Surgical site infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical site infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical site infections US Medical PG Question 1: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
Surgical site infections Explanation: ***Incentive spirometry***
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
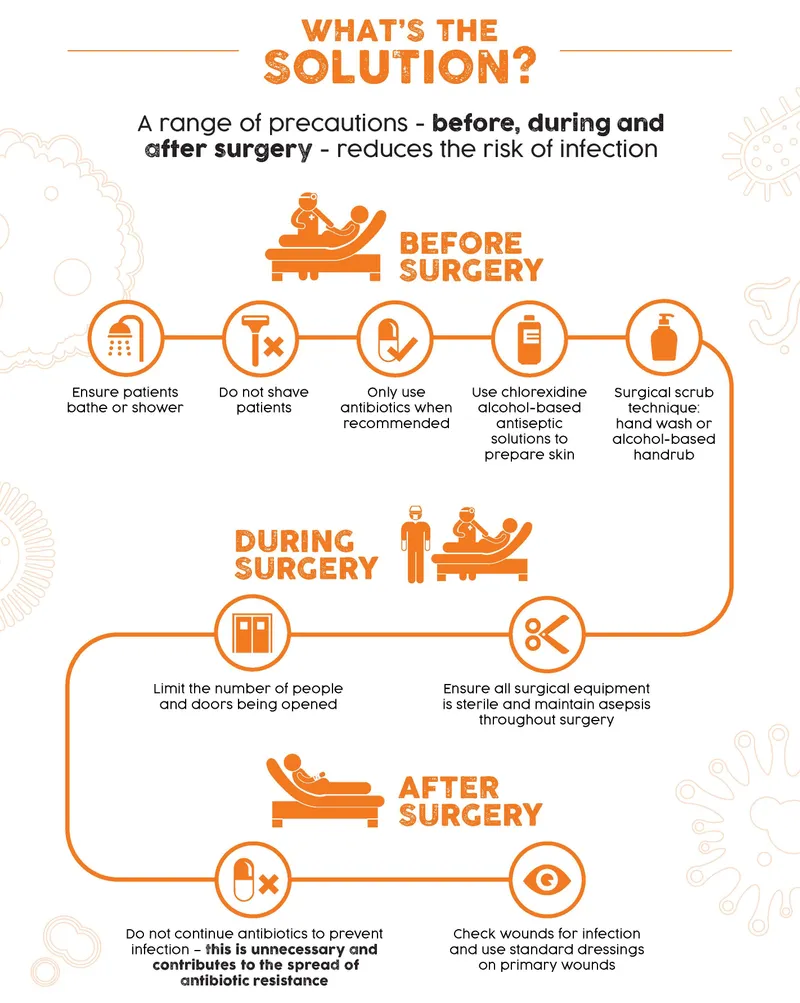
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
Surgical site infections US Medical PG Question 2: Two hours after admission to the intensive care unit, a 56-year-old man with necrotizing pancreatitis develops profound hypotension. His blood pressure is 80/50 mm Hg and he is started on vasopressors. A central venous access line is placed. Which of the following is most likely to decrease the risk of complications from this procedure?
- A. Placement of the central venous line in the femoral vein
- B. Replacement of the central venous line every 7-10 days
- C. Initiation of anticoagulation after placement
- D. Preparation of the skin with chlorhexidine and alcohol (Correct Answer)
- E. Initiation of periprocedural systemic antibiotic prophylaxis
Surgical site infections Explanation: ***Preparation of the skin with chlorhexidine and alcohol***
- **Chlorhexidine** with alcohol is the most effective skin antiseptic for preventing **catheter-related bloodstream infections (CRBSIs)** by significantly reducing skin microbial counts.
- Proper skin preparation is a cornerstone of preventing **infectious complications** associated with central venous catheter insertion.
*Placement of the central venous line in the femoral vein*
- The femoral site is generally associated with a **higher risk of infection** and **deep venous thrombosis** compared to subclavian or internal jugular sites in adult patients.
- Femoral access is often reserved for situations where other sites are inaccessible or contraindicated, due to its **less favorable complication profile**.
*Replacement of the central venous line every 7-10 days*
- Routine replacement of central venous lines at fixed intervals, without clinical indication, has **not been shown to reduce infection rates**.
- This practice can actually **increase the risk** of mechanical complications and introduce new opportunities for infection with each procedure.
*Initiation of anticoagulation after placement*
- Routine systemic **anticoagulation** after central venous line placement is generally **not recommended** due to an increased risk of **bleeding complications**.
- Anticoagulation is typically reserved for specific indications such as documented **catheter-related thrombosis**.
*Initiation of periprocedural systemic antibiotic prophylaxis*
- Routine **systemic antibiotic prophylaxis** is **not recommended** for central venous catheter insertion as it promotes **antibiotic resistance** without significantly reducing CRBSIs.
- Strict adherence to **aseptic technique** and proper skin antisepsis are more effective for preventing infections.
Surgical site infections US Medical PG Question 3: A 62-year-old man comes to the physician because of an oozing skin ulceration on his foot for 1 week. He has a history of type 2 diabetes mellitus and does not adhere to his medication regimen. Physical exam shows purulent discharge from an ulcer on the dorsum of his left foot. Pinprick sensation is decreased bilaterally to the level of the mid-tibia. A culture of the wound grows beta-hemolytic, coagulase-positive cocci in clusters. The causal organism most likely produces which of the following virulence factors?
- A. Exotoxin A
- B. M protein
- C. P fimbriae
- D. IgA protease
- E. Protein A (Correct Answer)
Surgical site infections Explanation: ***Protein A***
- The culture finding of **beta-hemolytic, coagulase-positive cocci in clusters** is characteristic of ***Staphylococcus aureus***.
- ***Staphylococcus aureus*** produces **Protein A**, which binds to the Fc region of IgG, preventing opsonization and phagocytosis, thereby hindering the immune response.
*Exotoxin A*
- **Exotoxin A** is a virulence factor primarily produced by ***Pseudomonas aeruginosa***, particularly associated with deep tissue infections and sepsis.
- It functions as an **ADP-ribosylating toxin** that inhibits protein synthesis, but it is not characteristic of the organism isolated in this patient.
*M protein*
- **M protein** is a key virulence factor of ***Streptococcus pyogenes*** (Group A Streptococcus), responsible for preventing phagocytosis and promoting adhesion.
- ***S. pyogenes*** is beta-hemolytic but typically grows in **chains**, not clusters, and is **coagulase-negative**.
*P fimbriae*
- **P fimbriae** (pyelonephritis-associated pilus) are virulence factors predominantly found in uropathogenic strains of ***Escherichia coli***, mediating adhesion to uroepithelial cells.
- These fimbriae are associated with urinary tract infections, not typically with skin ulcers from **Gram-positive cocci in clusters**.
*IgA protease*
- **IgA protease** is a virulence factor produced by several pathogenic bacteria such as ***Neisseria gonorrhoeae***, ***Haemophilus influenzae***, and ***Streptococcus pneumoniae***.
- It cleaves IgA at hinge regions, allowing the bacteria to evade mucosal immunity, but it is not a primary virulence factor of ***Staphylococcus aureus*** or commonly associated with skin ulcers.
Surgical site infections US Medical PG Question 4: Five days after being admitted to the hospital for a scald wound, a 2-year-old boy is found to have a temperature of 40.2°C (104.4°F). He does not have difficulty breathing, cough, or painful urination. He initially presented one hour after spilling a pot of boiling water on his torso while his mother was cooking dinner. He was admitted for fluid resuscitation, nutritional support, pain management, and wound care, and he was progressing well until today. He has no other medical conditions. Other than analgesia during this hospital stay, he does not take any medications. He appears uncomfortable but not in acute distress. His pulse is 150/min, respirations are 41/min, and blood pressure is 90/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Examination shows uneven, asymmetrical scalding covering his anterior torso in arrow-like patterns with surrounding erythema and purulent discharge. The remainder of the examination shows no abnormalities. His hemoglobin is 13.4 g/dL, platelet count is 200,000/mm3, and leukocyte count is 13,900/mm3. Which of the following is the most appropriate initial pharmacological treatment for this patient?
- A. Vancomycin and metronidazole
- B. Amoxicillin/clavulanic acid and ceftriaxone
- C. Ampicillin/sulbactam and daptomycin
- D. Vancomycin and cefepime (Correct Answer)
- E. Piperacillin/tazobactam and cefepime
Surgical site infections Explanation: ***Vancomycin and cefepime***
- The patient presents with classic signs of **burn wound infection**, including fever, purulent discharge, and a rapid pulse, necessitating broad-spectrum antibiotic coverage.
- **Vancomycin** provides excellent coverage against **MRSA (methicillin-resistant *Staphylococcus aureus*)**, a common pathogen in burn infections, while **cefepime** covers **gram-negative bacteria**, including *Pseudomonas aeruginosa*, which is also frequently implicated.
*Vancomycin and metronidazole*
- While vancomycin covers gram-positive bacteria like **MRSA**, **metronidazole** primarily targets **anaerobic bacteria**, which are less common as primary pathogens in burn wound infections.
- This combination lacks adequate coverage for crucial gram-negative bacteria such as *Pseudomonas aeruginosa*.
*Amoxicillin/clavulanic acid and ceftriaxone*
- This combination provides coverage against some common community-acquired pathogens but is insufficient for the broad-spectrum needs of a severe **hospital-acquired burn infection**.
- It lacks reliable coverage for **MRSA** and *Pseudomonas aeruginosa*, which are critical in this setting.
*Ampicillin/sulbactam and daptomycin*
- **Ampicillin/sulbactam** covers some gram-positive and gram-negative bacteria but would not reliably cover **MRSA** or *Pseudomonas aeruginosa*.
- **Daptomycin** is effective against gram-positive bacteria, including **MRSA**, but does not cover gram-negative pathogens, leaving a significant gap in treatment.
*Piperacillin/tazobactam and cefepime*
- Both **piperacillin/tazobactam** and **cefepime** are excellent broad-spectrum antibiotics covering gram-negative pathogens, including *Pseudomonas aeruginosa*, but are largely redundant in this combination.
- This regimen lacks specific coverage for **MRSA**, which is a significant concern in nosocomial burn wound infections.
Surgical site infections US Medical PG Question 5: A 16-year-old boy presents to the emergency department after a skateboarding accident. He fell on a broken bottle and received a 4 cm wound on the dorsal aspect of his left hand. His vitals are stable and he was evaluated by the surgeon on call who determined that suturing was not required. After several weeks the wound has almost completely healed (see image). Which of the following is the correct description of this patient's wound before healing?
- A. Incised wound (Correct Answer)
- B. Abrasion
- C. Laceration
- D. Avulsion
- E. Puncture
Surgical site infections Explanation: ***Incised wound***
- An **incised wound** is caused by a sharp object, such as a broken bottle, resulting in a clean, straight cut with well-defined edges and minimal tissue damage.
- The characteristics of the injury (sharp object mechanism, 4 cm linear wound) and the clinical decision that suturing was not required suggest a relatively clean incised wound with edges that could approximate well.
- Incised wounds typically heal with **fine linear scars** as shown in the image, especially when the edges are well-approximated.
*Abrasion*
- An abrasion is a **superficial wound** caused by friction or scraping, leading to removal of the epidermis and sometimes the superficial dermis.
- This mechanism does not match the described injury from a broken bottle, and abrasions produce broad, shallow wounds rather than deep linear cuts.
- Abrasions heal with minimal scarring and would not produce the linear scar pattern shown.
*Laceration*
- A laceration is a wound with **irregular, torn edges** typically caused by blunt force trauma or crushing injury.
- While broken glass can sometimes cause lacerations, the description of a clean "4 cm wound" from falling on a broken bottle more strongly suggests a sharp cutting mechanism rather than tearing.
- Lacerations have jagged edges with more tissue damage and typically require debridement or careful closure.
*Avulsion*
- An **avulsion** involves forcible tearing away of tissue, often resulting in significant tissue loss with irregular, gaping wounds.
- This injury pattern is much more severe than described and would typically require complex surgical management, including possible skin grafting.
- The mechanism (falling on broken glass) and the relatively straightforward healing do not support an avulsion injury.
*Puncture*
- A puncture wound is caused by a **pointed object** penetrating the skin, creating a small entry hole with depth greater than width.
- The description of a "4 cm wound" indicates a linear length, not a deep narrow penetration typical of puncture wounds.
- Puncture wounds carry high infection risk and would not produce the linear scar pattern shown in the image.
Surgical site infections US Medical PG Question 6: A 63-year-old female recovering from a total shoulder arthroplasty completed 6 days ago presents complaining of joint pain in her repaired shoulder. Temperature is 39 degrees Celsius. Physical examination demonstrates erythema and significant tenderness around the incision site. Wound cultures reveal Gram-positive cocci that are resistant to nafcillin. Which of the following organisms is the most likely cause of this patient's condition?
- A. Streptococcus pyogenes
- B. Escherichia coli
- C. Streptococcus viridans
- D. Staphylococcus epidermidis
- E. Staphylococcus aureus (Correct Answer)
Surgical site infections Explanation: ***Staphylococcus aureus***
- The combination of **post-surgical infection**, **erythema**, and fever with **Gram-positive cocci** that are **nafcillin-resistant** is highly indicative of **Methicillin-Resistant Staphylococcus aureus (MRSA)**.
- *S. aureus* is a common cause of **surgical site infections**, and its resistance to nafcillin implies it is MRSA, a significant clinical concern for its difficulty in treatment.
*Streptococcus pyogenes*
- While *S. pyogenes* is a Gram-positive coccus that can cause skin and soft tissue infections, it is typically **susceptible to penicillin** and related antibiotics like nafcillin, unlike the organism described.
- It is more commonly associated with **streptococcal pharyngitis** or **cellulitis**, and while it can cause severe disease, its resistance profile doesn't match the clinical picture.
*Escherichia coli*
- *E. coli* is a **Gram-negative rod**, not a Gram-positive coccus.
- It is a common cause of **urinary tract infections** and **gastrointestinal infections**, making it an unlikely pathogen for a post-surgical joint infection unless contaminated from a visceral source.
*Streptococcus viridans*
- **Viridans streptococci** are Gram-positive cocci but are typically associated with **endocarditis** or dental infections, especially after poor dental hygiene or procedures.
- They are usually **susceptible to penicillin** and do not typically exhibit nafcillin resistance as the primary feature in a post-arthroplasty infection.
*Staphylococcus epidermidis*
- *S. epidermidis* is a **coagulase-negative Staphylococcus** known for forming **biofilms on prosthetic devices**, leading to chronic, low-grade infections.
- While it can be nafcillin-resistant, the **acute presentation** with fever and significant inflammation suggests a more virulent pathogen like *S. aureus*, as *S. epidermidis* infections are typically indolent.
Surgical site infections US Medical PG Question 7: A 67-year-old man is brought to the emergency department because of severe dyspnea and orthopnea for 6 hours. He has a history of congestive heart disease and an ejection fraction of 40%. The medical history is otherwise unremarkable. He appears confused. At the hospital, his blood pressure is 165/110 mm Hg, the pulse is 135/min, the respirations are 48/min, and the temperature is 36.2°C (97.2°F). Crackles are heard at both lung bases. There is pitting edema from the midtibia to the ankle bilaterally. The patient is intubated and admitted to the critical care unit for mechanical ventilation and treatment. Intravenous morphine, diuretics, and nitroglycerine are initiated. Which of the following is the most effective method to prevent nosocomial infection in this patient?
- A. Nasogastric tube insertion
- B. Suprapubic catheter insertion
- C. Daily oropharynx decontamination with antiseptic agent (Correct Answer)
- D. Daily urinary catheter irrigation with antimicrobial agent
- E. Condom catheter placement
Surgical site infections Explanation: ***Daily oropharynx decontamination with antiseptic agent***
- **Oropharyngeal decontamination** helps reduce the bacterial load in the oral cavity, which is crucial for preventing **ventilator-associated pneumonia (VAP)** in intubated patients.
- Regular cleaning with an antiseptic agent disrupts the formation of **biofilms** and the aspiration of pathogenic bacteria into the lower respiratory tract.
*Nasogastric tube insertion*
- While a nasogastric tube can be important for nutrition and medication delivery, it does not directly prevent **nosocomial infections** and can even be a source of infection if not properly managed.
- It does not address the primary risk of pneumonia or other infections related to intubation and critical illness.
*Suprapubic catheter insertion*
- A suprapubic catheter is used for drainage of the bladder, but it is an invasive procedure with its own risks of **urinary tract infections (UTIs)** and is not indicated for preventing nosocomial infections in this patient's primary presentation.
- It is not a standard method to prevent the most common nosocomial infections in an intubated patient in the ICU.
*Daily urinary catheter irrigation with antimicrobial agent*
- Irrigating a urinary catheter daily with an antimicrobial agent is **not recommended** as a routine practice to prevent **catheter-associated urinary tract infections (CAUTIs)**.
- Such irrigation can disrupt the natural flora and potentially lead to **antimicrobial resistance** or further infection by promoting the growth of resistant organisms.
*Condom catheter placement*
- A condom catheter is a non-invasive external device used for urinary incontinence in males, but it's generally **less effective** than indwelling catheters for critical care patients requiring precise fluid output monitoring.
- It does not address the risk of **VAP**, which is a major concern for intubated patients, and may not be feasible or adequate for all bedridden patients in the ICU.
Surgical site infections US Medical PG Question 8: A 37-year-old-woman presents to the emergency room with complaints of fever and abdominal pain. Her blood pressure is 130/74 mmHg, pulse is 98/min, temperature is 101.5°F (38.6°C), and respirations are 23/min. The patient reports that she had a laparoscopic cholecystectomy 4 days ago but has otherwise been healthy. She is visiting her family from Nebraska and just arrived this morning from a 12-hour drive. Physical examination revealed erythema and white discharge from abdominal incisions and tenderness upon palpations at the right upper quadrant. What is the most probable cause of the patient’s fever?
- A. Pulmonary atelectasis
- B. Residual gallstones
- C. Urinary tract infection
- D. Wound infection (Correct Answer)
- E. Pulmonary embolism
Surgical site infections Explanation: ***Wound infection***
- The presence of **erythema**, **white discharge from abdominal incisions**, and **fever** 4 days post-laparoscopic cholecystectomy strongly indicates a surgical site infection.
- This is a common complication after surgery, especially with visible signs of local inflammation and purulent discharge.
*Pulmonary atelectasis*
- **Atelectasis** typically presents within **24-48 hours post-op** and usually resolves spontaneously.
- While it can cause fever, the prominent local wound signs and the timing (4 days post-op) make it less likely to be the primary cause of fever.
*Residual gallstones*
- **Residual gallstones** would typically present with symptoms resembling acute cholecystitis or cholangitis, such as **right upper quadrant pain**, **jaundice**, or **elevated liver enzymes**, without direct signs of wound infection.
- These do not account for the **erythema and discharge from the incision sites**.
*Urinary tract infection*
- A **urinary tract infection (UTI)** would present with **dysuria**, **frequency**, **urgency**, or **suprapubic pain**, and would not explain the local wound findings.
- While surgery can increase the risk of nosocomial UTIs, the clinical presentation is primarily focused on the surgical site.
*Pulmonary embolism*
- A **pulmonary embolism (PE)** would likely cause **dyspnea**, **tachycardia**, **hypoxia**, and **pleuritic chest pain**, which are not reported in this case.
- Though prolonged immobility (e.g., long drive) is a risk factor, the specific local signs of infection are not consistent with PE.
Surgical site infections US Medical PG Question 9: A 43-year-old man is brought to the emergency department 40 minutes after falling off a 10-foot ladder. He has severe pain and swelling of his right ankle and is unable to walk. He did not lose consciousness after the fall. He has no nausea. He appears uncomfortable. His temperature is 37°C (98.6°F), pulse is 98/min, respirations are 16/min, and blood pressure is 110/80 mm Hg. He is alert and oriented to person, place, and time. Examination shows multiple abrasions over both lower extremities. There is swelling and tenderness of the right ankle; range of motion is limited by pain. The remainder of the examination shows no abnormalities. An x-ray of the ankle shows an extra-articular calcaneal fracture. Intravenous analgesia is administered. Which of the following is the most appropriate next step in the management of this patient?
- A. Short leg splint and orthopedic consultation
- B. Broad-spectrum antibiotic therapy
- C. MRI of the right ankle
- D. Open reduction and internal fixation
- E. X-ray of the spine (Correct Answer)
Surgical site infections Explanation: ***X-ray of the spine***
- A **high-energy calcaneal fracture** (especially from a fall from height) is often associated with other injuries, particularly to the **spine**, due to axial loading.
- Approximately **10% of calcaneal fractures** are associated with **lumbar spine compression fractures**, making imaging of the spine an essential next step to rule out this potentially serious concomitant injury.
*Short leg splint and orthopedic consultation*
- While a **short leg splint** is appropriate for initial immobilization and pain control of the ankle fracture, and **orthopedic consultation** is necessary, these steps do not address the immediate need to exclude other critical injuries like spinal fractures in high-impact trauma.
- This option represents definitive management of the ankle rather than comprehensive early trauma assessment in a high-risk patient.
*Broad-spectrum antibiotic therapy*
- **Antibiotic therapy** is primarily indicated for **open fractures** to prevent infection, or in cases of significant soft tissue injury with high contamination risk; the provided information describes an extra-articular fracture with abrasions, but not explicitly an open fracture requiring immediate broad-spectrum antibiotics.
- The focus should first be on skeletal integrity elsewhere and definitive fracture management rather than presumptive infection prevention unless an open fracture is confirmed.
*MRI of the right ankle*
- While an **MRI** can provide detailed imaging of soft tissues, ligaments, and cartilage, and may be useful later for surgical planning or to assess subtle injuries, a plain **X-ray has already confirmed a calcaneal fracture**.
- The immediate priority after a high-energy trauma is to rule out other significant, potentially disabling or life-threatening bony injuries, particularly to the spine, rather than further detailed imaging of the already-identified ankle fracture.
*Open reduction and internal fixation*
- **Open reduction and internal fixation (ORIF)** is a surgical procedure for definitive management of certain fractures; however, it is not the **immediate next step** in the emergency department for initial patient assessment following trauma.
- Before surgical intervention, a comprehensive assessment to rule out other injuries (especially spinal fractures) and to thoroughly plan the specific surgical approach is required.
Surgical site infections US Medical PG Question 10: A 35-year-old man suffers severe polytrauma including traumatic brain injury (GCS 6), pulmonary contusions, splenic laceration, and open femur fracture. He undergoes damage control surgery with splenectomy and external fixation. On ICU day 4, he develops worsening hypoxemia (PaO2/FiO2 ratio 150), bilateral infiltrates on chest X-ray, normal pulmonary capillary wedge pressure, petechiae, and altered mental status beyond his head injury. Fat globules are noted in urine. Platelet count drops from 245,000 to 89,000/μL. Evaluate the diagnosis and management priority.
- A. Sepsis from missed abdominal injury; return to OR for re-exploration
- B. Transfusion-related acute lung injury; diuresis and transfusion avoidance
- C. Disseminated intravascular coagulation; aggressive factor replacement
- D. Acute respiratory distress syndrome; increase PEEP and lung-protective ventilation
- E. Fat embolism syndrome; supportive care and definitive fracture fixation when stable (Correct Answer)
Surgical site infections Explanation: ***Fat embolism syndrome; supportive care and definitive fracture fixation when stable***
- This patient presents with the classic **Gurd’s triad**: respiratory distress (hypoxemia, infiltrates), neurologic symptoms (altered mental status), and a **petechial rash** 24–72 hours after a **long bone fracture**.
- Laboratory findings of **thrombocytopenia** and **fat globules in urine** further confirm the diagnosis, with management prioritizing **supportive care** and stabilization before definitive orthopedic intervention.
*Sepsis from missed abdominal injury; return to OR for re-exploration*
- While common in trauma, sepsis typically presents with **hemodynamic instability**, fever, or leukocytosis, rather than the specific petechial rash seen here.
- Re-exploration is unnecessary unless there is evidence of **peritonitis** or a clear source of infection that cannot be managed medically.
*Transfusion-related acute lung injury; diuresis and transfusion avoidance*
- **TRALI** presents with acute hypoxemia and bilateral infiltrates shortly after blood administration, but does not explain the **petechiae** or fat globules.
- Unlike circulatory overload, TRALI management focuses on **supportive ventilation** rather than aggressive **diuresis**, which might worsen the patient's condition.
*Disseminated intravascular coagulation; aggressive factor replacement*
- **DIC** can cause a drop in platelets and widespread bleeding, but it is usually a consumptive process resulting in prolonged **PT/PTT** and elevated **D-dimer**.
- While fat embolism can trigger secondary coagulopathy, the primary pathology here is the embolism itself, and factor replacement is only indicated for active, severe hemorrhage.
*Acute respiratory distress syndrome; increase PEEP and lung-protective ventilation*
- While the P/F ratio of 150 meets criteria for **ARDS**, this diagnosis alone fails to account for the **petechial rash** and systemic fat globules.
- Lung-protective ventilation is part of the treatment for fat embolism, but the question asks for the most comprehensive diagnosis and management strategy for all clinical features.
More Surgical site infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.