor blood group incompatibilities are usually **milder and delayed** compared to ABO incompatibilities.
- They often involve **extravascular hemolysis**, which might not present with the acute febrile reaction seen here, and are less common a cause of immediate febrile reactions.
*Leukoagglutination reaction*
- This is an older term for what is now often considered a type of **febrile non-hemolytic transfusion reaction (FNHTR)** caused by recipient antibodies to donor leukocyte antigens leading to leukocyte clumping.
- While related to FNHTR, the term "febrile non-hemolytic transfusion reaction" is the more encompassing and appropriate diagnosis given the typical symptom complex of fever, chills, and headache.
Systemic inflammatory response syndrome US Medical PG Question 2: A 28-year-old research assistant is brought to the emergency department for severe chemical burns 30 minutes after accidentally spilling hydrochloric acid on himself. The burns cover both hands and forearms. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 20/min, and blood pressure is 108/82 mm Hg. Initial stabilization and resuscitation is begun, including respiratory support, fluid resuscitation, and cardiovascular stabilization. The burned skin is irrigated with saline water to remove the chemical agent. Which of the following is the most appropriate method to verify adequate fluid infusion in this patient?
- A. The Parkland formula
- B. Blood pressure
- C. Pulmonary capillary wedge pressure
- D. Heart rate
- E. Urinary output (Correct Answer)
Systemic inflammatory response syndrome Explanation: ***Urinary output***
- Maintaining a specific **urinary output** (e.g., adult with major burns: 0.5-1.0 mL/kg/hr or 30-50 mL/hr) is the most reliable clinical indicator of adequate fluid resuscitation in burn patients.
- This ensures sufficient end-organ perfusion and avoids both under-resuscitation (leading to shock and organ damage) and over-resuscitation (risk of compartment syndrome and pulmonary edema).
*The Parkland formula*
- The **Parkland formula** is used to *calculate* the initial fluid volume needed, but it does not *verify* the adequacy of the infusion once started.
- This formula provides a starting point for fluid administration, which then needs to be adjusted based on the patient's response.
*Blood pressure*
- **Blood pressure** can be misleading in burn patients; it may remain deceptively normal due to compensatory mechanisms even with significant fluid deficits.
- It is a late indicator of hypovolemic shock, and relying solely on it can lead to under-resuscitation.
*Pulmonary capillary wedge pressure*
- **Pulmonary capillary wedge pressure (PCWP)** requires invasive monitoring via a pulmonary artery catheter, which is rarely indicated for routine fluid management in burn patients due to its invasiveness and associated risks.
- Less invasive and equally effective methods, like urinary output, are preferred for monitoring resuscitation.
*Heart rate*
- **Heart rate** is a sensitive but non-specific indicator of fluid status; it can be elevated due to pain, anxiety, or infection, not solely hypovolemia.
- While a decreasing heart rate can indicate improved fluid status, it is not as reliable or direct an indicator of end-organ perfusion as urinary output.
Systemic inflammatory response syndrome US Medical PG Question 3: A researcher is studying the interactions between foreign antigens and human immune cells. She has isolated a line of lymphocytes that is known to bind antigen-presenting cells. From this cell line, she has isolated a cell surface protein that binds to class I major histocompatibility complex molecules. The continued activation, proliferation and survival of this specific cell line requires which of the following signaling molecules?
- A. Interleukin 1
- B. Interleukin 4
- C. Interleukin 2 (Correct Answer)
- D. Interleukin 8
- E. Interleukin 6
Systemic inflammatory response syndrome Explanation: ***Interleukin 2***
- The description of the lymphocyte binding the **constant portion of MHC class I** and requiring a signaling molecule for activation, proliferation, and survival points to a **T cell**.
- **Interleukin-2 (IL-2)** is a crucial cytokine for the proliferation, differentiation, and survival of T lymphocytes, acting in an autocrine or paracrine fashion after T cell activation.
*Interleukin 1*
- **Interleukin-1 (IL-1)** is primarily involved in inflammation and fever, produced by macrophages and other innate immune cells.
- While it can act as a costimulator for T cells, it is not the primary cytokine required for their sustained proliferation and survival after initial activation.
*Interleukin 4*
- **Interleukin-4 (IL-4)** is a key cytokine in humoral immunity, promoting B cell proliferation and differentiation, and inducing IgE class switching.
- It also plays a role in the differentiation of naive T cells into **Th2 cells**, but it is not the main cytokine for general T cell proliferation and survival.
*Interleukin 8*
- **Interleukin-8 (IL-8)**, also known as CXCL8, is a chemokine primarily responsible for attracting and activating neutrophils to sites of infection or inflammation.
- It does not have a direct role in the sustained proliferation and survival of activated lymphocytes.
*Interleukin 6*
- **Interleukin-6 (IL-6)** is a pleiotropic cytokine involved in acute phase reactions, hematopoiesis, and the immune response, particularly B cell differentiation and antibody production.
- Although it can influence T cell responses, it is not the primary growth factor for activated T lymphocytes as IL-2 is.
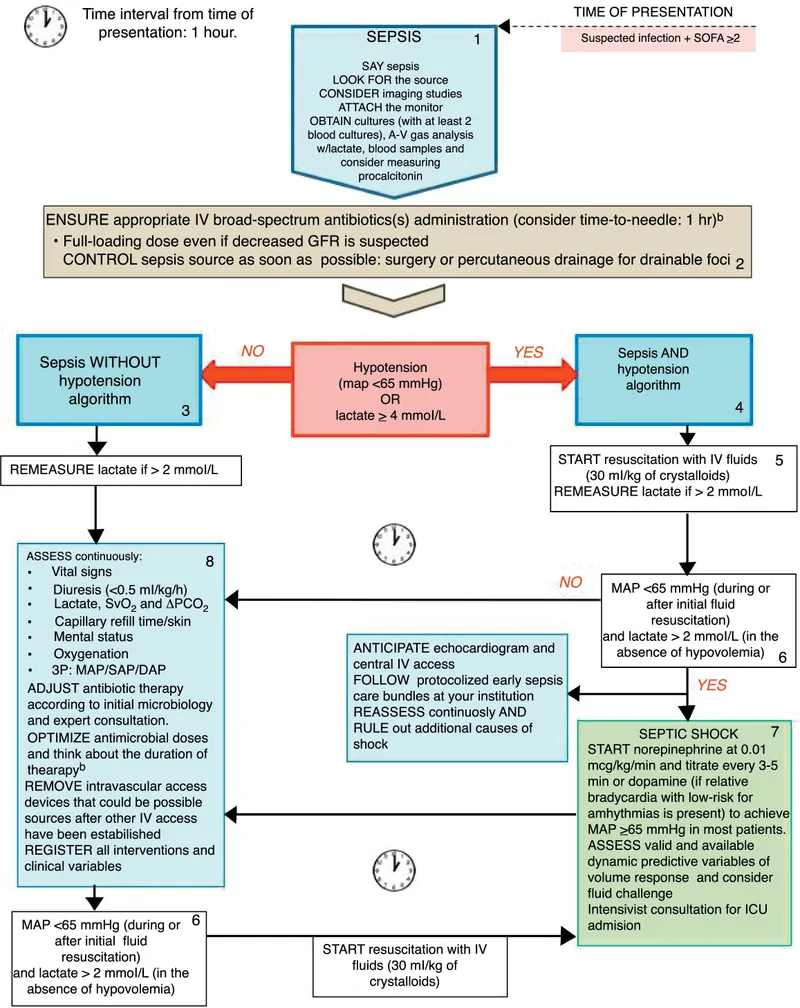
Systemic inflammatory response syndrome US Medical PG Question 4: A 53-year-old diabetic man with cellulitis of the right lower limb presents to the emergency department because of symptoms of fever and chills. His pulse is 122/min, the blood pressure is 76/50 mm Hg, the respirations are 26/min, and the temperature is 40.0°C (104.0°F). His urine output is < 0.5mL/kg/h. He has warm peripheral extremities. The hemodynamic status of the patient is not improving in spite of the initiation of adequate fluid resuscitation. He is admitted to the hospital. Which of the following is the most likely laboratory profile?
- A. WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L
- B. WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L
- C. WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L (Correct Answer)
- D. WBC count: 6670/mm3; low CVP; blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L
- E. WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L
Systemic inflammatory response syndrome Explanation: ***WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L***
- This profile aligns with **septic shock** driven by gram-negative bacteria, presenting with **tachycardia**, **hypotension**, **fever**, and **poor urine output** despite fluid resuscitation.
- A **high WBC count** (leukocytosis), **low CVP** (due to vasodilation and relative hypovolemia), **gram-negative bacteremia** (common in severe sepsis), and **elevated lactate** (indicating tissue hypoperfusion) are characteristic findings.
*WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L*
- While most components suggest sepsis (WBC count and low CVP), a **lactate level of 0.9 mmol/L** is within the normal range, contradicting the severe hypoperfusion and shock observed in the patient.
- The patient's presentation with **hypotension** unresponsive to fluids and **oliguria** strongly indicates significant tissue hypoperfusion, which would typically result in a higher lactate.
*WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L*
- A **WBC count of 1234/mm3 (leukopenia)** is an atypical response for severe infection and sepsis; often, sepsis presents with leukocytosis.
- A **high CVP** indicates fluid overload or cardiac dysfunction, which is not consistent with the initial low blood pressure and the need for fluid resuscitation seen in distributive shock.
*WBC count: 6670/mm3; low central venous pressure (CVP); blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L*
- A **WBC count of 6670/mm3** is within the normal range and does not reflect an adequate inflammatory response to severe infection and shock.
- A **normal lactate level (1.1 mmol/L)** does not support the clinical picture of shock and tissue hypoperfusion despite the presence of gram-positive bacteremia.
*WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L*
- A **WBC count of 8880/mm3** is normal, which is unlikely in a severe sepsis presentation.
- A **high CVP** is not consistent with the distributive shock state where there is often relative hypovolemia and vasodilation leading to low CVP.
Systemic inflammatory response syndrome US Medical PG Question 5: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Systemic inflammatory response syndrome Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Systemic inflammatory response syndrome US Medical PG Question 6: A 12-year-old boy admitted to the intensive care unit 1 day ago for severe pneumonia suddenly develops hypotension. He was started on empiric antibiotics and his blood culture reports are pending. According to the nurse, the patient was doing fine until his blood pressure suddenly dropped. Vital signs include: blood pressure is 88/58 mm Hg, temperature is 39.4°C (103.0°F), pulse is 120/min, and respiratory rate is 24/min. His limbs feel warm. The resident physician decides to start him on intravenous vasopressors, as the blood pressure is not responding to intravenous fluids. The on-call intensivist suspects shock due to a bacterial toxin. What is the primary mechanism responsible for the pathogenesis of this patient's condition?
- A. Inactivation of elongation factor (EF) 2
- B. Inhibition of GABA and glycine
- C. Inhibition of acetylcholine release
- D. Release of tumor necrosis factor (TNF) (Correct Answer)
- E. Degradation of lecithin in cell membranes
Systemic inflammatory response syndrome Explanation: ***Release of tumor necrosis factor (TNF)***
- The patient's presentation with **warm limbs** and **hypotension** despite fluid resuscitation in the setting of severe pneumonia is highly suggestive of **septic shock**.
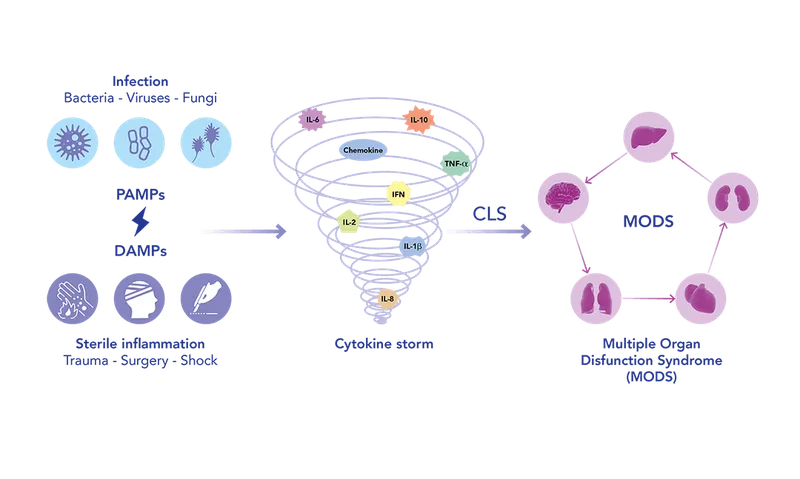
- **Bacterial toxins**, particularly **endotoxins** from gram-negative bacteria or **exotoxins** like superantigens, trigger a massive **inflammatory response** by stimulating immune cells to release pro-inflammatory cytokines such as **TNF-α**, IL-1, and IL-6, leading to systemic vasodilation and capillary leak.
*Inactivation of elongation factor (EF) 2*
- This is the mechanism of action of **diphtheria toxin** and **exotoxin A** from *Pseudomonas aeruginosa*.
- While these toxins can cause severe systemic illness, their primary role is not typically the induction of septic shock characterized by widespread vasodilation and warm extremities.
*Inhibition of GABA and glycine*
- This mechanism is characteristic of **tetanus toxin**, which prevents the release of inhibitory neurotransmitters and leads to spastic paralysis.
- This is not consistent with the patient's presentation of septic shock.
*Inhibition of acetylcholine release*
- This is the mechanism of action of **botulinum toxin**, which causes flaccid paralysis by blocking acetylcholine release at the neuromuscular junction.
- This effect is not associated with the pathogenesis of septic shock.
*Degradation of lecithin in cell membranes*
- This mechanism is associated with **alpha toxin** of *Clostridium perfringens* (lecithinase), which causes gas gangrene and hemolysis.
- While this toxin contributes to tissue damage in certain infections, it is not the primary mechanism behind the systemic inflammatory response and vasodilation seen in septic shock.
Systemic inflammatory response syndrome US Medical PG Question 7: A 61-year-old man with hypertension and hyperlipidemia comes to the physician for a 4-month history of recurrent episodes of retrosternal chest pain, shortness of breath, dizziness, and nausea. The episodes usually start after physical activity and subside within minutes of resting. He has smoked one pack of cigarettes daily for 40 years. He is 176 cm (5 ft 9 in) tall and weighs 95 kg (209 lb); BMI is 30 kg/m2. His blood pressure is 160/100 mm Hg. Coronary angiography shows an atherosclerotic lesion with stenosis of the left anterior descending artery. Compared to normal healthy coronary arteries, increased levels of platelet-derived growth factor (PDGF) are found in this lesion. Which of the following is the most likely effect of this factor?
- A. Calcification of the atherosclerotic plaque core
- B. Invasion of T-cells through the disrupted endothelium
- C. Increased expression of vascular cell-adhesion molecules
- D. Ingestion of cholesterol by mature monocytes
- E. Intimal migration of smooth muscle cells (Correct Answer)
Systemic inflammatory response syndrome Explanation: ***Intimal migration of smooth muscle cells***
- **PDGF** is a potent **mitogen** and **chemotactic factor** for smooth muscle cells, promoting their migration from the tunica media into the intima during atherogenesis.
- This migration is a crucial step in the formation of the **fibrous cap**, contributing to plaque growth and stability.
*Calcification of the atherosclerotic plaque core*
- While calcification does occur in advanced atherosclerotic plaques, it is primarily driven by mechanisms involving **osteoblast-like differentiation** of vascular cells and deposition of **calcium phosphate**, not directly by PDGF.
- PDGF's primary role is in **cellular proliferation** and **migration**, particularly of smooth muscle cells.
*Invasion of T-cells through the disrupted endothelium*
- **T-cell invasion** into the arterial wall is an important inflammatory process in atherosclerosis, but it is primarily mediated by **chemokines** like MCP-1 and adhesion molecules, not directly by PDGF.
- PDGF typically acts on mesenchymal cells (like smooth muscle cells and fibroblasts) rather than immune cells in this context.
*Increased expression of vascular cell-adhesion molecules*
- **Expression of adhesion molecules** (e.g., VCAM-1, ICAM-1) is crucial for the recruitment of inflammatory cells, but this process is mainly driven by **pro-inflammatory cytokines** like TNF-α and IL-1, not PDGF.
- While there might be indirect effects, PDGF's direct role is not primarily in promoting adhesion molecule expression.
*Ingestion of cholesterol by mature monocytes*
- **Ingestion of cholesterol** by **macrophages** (which mature from monocytes) leads to the formation of **foam cells**, a hallmark of early atherosclerosis.
- This process is largely driven by oxidized LDL uptake, often facilitated by scavenger receptors, rather than directly by PDGF.
Systemic inflammatory response syndrome US Medical PG Question 8: Every time your neighbor in the adjacent apartment flushes the toilet, the water in your shower becomes very hot, causing you to jump out of the way of the water stream. After this has occurred for several months, you note that you reflexively jump back from the water directly after the sound of the flushing toilet but before the water temperature changes. Which of the following situations is the most similar to the conditioning process detailed above?
- A. You consistently check the slots of pay telephones as you have previously found change left there
- B. White coat syndrome (patient anxiety evoked at the sight of a white lab coat) (Correct Answer)
- C. A young child elects to not throw a temper tantrum to avoid being grounded by his parents
- D. A mouse repeatedly presses a red button to avoid receiving an electric shock
- E. You now sleep through the noise of the train running past your apartment that kept you up 1 year ago
Systemic inflammatory response syndrome Explanation: ***White coat syndrome (patient anxiety evoked at the sight of a white lab coat)***
- This is an example of **classical conditioning**, where a neutral stimulus (**white coat**) becomes associated with an unconditioned stimulus (pain/anxiety-inducing medical procedures), leading to a conditioned response (anxiety).
- Similarly, the **sound of the flush** (neutral stimulus) became associated with the **hot water** (unconditioned stimulus), leading to a **reflexive jump** (conditioned response).
*You consistently check the slots of pay telephones as you have previously found change left there*
- This scenario represents **operant conditioning**, specifically **positive reinforcement**, where checking the slot is reinforced by the reward of finding change.
- The behavior is strengthened by the **consequence** that follows it, rather than an association between two stimuli.
*A young child elects to not throw a temper tantrum to avoid being grounded by his parents*
- This is an example of **negative punishment** in **operant conditioning**, where the child avoids a negative consequence (being grounded) by refraining from a specific behavior (tantrum).
- The focus is on the **consequences** of an action influencing future behavior, not an involuntary, learned association between stimuli.
*A mouse repeatedly presses a red button to avoid receiving an electric shock*
- This describes **operant conditioning**, specifically **negative reinforcement**, where the mouse performs an action (**pressing the button**) to remove an aversive stimulus (**electric shock**).
- It involves a voluntary action to escape or avoid an unpleasant event, differing from the involuntary, anticipatory reflex seen in classical conditioning.
*You now sleep through the noise of the train running past your apartment that kept you up 1 year ago*
- This is an example of **habituation**, a non-associative learning process where an organism decreases its response to a stimulus after repeated exposure.
- The organism learns to **ignore** an irrelevant or non-threatening stimulus, rather than forming a new association between two stimuli.
Systemic inflammatory response syndrome US Medical PG Question 9: A 40-year-old woman who works as a secretary presents to your office complaining of new pain and numbness in both of her hands. For the past few weeks, the sensation has occurred after long days of typing, but it now occasionally wakes her up from sleep. You do not note any deformities of her wrists or hands, but you are able to reproduce pain and numbness in the first three and a half digits by tapping the wrist. What is the best initial treatment for this patient's complaint?
- A. Local steroid injections
- B. Carpal tunnel release surgery
- C. Splinting (Correct Answer)
- D. A trial of gabapentin
- E. Short-acting benzodiazepines
Systemic inflammatory response syndrome Explanation: ***Splinting***
- This patient's symptoms are highly suggestive of **carpal tunnel syndrome (CTS)**, given the **pain and numbness** in the distribution of the **median nerve** (first three and a half digits) that is exacerbated by repetitive wrist movements (typing) and reproduced by **Tinel's sign** (tapping the wrist).
- **Splinting** the wrist, especially at night, is the **first-line conservative treatment** for CTS, as it keeps the wrist in a neutral position, reducing pressure on the median nerve.
*Local steroid injections*
- While local steroid injections can provide **temporary relief** for CTS, they are typically considered if splinting and activity modification are unsuccessful.
- They are not the **initial treatment** of choice due to potential side effects and the less invasive nature of splinting.
*Carpal tunnel release surgery*
- **Carpal tunnel release surgery** is a definitive treatment for CTS but is reserved for cases that fail conservative management, show signs of **thenar atrophy**, or have objective evidence of severe nerve compression on **electromyography/nerve conduction studies**.
- It is an **invasive procedure** and not appropriate as a first-line intervention.
*A trial of gabapentin*
- **Gabapentin** is an anticonvulsant often used to treat **neuropathic pain**, but it is generally reserved for more generalized or refractory neuropathic conditions.
- It is not the primary treatment for localized nerve compression like CTS when less invasive and more targeted options are available.
*Short-acting benzodiazepines*
- **Benzodiazepines** are primarily used for anxiety, insomnia, or muscle spasms and have **no direct role** in treating the underlying nerve compression or symptoms of carpal tunnel syndrome.
- They do not address the pathology and carry risks of dependency.
Systemic inflammatory response syndrome US Medical PG Question 10: A 23-year-old woman presents to the emergency department after being found unresponsive by her friends. The patient is an IV drug user and her friends came over and found her passed out in her room. The patient presented to the emergency department 2 days ago after being involved in a bar fight where she broke her nose and had it treated and packed with gauze. Her temperature is 99.3°F (37.4°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 24/min, and oxygen saturation is 97% on room air. Physical exam is notable for an obtunded woman with nasal packing and EKG tags from her last hospital stay, as well as a purpuric rash on her arms and legs. Her arms have track marks on them and blisters. Which of the following is the best next step in management?
- A. Removal of nasal packing (Correct Answer)
- B. Urine toxicology screen and empiric naloxone
- C. Nafcillin
- D. Vancomycin
- E. Norepinephrine
Systemic inflammatory response syndrome Explanation: ***Removal of nasal packing***
- This patient presents with classic **toxic shock syndrome (TSS)** caused by nasal packing following her nasal fracture repair 2 days ago.
- Key diagnostic features include: **purpuric rash** (diffuse macular erythroderma with petechiae), hypotension (90/48 mmHg), tachycardia (150/min), fever, and altered mental status.
- TSS is caused by **Staphylococcus aureus** toxin production, with nasal packing being a well-known risk factor.
- **Immediate removal of the nasal packing** (the source of infection) is the critical first step, followed by fluid resuscitation and empiric anti-staphylococcal antibiotics.
*Urine toxicology screen and empiric naloxone*
- While the patient is an IV drug user, opioid overdose does **not** explain the **purpuric rash**, which is the key diagnostic finding.
- Opioid overdose typically presents with **respiratory depression** (low respiratory rate), not tachypnea (24/min) with normal oxygen saturation.
- The clinical picture is dominated by TSS, not drug toxicity.
*Nafcillin*
- While **nafcillin** (anti-staphylococcal antibiotic) will be needed for TSS treatment, the **first step** is removal of the source (nasal packing).
- Source control takes precedence over antibiotics in foreign body-associated infections.
*Vancomycin*
- Similar to nafcillin, **vancomycin** is appropriate for empiric TSS coverage (especially for MRSA), but must come **after** removal of nasal packing.
- Antibiotics without source control will not adequately treat TSS.
*Norepinephrine*
- While the patient is hypotensive and may eventually require vasopressor support, the **immediate priority** is removing the infectious source.
- TSS-induced shock should be managed with aggressive fluid resuscitation first, and vasopressors are added if fluid resuscitation fails.
More Systemic inflammatory response syndrome US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.